Simple, 10-Minute Hip Opening Routine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hips Feeling Stiff?
If so, Flow with Adee’s video (below) has just the solution with a quick 10-minute hip-opening routine. Designed for intermediates but open to all, we love Adee’s work and recommend that you reach out to her to tell her what you’d like to see next.
Other Methods
If you’re a book lover, we’ve reviewed a fantastic book on reducing hip pain. Alternatively, learn stretching from a ballerina with Jasmine McDonald’s ballet stretching routine.
Otherwise, enjoy today’s video:
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
From Strength to Strength – by Dr. Arthur Brooks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For most professions, there are ways in which performance can be measured, and the average professional peak varies by profession, but averages are usually somewhere in the 30–45 range, with a pressure to peak between 25–35.
With a peak by age 45 or perhaps 50 at the latest (aside from some statistical outliers, of course), what then to expect at age 50+? Not long after that, there’s a reason for mandatory retirement ages in some professions.
Dr. Brooks examines the case for accepting that rather than fighting it, and/but making our weaknesses into our strengths as we go. If our fluid intelligence slows, our accumulated crystal intelligence (some might call it “wisdom“) can make up for it, for example.
But he also champions the idea of looking outside of ourselves; of the importance of growing and fostering connections; giving to those around us and receiving support in turn; not transactionally, but just as a matter of mutualism of the kind found in many other species besides our own. Indeed, Dr. Brooks gives the example of a grove of aspen trees (hence the cover art of this book) that do exactly that.
The style is very accessible in terms of language but with frequent scientific references, so very much a “best of both worlds” in terms of readability and information-density.
Bottom line: if ever you’ve wondered at what age you might outlive your usefulness, this book will do as the subtitle suggests, and help you carve out your new place.
Click here to check out From Strength To Strength, and find yours!
Share This Post
-
10% Human – by Dr. Alanna Collen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The title, of course, is a nod to how by cell count, we are only about 10% human, and the other 90% are assorted microbes.
Dr. Collen starts with the premise that “all diseases begin in the gut” which is perhaps a little bold, but as a general rule of thumb, the gut is, in fairness, implicated in most things—even if not being the cause, it generally plays at least some role in the pathogenesis of disease.
The book talks us through the various ways that our trillions of tiny friends (and some foes) interact with us, from immune-related considerations, to nutrient metabolism, to neurotransmitters, and in some cases, direct mind control, which may sound like a stretch but it has to do with the vagus nerve “gut-brain highway”, and how microbes have evolved to tug on its strings just right. Bearing in mind, most of these microbes have very short life cycles, which means evolution happens for them so much more rapidly than it does for us—something that Dr. Collen, with her PhD in evolutionary biology, has plenty to say about.
There is a practical element too: advice on how to avoid the many illnesses that come with having our various microbiomes (it’s not just the gut!) out of balance, and how to keep everything working together as a team.
The style is quite light pop-science and, once we get past the first chapter (which is about the history of the field), quite a pleasant read as Dr. Collen has an enjoyable and entertaining tone.
Bottom line: if you’d like to understand more about all the things that come together to make us functionally 100% human, then this book is an excellent guide to that.
Click here to check out 10% Human, and learn about how we interact with ourselves!
Share This Post
-
The Food Additive You Do Want
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Q: When Is A Fiber Not A Fiber?
A: when it’s a resistant starch. What’s it resistant to? Digestion. So, it functions as though a fiber, and by some systems, may get classified as such.
It’s a little like how sucralose is technically a sugar, but the body processes it like a fiber (but beware, because the sweetness of this disaccharide alone can trigger an insulin response anyway—dose dependent)
There may be other problems too:
But today’s not about sucralose, it’s about…
Guar gum’s surprising dietary role
You may have noticed “guar gum” on the list of ingredients of all kinds of things from baked goods to dairy products to condiments to confectionary and more.
It’s also used in cosmetics and explosives, but let’s not focus on that.
It’s used in food products as…
- a bulking agent
- a thickener
- a stabilizer
Our attention was caught by a new study, that found:
Resistant starch intake facilitates weight loss in humans by reshaping the gut microbiota
Often people think of “fiber helps weight loss” as “well yes, if you are bulking out your food with sawdust, you will eat less”, but it’s not that.
There’s an actual physiological process going on here!
We can’t digest it, but our gut microbiota can and will ferment it. See also:
Fiber against pounds: Resistant starch found to support weight loss
Beyond weight loss
Not everyone wants to lose weight, and even where weight loss is a goal, it’s usually not the only goal. As it turns out, adding guar gum into our diet does more things too:
Resistant starch supplement found to reduce liver triglycerides in people with fatty liver disease
(specifically, this was about NAFLD, non-alcoholic fatty liver disease)
Digging a little, it seems the benefits don’t stop there either:
Diet high in guar gum fiber limits inflammation and delays multiple sclerosis symptoms
(this one was a rodent study, but still, it’s promising and it’s consistent with what one would expect based on what else we know about its function in diet)
Should we just eat foods with guar gum in as an additive?
That depends on what they are, but watch out for the other additives if you do!
You can just buy guar gum by itself, by the way (here’s an example product on Amazon).
It’s doubtlessly no fun to take as a supplement (we haven’t tried this one), but it can be baked into bread, if baking’s your thing, or just used as a thickener in recipes where ordinarily you might use cornstarch or something else.
Can I get similar benefits from other foods?
The relevant quality is also present in resistant starches in general, so you might want to check out these foods, for example:
9 Foods That Are High in Resistant Starch
You can also check out ways to increase your fiber intake in general:
Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
Enjoy!
Share This Post
Related Posts
-
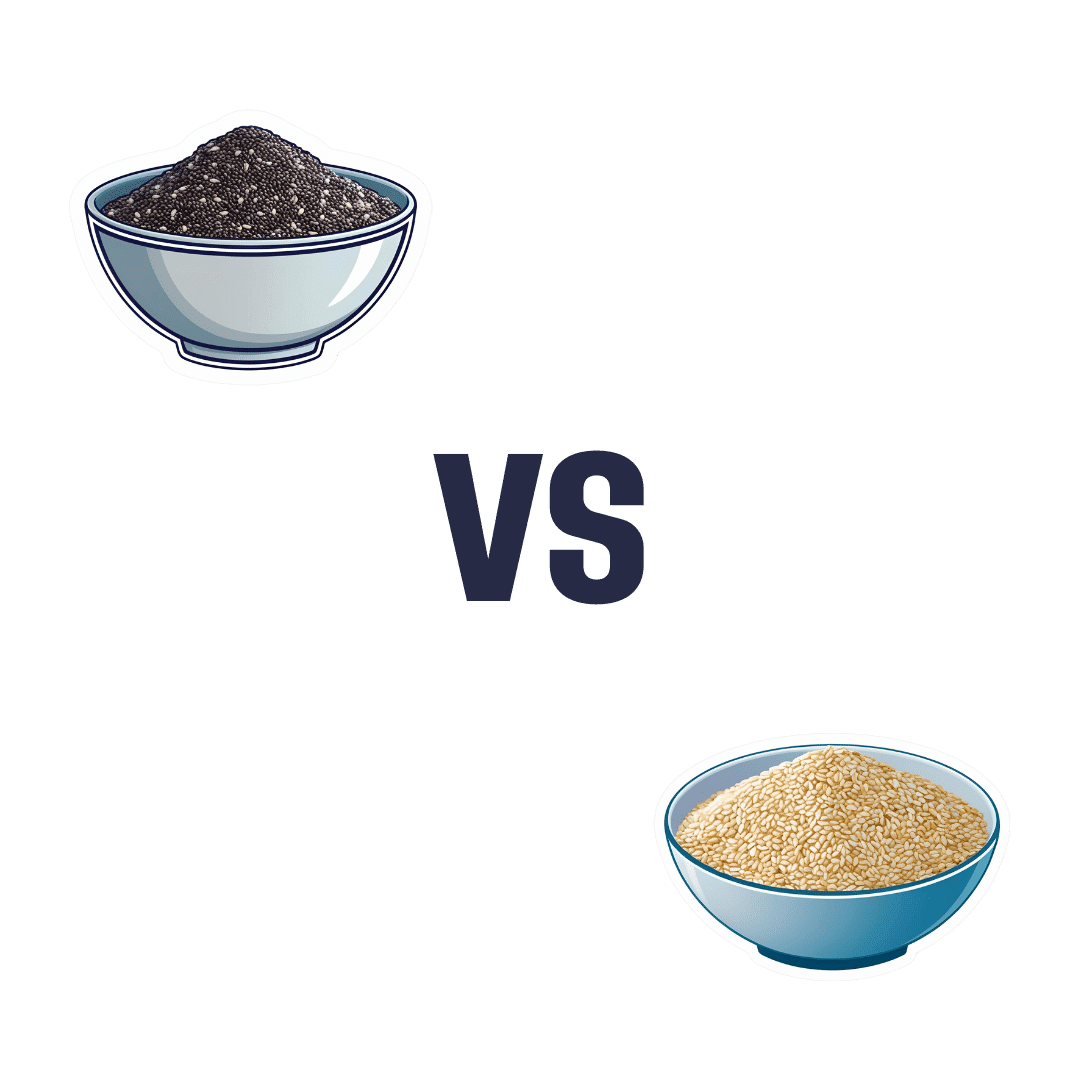
Chia vs Sesame – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing chia to sesame, we picked the chia.
Why?
This might not be a shocking decision; after all, chia has an awesome reputation, and it’s well deserved. But sesame seeds are great too, and definitely have their strengths!
In terms of macros, chia seeds have more than 3x the fiber (which is lots) for a little over 1.5x the carbs (giving it the lower glycemic index), and about equal protein. The matter of fats is also interesting: sesame seeds have nearly 2x the fat, but chia seeds have the better fats profile, with less saturated fat and more omega-3s. All in all, a sound win for chia in this category!
In the category of vitamins, chia seeds have more of vitamins B3, C, E, and choline, while sesame seeds have more of vitamins B1, B2, and B9. A more marginal win for chia here.
When it comes to minerals, chia seeds have more phosphorus, manganese, and selenium, while sesame seeds have more calcium, copper, iron, and zinc, making it a marginal win for sesame seeds this time!
Adding up the sections make for an overall win for chia (especially if we were to consider the macros category for its full weight, given the importance of those components, but it’s still a 2:1 win for chia even if we pay no attention to that), but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
The Tiniest Seeds With The Most Value: If You’re Not Taking Chia, You’re Missing Out
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Considering taking Wegovy to lose weight? Here are the risks and benefits – and how it differs from Ozempic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The weight-loss drug Wegovy is now available in Australia.
Wegovy is administered as a once-weekly injection and is approved specifically for weight management. It’s intended to be used in combination with a reduced-energy diet and increased physical activity.
So how does Wegovy work and how much weight can you expect to lose while taking it? And what are the potential risks – and costs – for those who use it?
Let’s look at what the science says.
Halfpoint/Shutterstock What is Wegovy?
Wegovy is a brand name for the medication semaglutide. Semaglutide is a glucagon-like peptide-1 receptor agonist (GLP-1RA). This means it makes your body’s own glucagon-like peptide-1 hormone, called GLP-1 for short, work better.
Normally when you eat, the body releases the GLP-1 hormone which helps signal to your brain that you are full. Semaglutides enhance this effect, leading to a feeling of fullness, even when you haven’t eaten.
Another role of GLP-1 is to stimulate the body to produce more insulin, a hormone which helps lower the level of glucose (sugar) in the blood. That’s why semaglutides have been used for several years to treat type 2 diabetes.
Wegovy is self-injected once a week. S Becker/Shutterstock How does Wegovy differ from Ozempic?
Like Wegovy, Ozempic is a semaglutide. The way Wegovy and Ozempic work in the body are essentially the same. They’re made by the same pharmaceutical company, Novo Nordisk.
But there are two differences:
1) They are approved for two different (but related) reasons.
In Australia (and the United States), Ozempic is approved for use to improve blood glucose levels in adults with type 2 diabetes. By managing blood glucose levels effectively, the medication aims to reduce the risk of major complications, such as heart disease.
Wegovy is approved for use alongside diet and exercise for people with a body mass index (BMI) of 30 or greater, or 27 or greater but with other conditions such as high blood pressure.
Wegovy can also be used in people aged 12 years and older. Like Ozempic, Wegovy aims to reduce the risk of future health complications, including heart disease.
2) They are both injected but come in different strengths.
Ozempic is available in pre-loaded single-dose pens with varying dosages of 0.25 mg, 0.5 mg, 1 mg, or 2 mg per injection. The dose can be slowly increased, up to a maximum of 2 mg per week, if needed.
Wegovy is available in prefilled single-dose pens with doses of 0.25 mg, 0.5 mg, 1 mg, 1.7 mg, or 2.4 mg. The treatment starts with a dose of 0.25 mg once weekly for four weeks, after which the dose is gradually increased until reaching a maintenance dose of 2.4 mg weekly.
While it’s unknown what the impact of Wegovy’s introduction will be on Ozempic’s availability, Ozempic is still anticipated to be in low supply for the remainder of 2024.
Is Wegovy effective for weight loss?
Given Wegovy is a semaglutide, there is very strong evidence it can help people lose weight and maintain this weight loss.
A recent study found that over four years, participants taking Wevovy as indicated experienced an average weight loss of 10.2% body weight and a reduction in waist circumference of 7.7cm.
For those who stop taking the medication, analyses have shown that about two-thirds of weight lost is regained.
Wegovy can help people lose weight and maintain their weight loss – while they take the drug. Mladen Mitrinovic/Shutterstock What are the side effects of Wegovy?
The most common side effects are nausea and vomiting.
However, other serious side effects are also possible because of the whole-of-body impact of the medication. Thyroid tumours and cancer have been detected as a risk in animal studies, yet are rarely seen in human scientific literature.
In the four-year Wegovy trial, 16.6% of participants who received Wegovy (1,461 people) experienced an adverse event that led to them permanently discontinuing their use of the medication. This was higher than the 8.2% of participants (718 people) who received the placebo (with no active ingredient).
Side effects included gastrointestinal disorders (including nausea and vomiting), which affected 10% of people who used Wegovy compared to 2% of people who used the placebo.
Gallbladder-related disorders occurred in 2.8% of people who used Wegovy, and 2.3% of people who received the placebo.
Recently, concerns about suicidal thoughts and behaviours have been raised, after a global analysis reviewed more than 36 million reports of adverse events from semaglutide (Ozempic or Wegovy) since 2000.
There were 107 reports of suicidal thoughts and self-harm among people taking semaglutide, sadly including six actual deaths. When people stopped the medication, 62.5% found the thoughts went away. What we don’t know is whether dose, weight loss, or previous mental health status or use of antidepressants had a role to play.
Finally, concerns are growing about the negative effect of semaglutides on our social and emotional connection with food. Anecdotal and scientific evidence suggests people who use semaglutides significantly reduce their daily dietary intake (as anticipated) by skipping meals and avoiding social occasions – not very enjoyable for people and their loved ones.
How can people access Wegovy?
Wegovy is available for purchase at pharmacists with a prescription from a doctor.
But there is a hefty price tag. Wegovy is not currently subsidised through the Pharmaceutical Benefits Scheme, leaving patients to cover the cost. The current cost is estimated at around A$460 per month dose.
If you’re considering Wegovy, make an appointment with your doctor for individual advice.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
From straight to curly, thick to thin: here’s how hormones and chemotherapy can change your hair
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Head hair comes in many colours, shapes and sizes, and hairstyles are often an expression of personal style or cultural identity.
Many different genes determine our hair texture, thickness and colour. But some people’s hair changes around the time of puberty, pregnancy or after chemotherapy.
So, what can cause hair to become curlier, thicker, thinner or grey?
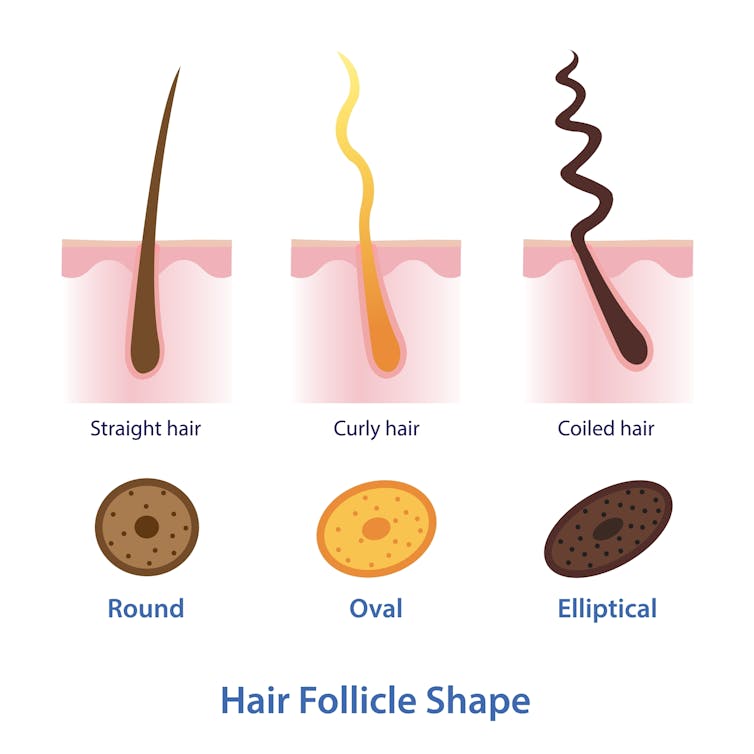
Curly or straight? How hair follicle shape plays a role
Hair is made of keratin, a strong and insoluble protein. Each hair strand grows from its own hair follicle that extends deep into the skin.
Curly hair forms due to asymmetry of both the hair follicle and the keratin in the hair.
Follicles that produce curly hair are asymmetrical and curved and lie at an angle to the surface of the skin. This kinks the hair as it first grows.
The asymmetry of the hair follicle also causes the keratin to bunch up on one side of the hair strand. This pulls parts of the hair strand closer together into a curl, which maintains the curl as the hair continues to grow.
Follicles that are symmetrical, round and perpendicular to the skin surface produce straight hair.
Each hair strand grows from its own hair follicle.
Mosterpiece/ShutterstockLife changes, hair changes
Our hair undergoes repeated cycles throughout life, with different stages of growth and loss.
Each hair follicle contains stem cells, which multiply and grow into a hair strand.
Head hairs spend most of their time in the growth phase, which can last for several years. This is why head hair can grow so long.
Let’s look at the life of a single hair strand. After the growth phase is a transitional phase of about two weeks, where the hair strand stops growing. This is followed by a resting phase where the hair remains in the follicle for a few months before it naturally falls out.
The hair follicle remains in the skin and the stems cells grow a new hair to repeat the cycle.
Each hair on the scalp is replaced every three to five years.
Each hair on the scalp is replaced every three to five years.
Just Life/ShutterstockHormone changes during and after pregnancy alter the usual hair cycle
Many women notice their hair is thicker during pregnancy.
During pregnancy, high levels of oestrogen, progesterone and prolactin prolong the resting phase of the hair cycle. This means the hair stays in the hair follicle for longer, with less hair loss.
A drop in hormones a few months after delivery causes increased hair loss. This is due to all the hairs that remained in the resting phase during pregnancy falling out in a fairly synchronised way.
Hair can change around puberty, pregnancy or after chemotherapy
This is related to the genetics of hair shape, which is an example of incomplete dominance.
Incomplete dominance is when there is a middle version of a trait. For hair, we have curly hair and straight hair genes. But when someone has one curly hair gene and one straight hair gene, they can have wavy hair.
Hormonal changes that occur around puberty and pregnancy can affect the function of genes. This can cause the curly hair gene of someone with wavy hair to become more active. This can change their hair from wavy to curly.
Researchers have identified that activating specific genes can change hair in pigs from straight to curly.
Chemotherapy has very visible effects on hair. Chemotherapy kills rapidly dividing cells, including hair follicles, which causes hair loss. Chemotherapy can also have genetic effects that influence hair follicle shape. This can cause hair to regrow with a different shape for the first few cycles of hair regrowth.
Your hair can change at different stages of your life.
Igor Ivakhno/ShutterstockHormonal changes as we age also affect our hair
Throughout life, thyroid hormones are essential for production of keratin. Low levels of thyroid hormones can cause dry and brittle hair.
Oestrogen and androgens also regulate hair growth and loss, particularly as we age.
Balding in males is due to higher levels of androgens. In particular, high dihydrotestosterone (sometimes shortened to DHT), which is produced in the body from testosterone, has a role in male pattern baldness.
Some women experience female pattern hair loss. This is caused by a combination of genetic factors plus lower levels of oestrogen and higher androgens after menopause. The hair follicles become smaller and smaller until they no longer produce hairs.
Reduced function of the cells that produce melanin (the pigment that gives our hair colour) is what causes greying.
Theresa Larkin, Associate professor of Medical Sciences, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: