Shame and blame can create barriers to vaccination
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Understanding the stigma surrounding infectious diseases like HIV and mpox may help community health workers break down barriers that hinder access to care.
Looking back in history can provide valuable lessons to confront stigma in health care today, especially toward Black, Latine, LGBTQ+, and other historically underserved communities disproportionately affected by COVID-19 and HIV.
Public Good News spoke with Sam Brown, HIV prevention and wellness program manager at Civic Heart, a community-based organization in Houston’s historic Third Ward, to understand the effects of stigma around sexual health and vaccine uptake.
Brown shared more about Civic Heart’s efforts to provide free confidential testing for sexually transmitted infections, counseling and referrals, and information about COVID-19, flu, and mpox vaccinations, as well as the lessons they’re learning as they strive for vaccine equity.
Here’s what Brown said.
[Editor’s note: This content has been edited for clarity and length.]
PGN: Some people on social media have spread the myth that vaccines cause AIDS or other immune deficiencies when the opposite is true: Vaccines strengthen our immune systems to help protect against disease. Despite being frequently debunked, how do false claims like these impact the communities you serve?
Sam Brown: Misinformation like that is so hard to combat. And it makes the work and the path to overall community health hard because people will believe it. In the work that we do, 80 percent of it is changing people’s perspective on something they thought they knew.
You know, people don’t even transmit AIDS. People transmit HIV. So, a vaccine causing immunodeficiency doesn’t make sense.
With the communities we serve, we might have a person that will believe the myth, and because they believe it, they won’t get vaccinated. Then later, they may test positive for COVID-19.
And depending on social determinants of health, it can impact them in a whole heap of ways: That person is now missing work, they’re not able to provide for their family—if they have a family. It’s this mindset that can impact a person’s life, their income, their ability to function.
So, to not take advantage of something like a vaccine that’s affordable, or free for the most part, just because of misinformation or a misunderstanding—that’s detrimental, you know.
For example, when we talk to people in the community, many don’t know that they can get mpox from their pet, or that it’s zoonotic—that means that it can be transferred between different species or different beings, from animals to people. I see a lot of surprise and shock [when people learn this].
It’s difficult because we have to fight the misinformation and the stigma that comes with it. And it can be a big barrier.
People misunderstand. [They] think that “this is something that gay people or the LGBTQ+ community get,” which is stigmatizing and comes off as blaming. And blaming is the thing that leads us to be misinformed.
PGN: In the last couple years, your organization’s HIV Wellness program has taken on promoting COVID-19, flu, and mpox vaccines to the communities you serve. How do you navigate conversations between sexual health and infectious diseases? Can you share more about your messaging strategies?
S.B.: As we promoted positive sexual health and HIV prevention, we saw people were tired of hearing about HIV. They were tired of hearing about how PrEP works, or how to prevent HIV.
But, when we had an outbreak of syphilis in Houston just last year, people were more inclined to test because of the severity of the outbreak.
So, what our team learned is that sometimes you have to change the message to get people what they need.
We changed our message to highlight more syphilis information and saw that we were able to get more people tested for HIV because we correlated how syphilis and HIV are connected and how a person can be susceptible to both.
Using messages that the community wants and pairing them with what the community needs has been better for us. And we see that same thing with COVID-19, the flu, and RSV. Sometimes you just can’t be married to a message. We’ve had to be flexible to meet our clients where they are to help them move from unsafe practices to practices that are healthy and good for them and their communities.
PGN: You’ve mentioned how hard it is to combat stigma in your work. How do you effectively address it when talking to people one-on-one?
S.B.: What I understand is that no one wants to feel shame. What I see people respond to is, “Here’s an opportunity to do something different. Maybe there was information that you didn’t know that caused you to make a bad decision. And now here’s an opportunity to gain information so that you can make a better decision.”
People want to do what they want to do; they want to live how they want to live. And we all should be able to do that as long as it’s not hurting anyone, but also being responsible enough to understand that, you know, COVID-19 is here.
So, instead of shaming and blaming, it’s best to make yourself aware and understand what it is and how to treat it. Because the real enemy is the virus—it’s the infection, not the people.
When we do our work, we want to make sure that we come from a strengths-based approach. We always look at what a client can do, what that client has. We want to make sure that we’re empowering them from that point. So, even if they choose not to prioritize our message right now, we can’t take that personally. We’ll just use it as a chance to try a new way of framing it to help people understand what we’re trying to say.
And sometimes that can be difficult, even for organizations. But getting past that difficulty comes with a greater opportunity to impact someone else.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Twenty-One, No Wait, Twenty Tweaks For Better Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Greger’s 21 Tweaks… We say 20, though!
We’ve talked before about Dr. Greger’s Daily Dozen (12 things he advises that we make sure to eat each day, to enjoy healthy longevity), but much less-talked-about are his “21 Tweaks”…
They are, in short, a collection of little adjustments one can make for better health. Some of them are also nutritional, but many are more like lifestyle tweaks. Let’s do a rundown:
At each meal:
- Preload with water
- Preload with “negative calorie” foods (especially: greens)
- Incorporate vinegar (1-2 tbsp in a glass of water will slow your blood sugar increase)
- Enjoy undistracted meals
- Follow the 20-minute rule (enjoy your meal over the course of at least 20 minutes)
Get your daily doses:
- Black cumin ¼ tsp
- Garlic powder ¼ tsp
- Ground ginger (1 tsp) or cayenne pepper (½ tsp)
- Nutritional yeast (2 tsp)
- Cumin (½ tsp)
- Green tea (3 cups)
Every day:
- Stay hydrated
- Deflour your diet
- Front-load your calories (this means implementing the “king, prince, pauper” rule—try to make your breakfast the largest meal of your day, followed my a medium lunch, and a small evening meal)
- Time-restrict your eating (eat your meals within, for example, an 8-hour window, and fast the rest of the time)
- Optimize exercise timing (before breakfast is best for most people, unless you are diabetic)
- Weigh yourself twice a day (doing this when you get up and when you go to bed results in much better long-term weight management than weighing only once per day)
- Complete your implementation intentions (this sounds a little wishy-washy, but it’s about building a set of “if this, then that” principles, and then living by them. An example could be directly physical health-related such as “if there is a choice of stairs or elevator, I will take the stairs”, or could be more about holistic good-living, such as “if someone asks me for help, I will try to oblige them so far as I reasonably can”)
Every night:
- Fast after 7pm
- Get sufficient sleep (7–9 hours is best. As we get older, we tend more towards the lower end of that, but try get at least those 7 hours!)
Experiment with Mild Trendelenburg(better yet, skip this one)*
*This involves a 6º elevation of the bed, at the foot end. Dr. Greger advises that this should only be undertaken after consulting your doctor, though, as a lot of health conditions can contraindicate it. We at 10almonds couldn’t find any evidence to support this practice, and numerous warnings against it, so we’re going to go ahead and say we think this one’s skippable.
Again, we do try to bring you the best evidence-based stuff here at 10almonds, and we’re not going to recommend something just because of who suggested it
As for the rest, you don’t have to do them all! And you may have noticed there was a little overlap in some of them. But, we consider them a fine menu of healthy life hacks from which to pick and choose!
Share This Post
-
The 6 Dimensions Of Sleep (And Why They Matter)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Good Is Your Sleep, Really?
This is Dr. Marie-Pierre St-Onge, Director of Columbia University’s Center of Excellence for Sleep and Circadian Research.
The focus of Dr. St-Onge’s research is the study of the impact of lifestyle, especially sleep and diet, on cardio-metabolic risk factors.
She conducts clinical research combining her expertise on sleep, nutrition, and energy regulation.
What kind of things do her studies look at?
Her work focuses on questions about…
- The role of circadian rhythms (including sleep duration and timing)
- Meal timing and eating patterns
…and their impact on cardio-metabolic risk.
What does she want us to know?
First things first, when not to worry:
❝Getting a bad night’s sleep once in a while isn’t anything to worry about. That’s what we would describe as transient insomnia. Chronic insomnia occurs when you spend three months or more without regular sleep, and that is when I would start to be concerned.❞
But… as prevention is (as ever) better than cure, she also advises that we do pay attention to our sleep! And, as for how to do that…
The Six Dimensions of Sleep
One useful definition of overall sleep health is the RU-Sated framework, which assesses six key dimensions of sleep that have been consistently associated with better health outcomes. These are:
- regularity
- satisfaction with sleep
- alertness during waking hours
- timing of sleep
- efficiency of sleep
- duration of sleep
You’ll notice that some of these things you can only really know if you use a sleep-monitoring app. She does recommend the use of those, and so do we!
We reviewed and compared some of the most popular sleep-monitoring apps! You can check them out here: Time For Some Pillow Talk
You also might like…
We’re not all the same with regard to when is the best time for us to sleep, so:
Use This Sleep Cycle Calculator To Figure Out the Optimal Time for You To Go to Bed and Wake Up
AROUND THE WEB
What’s happening in the health world…
- Aspirin may make your breathing worse
- Taking naps for more than 30 minutes may raise your metabolic disease risk
- How to ease back into exercise after surgery
- Study provides evidence that breathing exercises may reduce your Alzheimer’s risk
- No one in movies knows how to swallow a pill
More to come tomorrow!
Share This Post
-
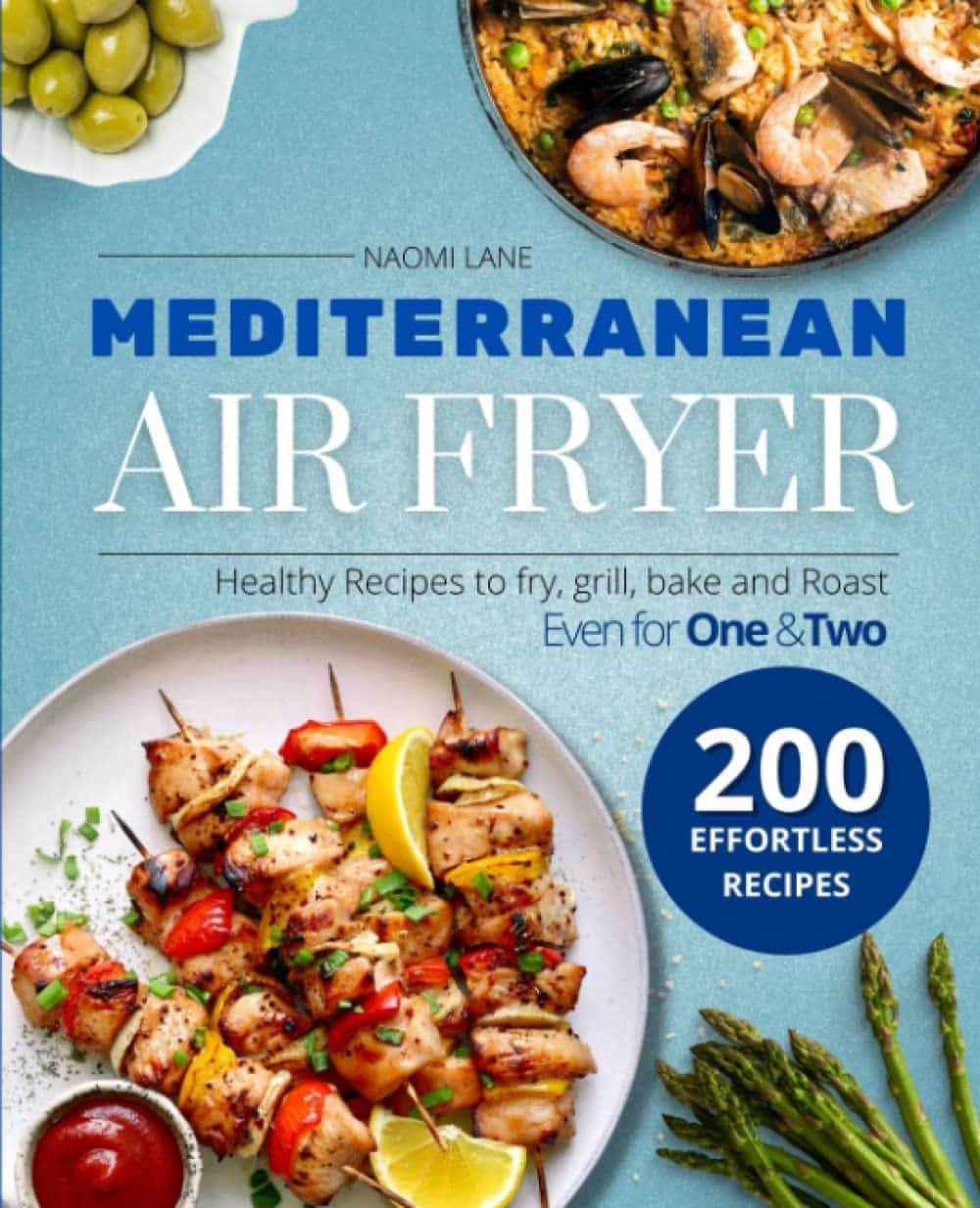
Mediterranean Air Fryer Cookbook – by Naomi Lane
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are Mediterranean Diet cookbooks, and there are air fryer cookbooks. And then there are (a surprisingly large intersection of!) Mediterranean Diet air fryer cookbooks. We wanted to feature one of them in today’s newsletter… And as part of the selection process, looked through quite a stack of them, and honestly, were quite disappointed with many. This one, however, was one of the ones that stood out for its quality of both content and clarity, and after a more thorough reading, we now present it to you:
Naomi Lane is a professional dietician, chef, recipe developer, and food writer… And it shows, on all counts.
She covers what the Mediterranean diet is, and she covers far more than this reviewer knew it was even possible to know about the use of an air fryer. That alone would make the book a worthy purchase already.
The bulk of the book is the promised 200 recipes. They cover assorted dietary requirements (gluten-free, dairy-free, etc) while keeping to the Mediterranean Diet.
The recipes are super clear, just what you need to know, no reading through a nostalgic storytime first to find things. Also no pictures, which will be a plus for some readers and a minus for others. The recipes also come complete with nutritional information for each meal (including sodium), so you don’t have to do your own calculations!
Bottom line: this is the Mediterranean Diet air fryer cook book. Get it, thank us later!
Get your copy of “Mediterranean Air Fryer Cookbook” on Amazon today!
Share This Post
Related Posts
-
Keep Your Wits About You – by Dr. Vonetta Dotson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Dotson sets out to provide the reader with the tools to maintain good brain health at any age, though she does assume the reader to be in midlife or older.
She talks us through the most important kinds of physical activity, mental activity, and social activity, as well as a good grounding in brain-healthy nutrition, and how to beat the often catch-22 situation of poor sleep.
If you are the sort of person who likes refreshers on what you have just read, you’ll enjoy that the final two chapters repeat the information from chapters 2–6. If not, then well, if you skip the final 2 chapters the book will be 25% shorter without loss of content.
The style is enthusiastic; when it comes to her passion for the brain, Dr. Dotson both tells and shows, in abundance. While some authors may take care to break down the information in a way that can be understood from skimming alone, Dr. Dotson assumes that the reader’s interest will match hers, and thus will not mind a lot of lengthy prose with in-line citations. So, provided that’s the way you like to read, it’ll suit you too.
Bottom line: if you are looking for a book on maintaining optimal brain health that covers the basics without adding advice that is out of the norm, then this is a fine option for that!
Click here to check out Keep Your Wits About You, and keep your wits about you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Superfood Energy Balls
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
They are healthy, they are tasty, they are convenient! Make some of these and when you need an energizing treat at silly o’clock when you don’t have time to prepare something, here they are, full of antioxidants, vitamins and minerals, good for blood sugars too, and ready to go:
You will need
- 1 cup pitted dates
- 1 cup raw mixed nuts
- ¼ cup goji berries
- 1 tbsp cocoa powder
- 1 tsp chili flakes
Naturally, you can adjust the spice level if you like! But this is a good starter recipe.
Method
(we suggest you read everything at least once before doing anything)
1) Blend all the ingredients in a good processor to make a dough
2) Roll the dough into 1″ balls; you should have enough dough for about 16 balls. If you want them to be pretty, you can roll them in some spare dry ingredients (e.g. chopped nuts, goji berries, chili flakes, seeds of some kind, whatever you have in your kitchen that fits the bill).
3) Refrigerate for at least 1–2 hours, and serve! They can also be kept in the fridge for at least a good while—couldn’t tell you how long for sure though, because honestly, they’ve never stayed that long in the fridge without being eaten.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Dates vs Figs – Which is Healthier?
- Why You Should Diversify Your Nuts!
- Goji Berries: Which Benefits Do They Really Have?
- The Sugary Food That Lowers Blood Sugars
- Enjoy Bitter Foods For Your Heart & Brain
- Capsaicin’s Hot Benefits
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Carrots vs Parsnips – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing carrots to parsnips, we picked the parsnips.
Why?
There are arguments for both! But we say parsnips win on overall nutritional density.
In terms of macros, parsnips vary quite a lot from region to another, but broadly speaking, parsnips have more carbs and fiber, and/but the ratios are such that carrots have the lower glycemic index. We’ll call this one a win for carrots.
When it comes to vitamins, carrots have more of vitamins A, B2, B3, B6, and choline, while parsnips have more of vitamins B1, B5, B9, C, E, and K. A small win for parsnips here.
In the category of minerals, carrots are not higher in any minerals, while parsnips are higher in calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. An overwhelming win for parsnips.
While the overall vitamin and mineral content puts parsnips ahead, it’s still worth noting that carrots have highly bioavailable megadoses of vitamin A.
Another thing to note is that the glycemic index recorded for both is when peeled and boiled, whereas both of these root vegetables can be enjoyed raw if you wish, which has a much lower GI.
In short, enjoy either or both, but parsnips are the more nutritionally dense overall.
Want to learn more?
You might like to read:
Glycemic Index vs Glycemic Load vs Insulin Index
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: