How To Engage Your Whole Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Stroke Of Insight That Nobody Wants
This is Dr. Jill Bolte Taylor. She’s a neuroanatomist, who, at the age of 37 (when she was a post-doctoral fellow at Harvard Medical School), had what she refers to as her “stroke of insight”.
That is to say, she had a massive stroke, and after a major brain surgery to remove a clot the size of a golf ball, she spent the next 8 years re-learning to do everything.
Whereas previously she’d been busy mapping the brain to determine how cells communicate with each other, now she was busy mapping whether socks or shoes should go on first. Needless to say, she got an insight into neuroplasticity that few people would hope for.
What does she want us to know?
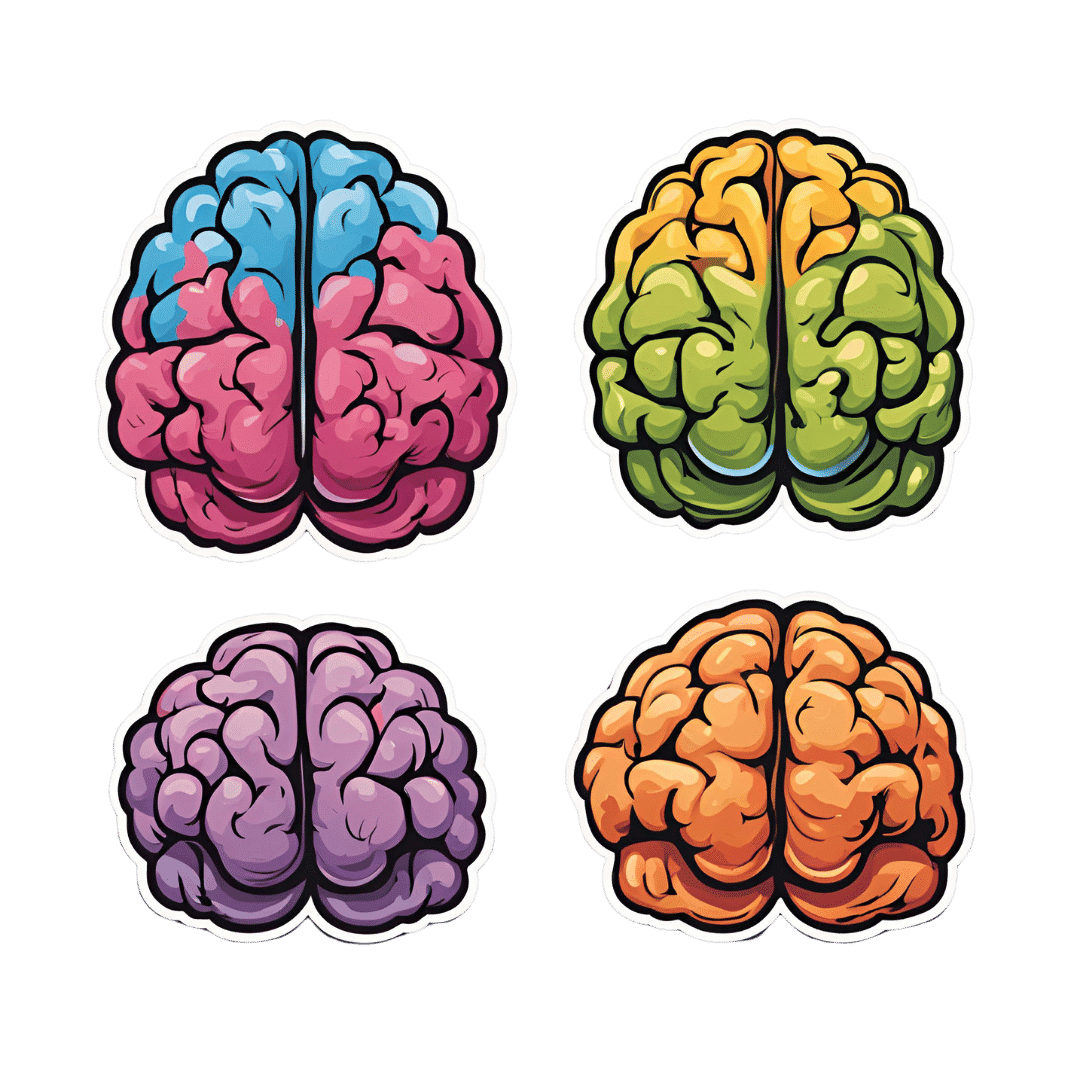
Dr. Taylor (now once again a successful scientist, lecturer, and author) advocates for “whole brain living”, which involves not taking parts of our brain for granted.
About those parts…
Dr. Taylor wants us to pay attention to all the parts regardless of size, ranging from the two hemispheres, all the way down to the billions of brain cells, and yet even further, to the “trillions of molecular geniuses”—because each brain cell is itself reliant on countless molecules of the many neurochemicals that make up our brain.
For a quick refresher on some of the key players in that latter category, see our Neurotransmitter Cheatsheet 😎
When it comes to the hemispheres, there has historically been a popular belief that these re divided into:
- The right brain: emotional, imaginative, creative, fluid feeling
- The left brain: intellectual, analytical, calculating, crystal thinking
…which is not true, anatomically speaking, because there are cells on both sides doing their part of both of these broad categories of brain processes.
However, Dr. Taylor found, while one hemisphere of her brain was much more damaged than the other, that nevertheless she could recover some functions more quickly than others, which, once she was able to resume her career, inspired her model of four distinct ways of cogitating that can be switched-between and played with or against each other:
Meet The Four Characters Inside Your Brain
Why this matters
As she was re-learning everything, the way forward was not quick or easy, and she also didn’t know where she was going, because for obvious reasons, she couldn’t remember, much less plan.
Looking backwards after her eventual full recovery, she noted a lot of things that she needed during that recovery, some of which she got and some of which she didn’t.
Most notably for her, she needed the right kind of support that would allow all four of the above “characters” as she puts it, to thrive and grow. And, when we say “grow” here we mean that literally, because of growing new brain cells to replace the lost ones (as well as the simple ongoing process of slowly replacing brain cells).
For more on growing new brain cells, by the way, see:
How To Grow New Brain Cells (At Any Age)
In order to achieve this in all of the required brain areas (i.e., and all of the required brain functions), she also wants us to know… drumroll please…
When to STFU
Specifically, the ability to silence parts of our brain that while useful in general, aren’t necessarily being useful right now. Since it’s very difficult to actively achieve a negative when it comes to brain-stuff (don’t think of an elephant), this means scheduling time for other parts of our brain to be louder. And that includes:
- scheduling time to feel (emotionally)
- scheduling time to feel (gut feelings)
- scheduling time to feel (kinesthetically)
…amongst others.
Note: those three are presented in that order, from least basic to most basic. And why? Because, clever beings that we are, we typically start from a position that’s not remotely basic, such as “overthinking”, for example. So, there’s a wind-down through thinking just the right amount, thinking through simpler concepts, feeling, noticing one’s feelings, noticing noticing one’s feelings, all the way down to what, kinesthetically, are we actually physically feeling.
❝It is interesting to note that although our limbic system fucntions throughout our lifetime, it does not mature. As a result, when our emotional “buttons” are pushed, we retain the ability to react to incoming stimulation as though we were a two-year-old, even when we are adults.❞
~ Dr. Jill Taylor
Of course, sometimes the above is not useful, which is why the ability to switch between brain modes is a very important and useful skill to develop.
And how do we do that? By practising. Which is something that it’s necessary to take up consciously, and pursue consistently. When children are at school, there are (hopefully, ideally) curricula set out to ensure they engage and train all parts of their brain. As adults, this does not tend to get the same amount of focus.
“Children’s brains are still developing”—indeed, and so are adult brains:
The Brain As A Work-In-Progress
Dr. Taylor had the uncommon experience of having to, in many ways, neurologically speaking, redo childhood. And having had a second run at it, she developed an appreciation of the process that most of us didn’t necessarily get when doing childhood just the once.
In other words: take the time to feel stuff; take the time to quiet down your chatty mind, take the time engage your senses, and take it seriously! Really notice, as though for the first time, what the texture of your carpet is like. Really notice, as though for the first time, what it feels like to swallow some water. Really notice, as though for the first time, what it feels like to experience joy—or sadness, or comfort, or anger, or peace. Exercise your imagination. Make some art (it doesn’t have to win awards; it just has to light up your brain!). Make music (again, it’s about wiring your brain in your body, not about outdoing Mozart in composition and/or performance). Make changes! Make your brain work in the ways it’s not in the habit of doing.
If you need a little help switching off parts of your brain that are being too active, so that you can better exercise other parts of your brain that might otherwise have been neglected, you might want to try:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Avoiding Anemia (More Than Just “Get More Iron”)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Iron Dilemma: Factors To Consider
Anemia affects around 10% of American seniors, and that number jumps to 34–39% if there’s a comorbidity such as diabetes, hypertension, or hypercholesterolemia, which in turn climbs with increasing age or with other chronic conditions:
So, what can we do about it?
Get iron yes, but how?
We’d be remiss not to say: yes, do of course make sure you get plenty of iron.
Most people know that red meats, which are terrible for the heart and for cancer risk, are good sources of iron.
Well, good insofar as they provide plenty of it! They’re bad for other reasons.
❝Studies consistently show that consumption of red meat has been contributory to a multitude of chronic conditions such as diabetes, CVD, and malignancies.
There are various emerging reasons that strengthen this link-from the basic constituents of red meat like the heme iron component, the metabolic reactions that take place after consumption, and finally to the methods used to cook it.
The causative links show that even occasional use raises the risk of T2DM.❞
Source: Red Meat Consumption (Heme Iron Intake) and Risk for Diabetes and Comorbidities?
To heme or not to heme
Did you catch that in the middle there, about the heme iron component?
Dietary iron is broadly divided into two kinds: heme, and non-heme.
- Heme iron comes from animals
- Non-heme iron comes from plants
Bad news for vegans: non-heme iron is not so easily absorbed as heme iron.
This means that if you’re just eating plants, the RDA may be significantly lowballing the amount actually required. As a rule, about 1.8x more iron may be needed for vegans, to compensate for it being less easily absorbed.
Why this happens: it’s because of the phytic acid / phytate in the plants that contain the iron, blocking its absorption.
Good news for vegans: however, taking iron with vitamin C increases its absorption rate by about 5x better absorption, and several other side-along nutrients do similarly, including allium (from garlic), carotenoids (from many colorful plants), and fermented foods.
Why this happens: it’s because they bind with similar sites as phytic acid, without causing the same effect. To make a metaphor: these foods steal phytic acid’s parking space, so phytic acid can’t do its iron-blocking thing.
By happy coincidence, today’s featured recipe has all of these things in, by the way (vitamin C, allium, carotenoids, and fermented foods), and the star ingredient (fava beans) is a rich source of iron.
What are good sources of iron, then?
In the category of plants:
- Beans (pick your favorites / eat a variety)
- Lentils (pick your favorites / eat a variety)
- Greens (especially dark leafy greens)
- Apricots (you can get these dried, for convenience!)
- Dark chocolate (5mg per 1oz square!)*
*Ok, technically dark chocolate is not a plant; cacao is a plant; dark chocolate is usually plant-based, though, as there is no reason to add milk.
In the category of dairy products:
That’s not a publication error; dairy products are just not great for iron. Cheeses are more nutrient-dense than milk, and have less than 0.5mg per oz, in other words, the top dairy product has around 10x less iron than dark chocolate, which came in 5th place and let’s face it, we were doing broad categories there. If we listed all the beans, lentils, greens, etc it’d be a much longer list.
Eggs, which are sometimes considered under the category of dairy by virtue of not being an animal (yet!) but an animal product, have around 1mg per egg, by the way, so considering eggs are nearer 2oz, that’s not much better than the cheese.
“But what about if…”
The above is good science and general good advice for most people. That said, some people may have conditions that preclude the foods we recommended, or have other considerations, and so things may be different. Anemia can sometimes be caused by things that can’t be fixed by diet (beyond the scope of today’s article; another time, perhaps), but for example, if you have leukemia then definitely discuss things with your doctors first. Other illnesses, and some medications, can also have troublesome effects that can contribute to anemia. Again, we can offer very good general information here, but we don’t know your medical history, and our standard legal/medical disclaimer applies as always.
See also: Do We Need Animal Products To Be Healthy?
Take care!
Share This Post
-
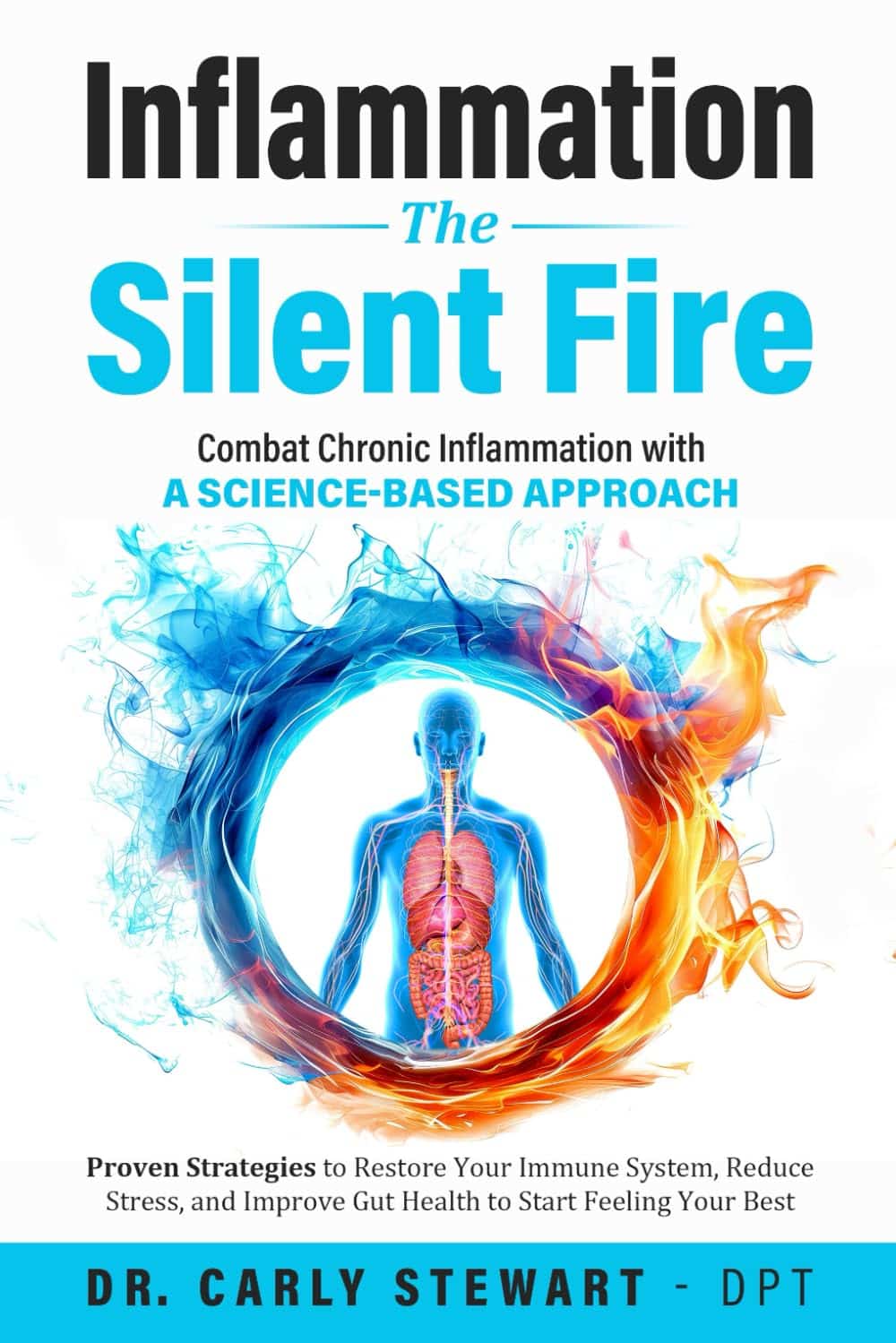
Inflammation: The Silent Fire – by Dr. Carly Stewart
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Despite its relative brevity (188 pages), this book is quite comprehensive, covering a lot more than “eat some fruits and vegetables please”.
In terms of complexity, it starts at the level of “what is inflammation?” and progresses to the nuances of NF-kB inhibitors and the role of clustered regularly interspaced short palindromic repeats and CRISPR-associated protein 9. And we do mean “progresses”; it doesn’t jump from one to the other.
The author, a doctor of physiotherapy, has plenty to say about the role of movement, as you may have guessed, and there’s a whole section on anti-inflammatory exercises to do (mostly derived from yoga), as well as all the things you might expect (and more) about diet, sleep, and so forth, plus a chapter on gut health, one on stress management (beyond the yoga and sleep and such in their respective chapters). She also covers supplements beyond the obvious, as well as medications—again, beyond the obvious.
The style is simple and explanatory, not complicating things more than necessary, nor padding it out with anecdotes or sensationalist fluff.
Bottom line: if you’d like to better manage inflammation, this book is a great resource for that.
Click here to check out Inflammation: The Silent Fire, and dial down yours!
Share This Post
-
Dioscorea Villosa: Hormones, Arthritis, & Skin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
On A Wild Yam Chase?
We recently came across a supplement blend that had wild yam extract as a minor ingredient. Our plucky (and usually very knowledgable) researcher had never heard of its use before, so she set about doing her thing. This is what she found…
What health claims are made?
Wild yam extract (Dioscorea villosa) is traditionally sold and used for:
- Balancing hormones
- Combating arthritis
- Anti-aging effects for the skin
Does it balance hormones?
First, as a quick catch-up, we’ll drop a previous article of ours for your convenience:
What Does “Balance Your Hormones” Even Mean?
We couldn’t find almost any studies into wild yam extract’s hormone-balancing effects, but we did find one study, and:
❝Symptom scores showed a minor effect of both placebo and active treatment on diurnal flushing number and severity and total non-flushing symptom scores, and on nocturnal sweating after placebo, but no statistical difference between placebo and active creams.
This study suggests that short-term treatment with topical wild yam extract in women suffering from menopausal symptoms is free of side-effects, but appears to have little effect on menopausal symptoms❞
…which is a very thorough, polite, sciencey way of saying “wow, this does so many different kinds of nothing”
On the one hand, this was a small study (n=23). On the other hand, it was also literally the only study we could find.
Does it combat arthritis?
Maybe! We again didn’t find much research into this but we did find two in vitro studies that suggests that diosgenin (which can be derived from wild yam extract) helps:
- Diosgenin inhibits IL-1β-induced expression of inflammatory mediators in human osteoarthritis chondrocytes
- Diosgenin, a plant steroid, induces apoptosis in human rheumatoid arthritis synoviocytes with cyclooxygenase-2 overexpression
And we also found a rodent study that found that wild yam extract specifically helped against “acetic acid-induced writhing and formalin-induced pain“, and put that down to anti-inflammatory properties:
So, none of these studies tell us much about whether it would be helpful for humans—with or without arthritis, and hopefully without “acetic acid-induced writhing and formalin-induced pain”.
However, they do suggest that it would be reasonable to test in humans next.
You might prefer:
- Tips For Avoiding/Managing Osteoarthritis
- Tips For Avoiding/Managing Rheumatoid Arthritis
- How to Prevent (or Reduce) Inflammation
Does it keep skin young?
Again, research is thin on the ground, but we did find some! A study with wild-yam-derived diosgenin found that it didn’t make anything worse, and otherwise performed a similar role to vitamin A:
Read: Novel effects of diosgenin on skin aging
That was on rats with breast cancer though, so its applicability to healthy humans may be tenuous (while in contrast, simply getting vitamin A instead is a known deal).
Summary
- Does it balance hormones? It probably does little to nothing in this regard
- Does it combat arthritis? It probably has anti-inflammatory effects, but we know of no studies in humans. There are much more well-established anti-inflammatories out there.
- Does it keep the skin young? We know that it performs a role similar to vitamin A for rats with breast cancer, and didn’t make anything worse for them. That’s the extent of what we know.
Where can I get some?
In the unlikely event that the above research review has inspired you with an urge to buy wild yam extract, here is an example product for your convenience.
Some final words…
If you are surprised that we’re really not making any effort to persuade you of its merits, please know that (outside of the clearly-marked sponsor section, which helps us keep the lights on, so please do visit those) we have no interest in selling you anything. We’re genuinely just here to inform 🙂
If you are wondering why we ran this article at all if the supplement has negligible merits, it’s because science is science, knowledge is knowledge, and knowing that something has negligible merit can be good knowledge to have!
Also, running articles like this from time to time helps you to know that when we do sing the praises of something, it’s with good reason
Take care!
Share This Post
Related Posts
-
Intermittent Fasting In Women
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Does intermittent fasting differ for women, and if so, how?❞
For the sake of layout, we’ve put a shortened version of this question here, but the actual wording was as below, and merits sharing in full for context
Went down a rabbit hole on your site and now can’t remember how I got to the “Fasting Without Crashing” article on intermittent fasting so responding to this email lol, but was curious what you find/know about fasting for women specifically? It’s tough for me to sift through and find legitimate studies done on the results of fasting in women, knowing that our bodies are significantly different from men. This came up when discussing with my sister about how I’ve been enjoying fasting 1-2 days/week. She said she wanted more reliable sources of info that that’s good, since she’s read more about how temporary starvation can lead to long-term weight gain due to our bodies feeling the need to store fat. I’ve also read about that, but also that fasting enables more focused autophagy in our bodies, which helps with long-term staving off of diseases/ailments. Curious to know what you all think!
~ 10almonds subscriber
So, first of all, great question! Thanks for asking it
Next up, isn’t it strange? Books come in the format:
- [title]
- [title, for women]
You would not think women are a little over half of the world’s population!
Anyway, there has been some research done on the difference of intermittent fasting in women, but not much.
For example, here’s a study that looked at 1–2 days/week IF, in other words, exactly what you’ve been doing. And, they did have an equal number of men and women in the study… And then didn’t write down whether this made a difference or not! They recorded a lot of data, but neglected to note down who got what per sex:
Here’s a more helpful study, that looked at just women, and concluded:
❝In conclusion, intermittent fasting could be a nutritional strategy to decrease fat mass and increase jumping performance.
However, longer duration programs would be necessary to determine whether other parameters of muscle performance could be positively affected by IF. ❞
~ Dr. Martínez-Rodríguez et al.
Those were “active women”; another study looked at just women who were overweight or obese (we realize that “active women” and “obese or overweight women” is a Venn diagram with some overlap, but still, the different focus is interesting), and concluded:
❝IER is as effective as CER with regard to weight loss, insulin sensitivity and other health biomarkers, and may be offered as an alternative equivalent to CER for weight loss and reducing disease risk.❞
As for your sister’s specific concern about yo-yoing, we couldn’t find studies for this yet, but anecdotally and based on books on Intermittent Fasting, this is not usually an issue people find with IF. This is assumed to be for exactly the reason you mention, the increased cellular apoptosis and autophagy—increasing cellular turnover is very much the opposite of storing fat!
You might, by the way, like Dr. Mindy Pelz’s “Fast Like A Girl”, which we reviewed previously
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Breathing Cure – by Patrick McKeown
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed this author’s “The Oxygen Advantage”, which as you might guess from the title, was also about breathing. So, what’s different here?
While The Oxygen Advantage was mostly about improving good health with optimized breathing, and with an emphasis on sports too, The Breathing Cure is more about the two-way relationship between ill health and disordered breathing (and how to fix it).
Many kinds of illnesses can affect our breathing, and our breathing can affect many types of illness; McKeown covers a lot of these, including the obvious things like respiratory diseases (including COVID and Long COVID, as well as non-infectious respiratory conditions like asthma), but also things like diabetes and heart disease, as well as peri-disease things like chronic pain, and demi-disease things like periods and menopause.
In each case (and more), he examines what things make matters better or worse, and how to improve them.
While the style itself is just as pop-science as The Oxygen Advantage, this time it relies less on anecdote (though there are plenty of anecdotes too), and leans more heavily on a generous chapter-by-chapter scientific bibliography, with plenty of citations to back up claims.
Bottom line: if you’d like to breathe better, this book can help in very many ways.
Click here to check out The Breathing Cure, and breathe easy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Healthy Cook’s Anti-Inflammatory Diet & Cookbook – by Dr. Albert Orbinati
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Chronic inflammation is a root cause of very many illnesses, and exacerbates almost all the ones it doesn’t cause. So, reducing inflammation is a very good way to stay well in general, reducing one’s risk factors for very many other diseases.
Dr. Orbinati starts by giving advice for adjusting to an anti-inflammatory diet, including advice on trying an elimination diet, if you suspect an undiagnosed allergy/intolerance.
Thereafter, he gives guidance on pantry-stocking—not just what anti-inflammatory foods to include and what inflammatory foods to skip, but also, what food and nutrient pairings are particularly beneficial, like how black pepper and turmeric are both anti-inflammatory by themselves, but the former greatly increases the bioavailability of the latter if consumed together.
The rest of the book—aside from assorted appendices, such as 8 pages of scientific references—is given over to the recipes.
The recipes themselves are, obviously, anti-inflammatory in focus. As one might expect, therefore, most are vegetarian and many are vegan, but we do find many recipes with chicken and fish as well; there’s also some use of eggs and fermented dairy in some of the recipes too.
The book certainly does deliver on its promise of flavorful healthy food; that’s what happens when one includes a lot of herbs and spices in one’s cooking, as well as the fact that many other polyphenol-rich foods are, by nature, tasty in and of themselves.
Bottom line: if you’d like to expand your anti-inflammatory culinary repertoire, this book is a top-tier choice for that.
Click here to check out Healthy Cook’s Anti-Inflammatory Diet & Cookbook, and spice up your kitchen!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: