Semaglutide’s Surprisingly Unexamined Effects
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Semaglutide’s Surprisingly Big Research Gap
GLP-1 receptor agonists like Ozempic, Wegovy, and other semaglutide drugs. are fast becoming a health industry standard go-to tool in the weight loss toolbox. When it comes to recommending that patients lose weight, “Have you considered Ozempic?” is the common refrain.
Sometimes, this may be a mere case of kicking the can down the road with regard to some other treatment that it can be argued (sometimes even truthfully) would go better after some weight loss:
How weight bias in health care can harm patients with obesity: Research
…which we also covered in fewer words in the second-to-last item here:
But GLP-1 agonists work, right?
Yes, albeit there’s a litany of caveats, top of which are usually:
- there are often adverse gastrointestinal side effects
- if you stop taking them, weight regain generally ensues promptly
For more details on these and more, see:
…but now there’s another thing that’s come to light:
The dark side of semaglutide’s weight loss
In academia, “dark” is often used to describe “stuff we don’t have much (or in some cases, any) direct empirical evidence of, but for reasons of surrounding things, we know it’s there”.
Well-known examples include “dark matter” in physics and the Dark Ages in (European) history.
In the case of semaglutide and weight loss, a review by a team of researchers (Drs. Sandra Christenen, Katie Robinson, Sara Thomas, and Dominique Williams) has discovered how little research has been done into a certain aspect of GLP-1 agonist’s weight loss effects, namely…
Dietary changes!
There’s been a lot of popular talk about “people taking semaglutide eat less”, but it’s mostly anecdotal and/or presumed based on parts of the mechanism of action (increasing insulin production, reducing glucagon secretions, modulating dietary cravings).
Where studies have looked at dietary changes, it’s almost exclusively been a matter of looking at caloric intake (which has been found to be a 16–39% reduction), and observations-in-passing that patients reported reduction in cravings for fatty and sweet foods.
This reduction in caloric intake, by the way, is not significantly different to the reduction brought about by counselling alone (head-to-head studies have been done; these are also discussed in the research review).
However! It gets worse. Very few studies of good quality have been done, even fewer (two studies) actually had a registered dietitian nutritionist on the team, and only one of them used the “gold standard” of nutritional research, the 24-hour dietary recall test. Which, in case you’re curious, you can read about what that is here:
Dietary Assessment Methods: What Is A 24-Hour Recall?
Of the four studies that actually looked at the macros (unlike most studies), they found that on average, protein intake decreased by 17.1%. Which is a big deal!
It’s an especially big deal, because while protein’s obviously important for everyone, it’s especially important for anyone trying to lose weight, because muscle mass is a major factor in metabolic base rate—which in turn is much important for fat loss/maintenance than exercise, when it comes to how many calories we burn by simply existing.
A reasonable hypothesis, therefore, is that one of the numerous reasons people who quit GLP-1 agonists immediately put fat back on, is because they probably lost muscle mass in amongst their weight loss, meaning that their metabolic base rate will have decreased, meaning that they end up more disposed to put on fat than before.
And, that’s just a hypothesis and it’s a hypothesis based on very few studies, so it’s not something to necessarily take as any kind of definitive proof of anything, but it is to say—as the researchers of this review do loudly say—more research needs to be done into this, because this has been a major gap in research so far!
Any other bad news?
While we’re talking research gaps, guess how many studies looked into micronutrient intake changes in people taking GLP-1 agonists?
If you guessed zero, you guessed correctly.
You can find the paper itself here:
What’s the main take-away here?
On a broad, scoping level: we need more research!
On a “what this means for individuals who want to lose weight” level: maybe we should be more wary of this still relatively new (less than 10 years old) “wonder drug”. And for most of those 10 years it’s only been for diabetics, with weight loss use really being in just the past few years (2021 onwards).
In other words: not necessarily any need to panic, but caution is probably not a bad idea, and natural weight loss methods remain very reasonable options for most people.
See also: How To Lose Weight (Healthily!)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Caramelized Caraway Cabbage
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cabbage is an underrated vegetable for its many nutrients and its culinary potential—here’s a great way to make it a delectable starter or respectable side.
You will need
- 1 medium white cabbage, sliced into 1″ thick slabs
- 1 tbsp extra-virgin olive oil
- 1 tbsp caraway seeds
- 1 tsp black pepper
- ½ tsp turmeric
- ¼ tsp MSG or ½ tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 400℉ / 200℃.
2) Combine the non-cabbage ingredients in a small bowl, whisking to mix thoroughly—with a tiny whisk if you have one, but a fork will work if necessary.
3) Arrange the cabbage slices on a lined baking tray and brush the seasoning-and-oil mixture over both sides of each slice.
4) Roast for 20–25 minutes until the cabbage is tender and beginning to caramelize.
5) Serve warm.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Curcumin (Turmeric) is worth its weight in gold
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Avocado Oil vs Olive Oil – Which is Healthier?
Take care!
Share This Post
-
Dates vs Banana – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing dates to banana, we picked the dates.
Why?
It was close, and bananas do have some strengths too! We pitted these two against each other as they’re both sweet fruits often used as a sweetening and consistency-altering ingredient in desserts and sweet snacks, so if you’re making a choice between them, here are the things to consider:
In terms of macros, dates have more than 3x the fiber, more than 2x the protein, and a little over 3x the carbs. You may be wondering how this adds up in terms of glycemic index: dates have the lower GI. So, we pick dates, here, for that reason and overall nutritional density too.
When it comes to vitamins, bananas have their moment, albeit barely: dates have more of vitamins B1, B3, B5, and K, while bananas have more of vitamins A, B6, C, E, and choline, making for a marginal victory for bananas in this category.
Looking at minerals next, however, it’s quite a different story: dates have more calcium, copper, iron, magnesium, phosphorus, potassium, selenium, and zinc, while bananas are not higher in any mineral. No, not even potassium, for which they are famous—dates have nearly 2x more potassium than bananas.
Adding up these sections makes for a clear win for dates in general!
Enjoy either/both, but dates are the more nutritious snack/ingredient.
Want to learn more?
You might like to read:
From Apples to Bees, and High-Fructose Cs: Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Share This Post
-
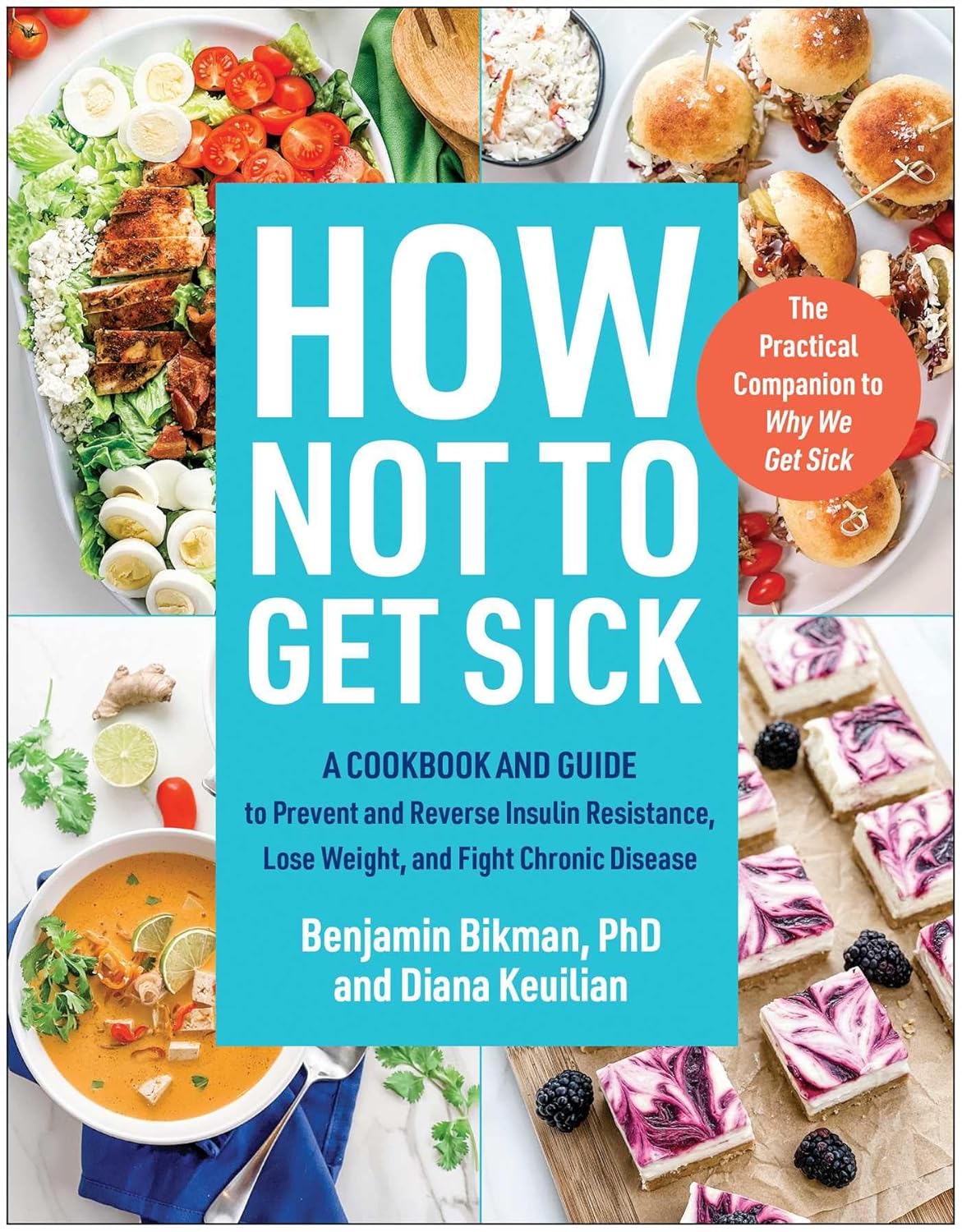
How Not To Get Sick: A Cookbook – by Dr. Benjamin Bikman and Diana Keuilian
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Dr. Bikman’s excellent “Why We Get Sick”, and if you haven’t read that yet, we recommend doing so.
Nevertheless, you don’t need to have read it to benefit from this one, which is about cooking with those learnings (from the other book) in mind.
Before getting to the recipes, we get a section recapping what we learned previously, as well as adding some more general lifestyle advices beyond the kitchen. The science is also expanded a bit, to include such things as the two-way relationship between insulin and aging, as well as the interplay with other metrics of health, including blood lipids, for example.
The authors then provide a plan, in the three stages: reverse (insulin resistance), prevent (insulin resistance), maintain (insulin sensitivity).
The recipes themselves, of which there are 70, are of course tailored to do the above three things; they’re also quite diverse, albeit if you are vegetarian or vegan, you should know in advance that most of these recipes are not.
Bottom line: if the above doesn’t apply to you, and you would like to improve your insulin sensitivity, this book can indeed help.
Share This Post
Related Posts
-
Chickpeas vs Black-Eyed Peas – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing chickpeas to black-eyed peas, we picked the chickpeas.
Why?
In terms of macros, chickpeas have more protein, carbs, and fiber, the ratio of the latter two also giving them the lower glycemic index. An easy win for chickpeas.
In the category of vitamins, chickpeas have more of vitamins B2, B6, C, E, K, and choline, while black-eyed peas have more of vitamins B1, B5, and B9. Another victory for chickpeas.
When it comes to minerals, things are even more pronounced: chickpeas have more calcium, copper, iron, manganese, phosphorus, potassium, selenium, and zinc, while black-eyed peas have (barely) more magnesium. An overwhelming win for chickpeas.
Adding up the sections makes for a very evident overall win for chickpeas; as ever, do enjoy either or both though; diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Mindfulness – by Olivia Telford
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Olivia Telford takes us on a tour of mindfulness, meditation, mindfulness meditation, and how each of these things impacts stress, anxiety, and depression—as well as less obvious things too, like productivity and relationships.
In the category of how much this is a “how-to-” guide… It’s quite a “how-to” guide. We’re taught how to meditate, we’re taught assorted mindfulness exercises, and we’re taught specific mindfulness interventions such as beating various life traps (e.g. procrastination, executive dysfunction, etc) with mindfulness.
The writing style is simple and to the point, explanatory and very readable. References are made to pop-science and hard science alike, and all in all, is not too far from the kind of writing you might expect to find here at 10almonds.
Bottom line: if you’d like to practice mindfulness meditation and want an easy “in”, or perhaps you’re curious and wonder what mindfulness could tangibly do for you and how, then this book is a great choice for that.
Click here to check out Mindfulness, and enjoy being more present in life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pine Nuts vs Peanuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pine nuts to peanuts, we picked the pine nuts.
Why?
An argument could be made for either, honestly, as it depends on what we prioritize the most. These are both very high-calorie foods, and/but are far from empty calories, as they both contain main nutrients. Obviously, if you are allergic to nuts, this one is just not a comparison for you, sorry.
Looking at the macros first, peanuts are higher in protein, carbs, and fiber, while pine nuts are higher in fats—though the fats are healthy, being mostly polyunsaturated, with about a third of the total fats monounsaturated, and a low amount of saturated fat (peanuts have nearly 2x the saturated fat). On balance, we’ll call the macros category a moderate win for peanuts, though.
In terms of vitamins, peanuts have more of vitamins B1, B3, B5, B6, and B9, while pine nuts have more of vitamins A, B2, C, E, K, and choline. All in all, a marginal win for pine nuts.
In the category of minerals, peanuts have more calcium and selenium, while pine nuts have more copper, iron, magnesium, manganese, phosphorus, and zinc. An easy win for pine nuts, even before we take into account that peanuts have nearly 10x as much sodium. And yes, we are talking about the raw nuts, not nuts that have been roasted and salted.
Adding up the categories gives a win for pine nuts—but if you have certain particular priorities, you might still prefer peanuts for the areas in which peanuts are stronger.
Of course, the best solution is to enjoy both!
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: