Spoon-Fed – by Dr. Tim Spector
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Spector looks at widespread beliefs about food, and where those often scientifically disproven beliefs come from. Hint, there’s usually some manner of “follow the money”.
From calorie-counting to cholesterol content, from fish to bottled water, to why of all the people who self-report having an allergy, only around half turn out to actually have one when tested, Dr. Spector sets the record straight.
The style is as very down-to-earth and not at all self-aggrandizing; the author acknowledges his own mistakes and limitations along the way. In terms of pushing any particular agenda, his only agenda is clear: inform the public about bad science, so that we demand better science going forwards. Along the way, he gives us lots of information that can inform our personal health choices based on better science than indiscriminate headlines wildly (and sometimes intentionally) misinterpreting results.
Read this book, and you may find yourself clicking through to read the studies for yourself, next time you see a bold headline.
Bottom line: this book looks at a lot of what’s wrong with what a lot of people believe about healthy eating. Regular 10almonds readers might not find a lot that’s new here, but it could be a great gift for a would-be health-conscious friend or relative
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Superfood Baked Apples
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Superfoods, and super-tasty. This is a healthy twist on a classic; your blood sugars will thank you for choosing this tasty sweet delight. It’s also packed with nutrients!
You will need
- 2 large firm baking apples, cored but not peeled
- 1/2 cup chopped walnuts
- 3 tbsp goji berries, rehydrated (soak them in warm water for 10–15minutes and drain)
- 1 tbsp honey, or maple syrup, per your preference (this writer is also a fan of aged balsamic vinegar for its strong flavor and much milder sweetness. If you don’t like things to be too sweet, this is the option for you)
- 2 tsp ground sweet cinnamon
- 1 tsp ground ginger
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 180℃ / 350℉ / gas mark 4
2) Mix the chopped walnuts with the goji berries and the honey (or whatever you used instead of the honey) as well as the sweet cinnamon and the ginger.
3) Place the apples in shallow baking dish, and use the mixture you just made to stuff their holes.
4) Add 1/2 cup water to the dish, around the apples. Cover gently with foil, and bake until soft.
Tip: check them every 20 minutes; they may be done in 40 or it may take 60; in honesty it depends on your oven. If unsure, cook them for longer at a lower temperature.
5) Serve warm.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- From Apples to Bees, and High-Fructose C’s
- Why You Should Diversify Your Nuts!
- Goji Berries: Which Benefits Do They Really Have?
- The Sugary Food That Lowers Blood Sugars
- Honey vs Maple Syrup – Which is Healthier?
- A Tale Of Two Cinnamons ← this is important, about why we chose the sweet cinnamon
- Ginger Does A Lot More Than You Think
Take care!
Share This Post
-
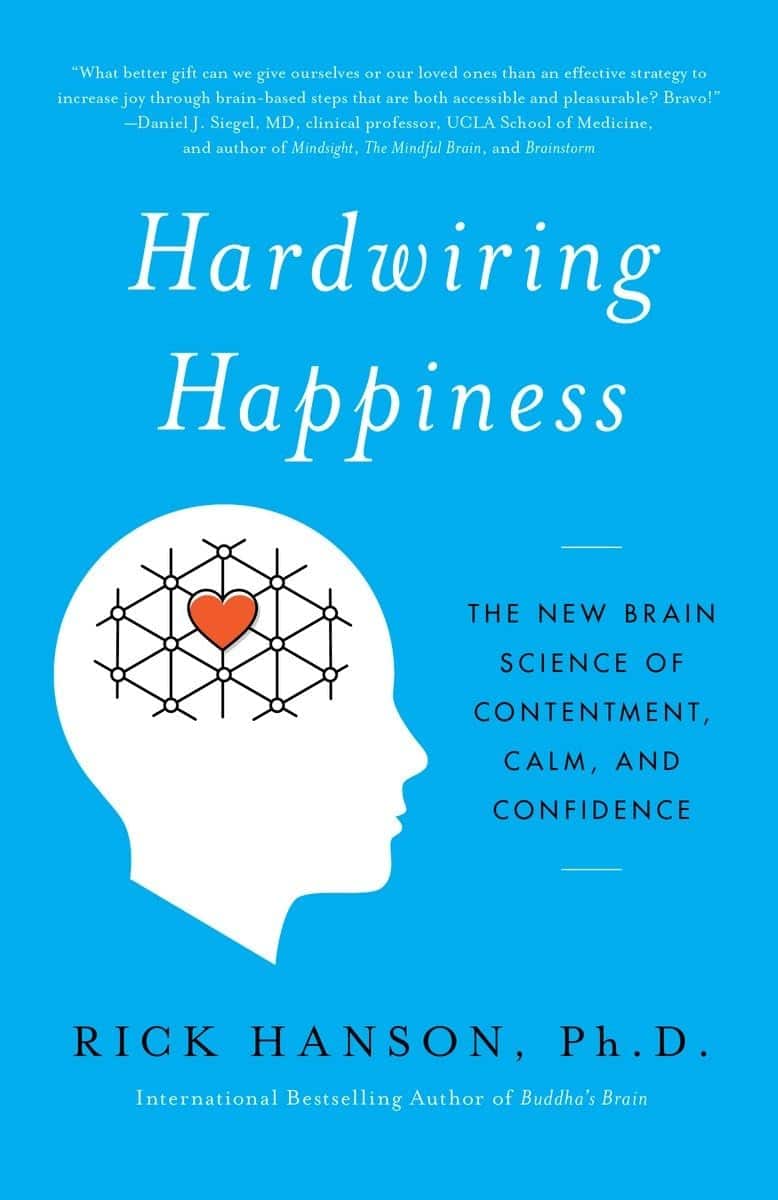
Hardwiring Happiness – by Dr. Rick Hanson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Publishers are very excitable about “the new science of…”, and it’s almost never actually a new science of. But what about in this case?
No, it isn’t. It’s the very well established science of! And that’s a good thing, because it means this book is able to draw on quite a lot of research and established understanding of how neuroplasticity works, to leverage that and provide useful guidance.
A particular strength of this book is that while it polarizes the idea that some people have “happy amygdalae” and some people have “sad amygdalae”, it acknowledges that it’s not just a fated disposition and is rather the result of the lives people have led… And then provides advice on upgrading from sad to happy, based on the assumption that the reader is quite possibly coming from a non-ideal starting point.
The bookdoes an excellent job of straddling neuroscience and psychology, which sounds like not much of a straddle (the two are surely very connected, after all, right?) but this does mean that we’re hearing about the chemical structure of DNA inside the nuclei of the neurons of the insula, not long after reading an extended gardening metaphor about growth, choices, and vulnerabilities.
Bottom line: if you’d like a guide to changing your brain for the better (happier) that’s not just “ask yourself: what if it goes well?” and similar CBTisms, then this is a fine book for you.
Click here to check out Hardwiring Happiness, and indeed hardwire happiness!
Share This Post
-
Rebalancing Dopamine (Without “Dopamine Fasting”)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Rebalancing Dopamine (Without “Dopamine Fasting”)
Credit Steve Fisch This is Dr. Anna Lembke. She’s a professor of psychiatry at Stanford, and chief of the Stanford Addiction Medicine Dual Diagnosis Clinic—as well as running her own clinical practice, and serving on the board of an array of state and national addiction-focused organizations.
Today we’re going to look at her work on dopamine management…
Getting off the hedonic treadmill
For any unfamiliar with the term, the “hedonic treadmill” is what happens when we seek pleasure, enjoy the pleasure, the pleasure becomes normalized, and now we need to seek a stronger pleasure to get above our new baseline.
In other words, much like running on a reciprocal treadmill that just gets faster the faster we run.
What Dr. Lembke wants us to know here: pleasure invariably leads to pain
This is not because of some sort of extrinsic moral mandate, nor even in the Buddhist sense. Rather, it is biology.
Pleasure and pain are processed by the same part of the brain, and if we up one, the other will be upped accordingly, to try to keep a balance.
Consequently, if we recklessly seek “highs”, we’re going to hit “lows” soon enough. Whether that’s by drugs, sex, or just dopaminergic habits like social media overuse.
Dr. Lembke’s own poison of choice was trashy romance novels, by the way. But she soon found she needed more, and more, and the same level wasn’t “doing it” for her anymore.
So, should we just give up our pleasures, and do a “dopamine fast”?
Not so fast!
It depends on what they are. Dopamine fasting, per se, does not work. We wrote about this previously:
Short On Dopamine? Science Has The Answer
However, when it comes to our dopaminergic habits, a short period (say, a couple of weeks) of absence of that particular thing can help us re-find our balance, and also, find insight.
Lest that latter sound wishy-washy: this is about realizing how bad an overuse of some dopaminergic activity had become, the better to appreciate it responsibly, going forwards.
So in other words, if your poison is, as in Dr. Lembke’s case, trashy romance novels, you would abstain from them for a couple of weeks, while continuing to enjoy the other pleasures in life uninterrupted.
Substances that create a dependency are a special case
There’s often a popular differentiation between physical addictions (e.g. alcohol) and behavioral addictions (e.g. video games). And that’s fair; physiologically speaking, those may both involve dopamine responses, but are otherwise quite different.
However, there are some substances that are physical addictions that do not create a physical dependence (e.g. sugar), and there are substances that create a physical dependence without being addictive (e.g. many antidepressants)
See also: Addiction and physical dependence are not the same thing
In the case of anything that has created a physical dependence, Dr. Lembke does not recommend trying to go “cold turkey” on that without medical advice and supervision.
Going on the counterattack
Remember what we said about pleasure and pain being processed in the same part of the brain, and each rising to meet the other?
While this mean that seeking pleasure will bring us pain, the inverse is also true.
Don’t worry, she’s not advising us to take up masochism (unless that’s your thing!). But there are very safe healthy ways that we can tip the scales towards pain, ultimately leading to greater happiness.
Cold showers are an example she cites as particularly meritorious.
As a quick aside, we wrote about the other health benefits of these, too:
A Cold Shower A Day Keeps The Doctor Away?
Further reading
Want to know more? You might like her book:
Dopamine Nation: Finding Balance in the Age of Indulgence
Enjoy!
Share This Post
Related Posts
-
How To Engage Your Whole Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Stroke Of Insight That Nobody Wants
This is Dr. Jill Bolte Taylor. She’s a neuroanatomist, who, at the age of 37 (when she was a post-doctoral fellow at Harvard Medical School), had what she refers to as her “stroke of insight”.
That is to say, she had a massive stroke, and after a major brain surgery to remove a clot the size of a golf ball, she spent the next 8 years re-learning to do everything.
Whereas previously she’d been busy mapping the brain to determine how cells communicate with each other, now she was busy mapping whether socks or shoes should go on first. Needless to say, she got an insight into neuroplasticity that few people would hope for.
What does she want us to know?
Dr. Taylor (now once again a successful scientist, lecturer, and author) advocates for “whole brain living”, which involves not taking parts of our brain for granted.
About those parts…
Dr. Taylor wants us to pay attention to all the parts regardless of size, ranging from the two hemispheres, all the way down to the billions of brain cells, and yet even further, to the “trillions of molecular geniuses”—because each brain cell is itself reliant on countless molecules of the many neurochemicals that make up our brain.
For a quick refresher on some of the key players in that latter category, see our Neurotransmitter Cheatsheet 😎
When it comes to the hemispheres, there has historically been a popular belief that these re divided into:
- The right brain: emotional, imaginative, creative, fluid feeling
- The left brain: intellectual, analytical, calculating, crystal thinking
…which is not true, anatomically speaking, because there are cells on both sides doing their part of both of these broad categories of brain processes.
However, Dr. Taylor found, while one hemisphere of her brain was much more damaged than the other, that nevertheless she could recover some functions more quickly than others, which, once she was able to resume her career, inspired her model of four distinct ways of cogitating that can be switched-between and played with or against each other:
Meet The Four Characters Inside Your Brain
Why this matters
As she was re-learning everything, the way forward was not quick or easy, and she also didn’t know where she was going, because for obvious reasons, she couldn’t remember, much less plan.
Looking backwards after her eventual full recovery, she noted a lot of things that she needed during that recovery, some of which she got and some of which she didn’t.
Most notably for her, she needed the right kind of support that would allow all four of the above “characters” as she puts it, to thrive and grow. And, when we say “grow” here we mean that literally, because of growing new brain cells to replace the lost ones (as well as the simple ongoing process of slowly replacing brain cells).
For more on growing new brain cells, by the way, see:
How To Grow New Brain Cells (At Any Age)
In order to achieve this in all of the required brain areas (i.e., and all of the required brain functions), she also wants us to know… drumroll please…
When to STFU
Specifically, the ability to silence parts of our brain that while useful in general, aren’t necessarily being useful right now. Since it’s very difficult to actively achieve a negative when it comes to brain-stuff (don’t think of an elephant), this means scheduling time for other parts of our brain to be louder. And that includes:
- scheduling time to feel (emotionally)
- scheduling time to feel (gut feelings)
- scheduling time to feel (kinesthetically)
…amongst others.
Note: those three are presented in that order, from least basic to most basic. And why? Because, clever beings that we are, we typically start from a position that’s not remotely basic, such as “overthinking”, for example. So, there’s a wind-down through thinking just the right amount, thinking through simpler concepts, feeling, noticing one’s feelings, noticing noticing one’s feelings, all the way down to what, kinesthetically, are we actually physically feeling.
❝It is interesting to note that although our limbic system fucntions throughout our lifetime, it does not mature. As a result, when our emotional “buttons” are pushed, we retain the ability to react to incoming stimulation as though we were a two-year-old, even when we are adults.❞
~ Dr. Jill Taylor
Of course, sometimes the above is not useful, which is why the ability to switch between brain modes is a very important and useful skill to develop.
And how do we do that? By practising. Which is something that it’s necessary to take up consciously, and pursue consistently. When children are at school, there are (hopefully, ideally) curricula set out to ensure they engage and train all parts of their brain. As adults, this does not tend to get the same amount of focus.
“Children’s brains are still developing”—indeed, and so are adult brains:
The Brain As A Work-In-Progress
Dr. Taylor had the uncommon experience of having to, in many ways, neurologically speaking, redo childhood. And having had a second run at it, she developed an appreciation of the process that most of us didn’t necessarily get when doing childhood just the once.
In other words: take the time to feel stuff; take the time to quiet down your chatty mind, take the time engage your senses, and take it seriously! Really notice, as though for the first time, what the texture of your carpet is like. Really notice, as though for the first time, what it feels like to swallow some water. Really notice, as though for the first time, what it feels like to experience joy—or sadness, or comfort, or anger, or peace. Exercise your imagination. Make some art (it doesn’t have to win awards; it just has to light up your brain!). Make music (again, it’s about wiring your brain in your body, not about outdoing Mozart in composition and/or performance). Make changes! Make your brain work in the ways it’s not in the habit of doing.
If you need a little help switching off parts of your brain that are being too active, so that you can better exercise other parts of your brain that might otherwise have been neglected, you might want to try:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Speedy Easy Ratatouille
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One of the biggest contributing factors to unhealthy eating? The convenience factor. To eat well, it seems, one must have at least two of the following: money, time, and skill. So today we have a health dish that’s cheap, quick, and easy!
(You won’t need a rat in a hat to help you with this one)
You will need
- 3 ripe tomatoes, roughly chopped
- 2 zucchini, halved and chopped into thick batons
- 2 portobello mushrooms, sliced into ½” slices
- 1 large red pepper, cut into thick chunks
- 3 tbsp extra virgin olive oil
- 2 tbsp finely chopped parsley
- 2 tsp garlic paste
- 2 tsp thyme leaves, destalked
- 1 tsp rosemary leaves, destalked
- 1 tsp red chili flakes
- 1 tsp black pepper
- Optional: 1 tsp MSG, or 1 tsp low sodium salt (the MSG is the healthier option as it contains less sodium than even low sodium salt)
- Optional: other vegetables, chopped. Use what’s in your fridge! This is a great way to use up leftovers. Particularly good options include chopped eggplant, chopped red onion, and/or chopped carrot.
Method
(we suggest you read everything at least once before doing anything)
1) Put the olive oil into a sauté pan and set the heat on medium. When hot but smoking, add the mushrooms and any optional vegetables (but not the others from the list yet), and fry for 5 minutes.
Note: if you aren’t pressed for time, then you can diverge from the “speedy” part of this by cooking each of the vegetables separately before combining, which allows each to keep its flavor more distinct.
2) Add the garlic, followed by the zucchini, red pepper, chili flakes, and thyme; stir periodically (you shouldn’t have to stir constantly) for 10 minutes.
3) Add the tomatoes and a cup of water to the pan, along with any MSG/salt. Cover with the lid and allow to simmer for a further 10 minutes.
4) Serve, adding the garnish.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- The Magic Of Mushrooms: “The Longevity Vitamin” (That’s Not A Vitamin)
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we had 3/5 today!
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
- MSG vs Salt: Sodium Comparison
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Simple Wall Pilates for Seniors – by Grace Clark
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
While the cover illustration makes this look a little too simple, in fact there’s a lot of value in this book, with exercises ranging from things like that on the cover, to the “wall downward dog”. But the actual exercises (of which there are 29) themselves are only a part of the book (taking about 70 pages of it with clear illustrations).
There’s also a lot about important Pilates principles to apply, such as breathing, correct body alignment (if you don’t already do Pilates, you will not have this, as Pilates alignment is quite specific), flexibility, balance, stability, coordination, range of motion, isometric exercise considerations, endurance, and more.
Unlike a lot of “…for seniors” books, this is not a watered down barely-does-anything version of the “real” exercises, but rather, would present most the same challenges to a 20-year-old reader; it’s just that the focus here is more on matters that tend to concern an older rather than younger demographic. That 20-something may be busy building their butt, for instance, while the 80-year-old is building their bones. No reason both shouldn’t do both, of course, but the focus is age-specific.
The author guides us through working up from easy things to hard, breaking stuff down so that we can progress at our own pace, such that even the most cautious or enthusiastic reader can start at an appropriate point and proceed accordingly.
She also talks us through a 28-day program (as promised by the subtitle), and advice on how to keep it going without plateauing, how to set realistic goals, how to tailor it to our abilities as we go, track our progress, and so forth.
The style is clear and instructional, and one thing that sets this apart from a lot of Pilates books is that the education comes from an angle not of “trust me”, but rather from well-sourced claims with bibliography whose list spans 5 pages at the end.
Bottom line: if you’d like to progressively increase your strength, stability, and more—with no gym equipment, just a wall—then this book will have you see improvements in the 28 days it promises, and thereafter.
Click here to check out Simple Wall Pilates For Seniors, and experience the difference!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: