Stick with It – by Dr. Sean Young
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most of us know the theory when it comes to building new habits and/or replacing old ones, and maybe we even implement those ideas. So why is our success rate still not as high as we think it should be?
Dr. Sean Young is here to do science to it!
This book comes with advice and explanations that rely a lot less on “that sounds reasonable” and a lot more on “in this recent high-quality study, researchers found…”
And, at 10almonds, we love that. We’re all for trying new things that sound reasonable in general… but we definitely prefer when there’s a stack of solid science to point to, and that’s the kind of thing we recommend!
Dr. Young is big on using that science to find ways to trick our brains and get them working the way we want.
Each chapter has lots of science, lots of explanations, and lots of actionable step-by-step advice.
Bottom line: if you’re all over “Atomic Habits”, this one’s the science-based heavy-artillery for your practical neurohacking.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Vibration Plate, Review After 6 Months: Is It Worth It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is it push-button exercise, or an expensive fad, or something else entirely? Robin, from “The Science of Self-Care”, has insights:
Science & Experience
According to the science (studies cited in the video and linked-to in the video description, underneath it on YouTube), vibration therapy does have some clear benefits, namely:
- Bone health (helps with bone density, particularly beneficial for postmenopausal women)
- Muscle recovery (reduces lactate levels, aiding faster recovery)
- Joint health (reduces pain and improves function in osteoarthritis patients)
- Muscle stimulation (helps older adults maintain muscle mass)
- Cognitive function (due to increased blood flow to the brain)
And from her personal experience, the benefits included:
- Improved recovery after exercise, reducing muscle soreness and stiffness
- Reduced back pain and improved posture (not surprising, given the need for stabilizing muscles when using one of these)
- Better circulation and (likely resulting from same) skin clarity
She did not, however, notice:
- Any reduction in cellulite
- Any change in body composition (fat loss or muscle gain)
For a deeper look into these things and more, plus a demonstration of how the machine actually operates, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
Unprocess Your Life – by Rob Hobson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Rob Hobson is not a doctor, but he is a nutritionist with half the alphabet after his name (BSc, PGDip, MSc, AFN, SENR) and decades of experience in the field.
The book covers, in jargon-free fashion, the science of ultra-processed foods, and why for example that pack of frozen chicken nuggets are bad but a pack of tofu (which obviously also took some processing, because it didn’t grow on the plant like that) isn’t.
This kind of explanation puts to rest a lot of the “does this count?” queries that a reader might have when giving the shopping list a once-over.
He also covers practical considerations such as kitchen equipment that’s worth investing in if you don’t already have it, and an “unprocessed pantry” shopping list.
The recipes (yes, there are recipes, nearly a hundred of them) are not plant-based by default, but there is a section of vegan and vegetarian recipes. Given that the theme of the book is replacing ultra-processed foods, it doesn’t mean a life of abstemiousness—there are recipes for all manner of things from hot sauce to cakes. Just, healthier unprocessed ones! There are classically healthy recipes too, of course.
Bottom line: if you’ve been wishing for a while that you could get rid of those processed products that are just so convenient that you haven’t got around to replacing them with healthier options, this book can indeed help you do just that.
Click here to check out Unprocess Your Life, and unprocess your life!
Share This Post
-
The Teenage Brain – by Dr. Frances Jensen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We realize that we probably have more grandparents of teenagers than parents of teenagers here, but most of us have at least some teenage relative(s). Which makes this book interesting.
There are a lot of myths about the teenage brain, and a lot of popular assumptions that usually have some basis in fact but are often misleading.
Dr. Jensen gives us a strong foundational grounding in the neurophysiology of adolescence, from the obvious-but-often-unclear (such as the role of hormones) to less-known things like the teenage brain’s general lack of myelination. Not just “heightened neuroplasticity” but, if you imagine the brain as an electrical machine, then think of myelin as the insulation between the wires. Little wonder some wires may get crossed sometimes!
She also talks about such things as the teenage circadian rhythm’s innate differences, the impact of success and failure on the brain, and harder topics such as addiction—and the adolescent cortisol functions that can lead to teenagers needing to seek something to relax in the first place.
In criticism, we can only say that sometimes the author makes sweeping generalizations without acknowledging such, but that doesn’t detract from what she has to say on the topic of neurophysiology.
Bottom line: if there’s a teenager in your life whose behavior and/or moods are sometimes baffling to you, and whose mysteries you’d like to unravel, this is a great book.
Click here to check out the Teenage Brain, and better understand those around you!
Share This Post
Related Posts
-
Cupping: How It Works (And How It Doesn’t)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Good Health By The Cup?
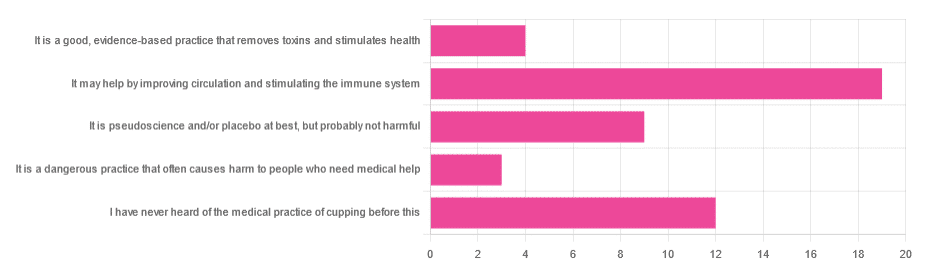
In Tuesday’s newsletter, we asked you for your opinion of cupping (the medical practice), and got the above-depicted, below-described, set of responses:
- About 40% said “It may help by improving circulation and stimulating the immune system”
- About 26% said “I have never heard of the medical practice of cupping before this”
- About 19% said “It is pseudoscience and/or placebo at best, but probably not harmful
- About 9% said “It is a good, evidence-based practice that removes toxins and stimulates health”
- About 6% said “It is a dangerous practice that often causes harm to people who need medical help”
So what does the science say?
First, a quick note for those unfamiliar with cupping: it is the practice of placing a warmed cup on the skin (open side of the cup against the skin). As the warm air inside cools, it reduces the interior air pressure, which means the cup is now (quite literally) a suction cup. This pulls the skin up into the cup a little. The end result is visually, and physiologically, the same process as what happens if someone places the nozzle of a vacuum cleaner against their skin. For that matter, there are alternative versions that simply use a pump-based suction system, instead of heated cups—but the heated cups are most traditional and seem to be most popular. See also:
National Center for Complementary and Integrative Health | Cupping
It is a dangerous practice that often causes harm to people who need medical help: True or False?
False, for any practical purposes.
- Directly, it can (and usually does) cause minor superficial harm, much like many medical treatments, wherein the benefits are considered to outweigh the harm, justifying the treatment. In the case of cupping, the minor harm is usually a little bruising, but there are other risks; see the link we gave just above.
- Indirectly, it could cause harm by emboldening a person to neglect a more impactful treatment for their ailment.
But, there’s nothing for cupping akin to the “the most common cause of death is when someone gets a vertebral artery fatally severed” of chiropractic, for example.
It is a good, evidence-based practice that removes toxins and stimulates health: True or False?
True and False in different parts. This one’s on us; we included four claims in one short line. But let’s look at them individually:
- Is it good? Well, those who like it, like it. It legitimately has some mild health benefits, and its potential for harm is quite small. We’d call this a modest good, but good nonetheless.
- Is it evidence-based? Somewhat, albeit weakly; there are some papers supporting its modest health claims, although the research is mostly only published in journals of alternative medicine, and any we found were in journals that have been described by scientists as pseudoscientific.
- Does it remove toxins? Not directly, at least. There is also a version that involves making a small hole in the skin before applying the cup, the better to draw out the toxins (called “wet cupping”). This might seem a little medieval, but this is because it is from early medieval times (wet cupping’s first recorded use being in the early 7th century). However, the body’s response to being poked, pierced, sucked, etc is to produce antibodies, and they will do their best to remove toxins. So, indirectly, there’s an argument.
- Does it stimulate health? Yes! We’ll come to that shortly. But first…
It is pseudoscience and/or placebo at best, but probably not harmful: True or False?
True in that its traditionally-proposed mechanism of action is a pseudoscience and placebo almost certainly plays a strong part, and also in that it’s generally not harmful.
On it being a pseudoscience: we’ve talked about this before, but it bears repeating; just because something’s proposed mechanism of action is pseudoscience, doesn’t necessarily mean it doesn’t work by some other mechanism of action. If you tell a small child that “eating the rainbow” will improve their health, and they believe this is some sort of magical rainbow power imbuing them with health, then the mechanism of action that they believe in is a pseudoscience, but eating a variety of colorful fruit and vegetables will still be healthy.
In the case of cupping, its proposed mechanism of action has to do withbalancing qi, yin and yang, etc (for which scientific evidence does not exist), in combination with acupuncture lore (for which some limited weak scientific evidence exists). On balancing qi, yin and yang etc, this is a lot like Europe’s historically popular humorism, which was based on the idea of balancing the four humors (blood, yellow bile, black bile, phlegm). Needless to say, humorism was not only a pseudoscience, but also eventually actively disproved with the advent of germ theory and modern medicine. Cupping therapy is not more scientifically based than humorism.
On the placebo side of things, there probably is a little more to it than that; much like with acupuncture, a lot of it may be a combination of placebo and using counter-irritation, a nerve-tricking method to use pain to reduce pain (much like pressing with one’s nail next to an insect bite).
Here’s one of the few studies we found that’s in what looks, at a glance, to be a reputable journal:
Cupping therapy and chronic back pain: systematic review and meta-analysis
It may help by improving circulation and stimulating the immune system: True or False?
True! It will improve local circulation by forcing blood into the area, and stimulate the immune system by giving it a perceived threat to fight.
Again, this can be achieved by many other means; acupuncture (or just “dry needling”, which is similar but without the traditional lore), a cold shower, and/or exercise (and for that matter, sex—which combines exercise, physiological arousal, and usually also foreign bodies to respond to) are all options that can improve circulation and stimulate the immune system.
You can read more about using some of these sorts of tricks for improving health in very well-evidenced, robustly scientific ways here:
The Stress Prescription (Against Aging!)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Figs vs Plums – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing figs to plums, we picked the figs.
Why?
In terms of macros, figs have more protein, carbs, and fiber; the glycemic index is about equal so we’ll call this category either a tie, or a nominal win for figs (as the “more food per food” option).
In the category of vitamins, figs have more of vitamins B1, B2, B3, B5, B6, B7, B9, and choline, while plums have more of vitamins A, C, E, and K. We may subjectively prefer one set of vitamins or the other (depending on the rest of our diet, for example), but by the numbers, this is a 7:4 victory for figs.
When it comes to minerals, figs have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while plums are not higher in any minerals. An easy win for figs here.
Of course, enjoy either or both, but if you’re going to pick one for nutritional density, we say it’s figs, as illustrated scientifically below:
Want to learn more?
You might like to read:
Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why You Can’t Deep Squat (And the Benefits You’re Missing)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Matt Hsu fought his own battle with chronic pain from the age of 16 in his feet, knees, hips, back, shoulders, elbows, forearms, wrists, hands, and head. Seeking answers, he’s spent a career in corrective exercise, posture alignment, structural integration, orthopedic exercise, sports medicine, and has more certifications than we care to list. In short, he knows his stuff.
Yes you can (with some work)
The deep squat, also called Asian squat, Slav squat, sitting squat, resting squat, primal squat, and various other names, is an important way of sitting that has implications for a lot of aspects of health.
Why it’s so important: it preserves the mobility of our hips, ankles, and everything in between, and maintaining especially the hip mobility makes a big difference not only to general health, but also to reducing the risk of injury. It also maintains lower body strength, making falls in older age less likely in the first place, and if falls do happen, makes injury less likely, and if injury does happen, makes the injury likely less severe.
An important misconception: there is a popular, but unfounded, belief that the ability or inability to do this is decided by genes—or if not outright decided, that at the very least Asians and Slavs have a genetic advantage. However, this is simply not true. Westerners and others can learn to do it just fine, and on the flipside, Asians and Slavs who grew up in the West may often struggle with it. The truth is, the deciding factor is lifestyle: if your culture involves sitting this way more often, you’ll be able to do it more comfortably and easily than if you’re just now trying it for the first time.
Factors that you can control: you can’t change where you grew up, but you can change how you sit down now. Achieving the squat requires repeated position practice, and the more frequently you do so (even if you just start with a few seconds and work your way up to longer periods), the better you’ll get at it. And, on the contrary, sitting in chairs weakens and shortens the muscles involved, so any time you spend sitting in chairs is working against you. There are many reasons it’s advisable to avoid sitting in chairs more than necessary, and this is one of them.
10almonds tip: a limiting factor for many people initially is ankle flexibility, which may result in one’s center of gravity being a bit far back, leading to a tendency to have to change something to avoid toppling over backwards. Rather than holding onto something immobile (e.g. furniture) in front of where you are sitting, consider simply holding an object in front of you in your hands. A book is a fine example; holding that in front of you (feel free to read the book) will shift your center of gravity forwards a bit, and will thus allow you to sit there a little longer, thus improving your strength and flexibility while you do, until you can do it without holding something in front of you. If you try with a book and you’re still prone to toppling backwards, try with something heavier, but do use the minimum weight necessary, because ultimately the counterbalance is just a crutch to get you to where you need to be.
For more visual advice on how to do it, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: