Ruminating vs Processing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to traumatic experiences, there are two common pieces of advice for being able to move forwards functionally:
- Process whatever thoughts and feelings you need to process
- Do not ruminate
The latter can seem, at first glance, a lot like the former. So, how to tell them apart, and how to do one without the other?
Getting tense
One major difference between the two is the tense in which our mental activity takes place:
- processing starts with the traumatic event (or perhaps even the events leading up to the traumatic event), analyses what happened and if possible why, and then asks the question “ok, what now?” and begins work on laying out a path for the future.
- rumination starts with the traumatic event (or perhaps even the events leading up to the traumatic event), analyses what happened and if why, oh why oh why, “I was such an idiot, if only I had…” and gets trapped in a fairly tight (and destructive*) cycle of blame and shame/anger, never straying far from the events in question.
*this may be directly self-destructive, but it can also sometimes be only indirectly self-destructive, for example if the blame and anger is consciously placed with someone else.
This idea fits in, by the way, with Dr. Elisabeth Kübler-Ross’s “five stages of grief” model; rumination here represents the stages “bargaining”, “despair”, and “anger”, while emotional processing here represents the stage “acceptance”. Thus, it may be that rumination does have a place in the overall process—just don’t get stuck there!
For more on healthily processing grief specifically:
What Grief Does To The Body (And How To Manage It)
Grief, by the way, can be about more than the loss of a loved one; a very similar process can play out with many other kinds of unwanted life changes too.
What are the results?
Another way to tell them apart is to look at the results of each. If you come out of a long rumination session feeling worse than when you started, it’s highly unlikely that you just stopped too soon and were on the verge of some great breakthrough. It’s possible! But not likely.
- Processing may be uncomfortable at first, and if it’s something you’ve ignored for a long time, that could be very uncomfortable at first, but there should quite soon be some “light at the end of the tunnel”. Perhaps not even because a solution seems near, but because your mind and body recognize “aha, we are doing something about it now, and thus may find a better way forward”.
- Rumination tends to intensify and prolong uncomfortable emotions, increases stress and anxiety, and likely disrupts sleep. At best, it may serve as a tipping point to seek therapy or even just recognize “I should figure out a way to deal with this, because this isn’t doing me any good”. At worst, it may serve as a tipping point to depression, and/or substance abuse, and/or suicidality.
See also: How To Stay Alive (When You Really Don’t Want To) ← which also has a link back to our article on managing depression, by the way!
Did you choose it, really?
A third way to tell them apart is the level of conscious decision that went into doing it.
- Processing is almost always something that one decides “ok, let’s figure this out”, and sits down to figure it out.
- Rumination tends to be about as voluntary as social media doomscrolling. Technically we may have decided to begin it (we also might not have made any conscious decision, and just acted on impulse), but let’s face it, our hands weren’t at the wheel for long, at all.
A good way to make sure that it is a conscious process, is to schedule time for it in advance, and then do it only during that time. If thoughts about it come up at other times, tell yourself “no, leave that for later”, and then deal with it when (and only when) the planned timeslot arrives.
It’s up to you and your schedule what time you pick, but if you’re unsure, consider an hour in the early evening. That means that the business of the day is behind you, but it’s also not right before bed, so you should have some decompression time as a buffer. So for example, perhaps after dinner you might set a timer* for an hour, and sit down to journal, brainstorm, or just plain think, about the matter that needs processing.
*electronic timers can be quite jarring, and may distract you while waiting for the beeps. So, consider investing in a relaxing sand timer like this one instead.
Is there any way to make rumination less bad?
As we mentioned up top, there’s a case to be made for “rumination is an early part of the process that gets us where we need to go, and may not be skippable, or may not be advisable to skip”.
So, if you are going to ruminate, then firstly, we recommend again bordering it timewise (with a timer as above) and having a plan to pull yourself out when you’re done rather than getting stuck there (such as: The Off-Button For Your Brain: How To Stop Negative Thought Spirals).
And secondly, you might want to consider the following technique, which allows one to let one’s brain know that the thing we’re thinking about / imagining is now to be filed away safely; not lost or erased, but sent to the same place that nightmares go after we wake up:
A Surprisingly Powerful Tool: Eye Movement Desensitization & Reprocessing (EMDR)
What if I actually do want to forget?
That’s not usually recommendable; consider talking it through with a therapist first. However, for your interest, there is a way:
The Dark Side Of Memory (And How To Forget)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Trout vs Carp – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing trout to carp, we picked the trout.
Why?
Both have their strong points!
In terms of macros, trout has slightly more protein and fat, and/but also has less cholesterol than carp. So, we pick the trout in the macros category.
In the category of vitamins, trout has much more of vitamins A, B1, B2, B3, B5, B6, B7, B12, C, D, E, K, and choline, while carp has slightly more vitamin B9. In other words, an easy win for trout here.
When it comes to minerals, however, trout has more potassium and selenium, while carp has more calcium, copper, iron, magnesium, manganese, phosphorus, and zinc. A fair win for carp this time.
You may be wondering about heavy metals: this will vary depending on location, as well as the age of the fish (younger fish have had less time to accumulate heavy metals than old ones, so if you’re visiting the fishmonger, choose the smaller ones) and the lives they have led (e.g. wild vs farmed), however, as a general rule of thumb, trout will generally have lower heavy metals levels than carp, all other things (e.g. location, age, etc) being equal.
In short, enjoy either or both in moderation, but trout wins on 3/4 categories today.
Want to learn more?
You might like to read:
Farmed Fish vs Wild Caught: Antibiotics, Mercury, & More
Take care!
Share This Post
-
Anti-Inflammatory Pineapple Fried Rice
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fried rice is not most people’s go-to when one thinks of health food, but this one is. It’s packed with plenty of nutrients, many of which are anti-inflammatory, but the real star is the pineapple (with its high bromelain content and thus particularly potent benefits).
You will need
- 2½ cups cooked wholegrain basmati rice (you can use our Tasty Versatile Rice recipe if you don’t already have leftovers to use)
- 1 cup pineapple chunks
- ½ red onion, diced
- 1 red bell pepper, diced
- ½ cup sweetcorn
- ½ peas
- 3 green onions, chopped
- 2 serrano peppers, chopped (omit if you don’t care for heat)
- 2 tbsp coconut oil
- 1 tbsp grated fresh ginger
- 1 tbsp black pepper, coarse ground
Method
(we suggest you read everything at least once before doing anything)
1) Fry the red onion, serrano peppers, and ginger in the coconut oil over a medium heat, stirring frequently, for about 3 minutes.
2) Add the pineapple, bell pepper, sweetcorn, peas, and black pepper, stirring frequently, for about another 3 minutes.
3) Add the rice, stirring gently but thoroughly, until fully reheated and mixed in.
4) Serve, garnishing with the green onions.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat To Beat Inflammation
- Ginger Does A Lot More Than You Think
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Bromelain vs Inflammation & Much More
Take care!
Share This Post
-
Delicious Quinoa Avocado Bread
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
They’re gluten-free, full of protein and healthy fats, generous with the fiber, easy to make, and tasty too! What’s not to love? Keep this recipe (and its ingredients) handy for next time you want healthy burger buns or similar:
You will need
- 2½ cups quinoa flour
- 2 cups almond flour (if allergic, just substitute more quinoa flour)
- 1 avocado, peeled, pitted, and mashed
- zest and juice of 1 lime
- 2 tbsp ground flaxseed
- 1 tsp baking powder
- ½ tsp MSG or 1 tsp low-sodium salt
- Optional: seeds, oats, or similar for topping the buns
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉/175℃.
2) Mix the flaxseed with ⅓ cup warm water and set aside.
3) Mix, in a large bowl, the quinoa flour and almond flour with the baking powder and the MSG or salt.
4) Mix, in a separate smaller bowl, the avocado and lime.
5) Add the wet ingredients to the dry, slowly, adding an extra ½ cup water as you do, and knead into a dough.
6) Divide the dough into 4 equal portions, each shaped into a ball and then slightly flattened, to create a burger bun shape. If you’re going to add any seeds or similar as a topping, add those now.
7) Bake them in the oven (on a baking sheet lined with baking paper) for 20–25 minutes. You can check whether they’re done the same way you would a cake, by piercing them to the center with a toothpick and seeing whether it comes out clean.
8) Serve when sufficiently cooled.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Gluten: What’s The Truth?
- Why You Should Diversify Your Nuts!
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
Take care!
Share This Post
Related Posts
-
Better Sex Through Mindfulness – by Dr. Lori Brotto
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Female sexuality is such a taboo topic that, if one searches for (ob/gyn professor, women’s health research director, and psychologist) Dr. Brotto’s book on Google or Amazon, it suggests only “lori brotto mindfulness book”. So, for those brave enough to read a book that would have shocked Victorians, what does this one contain?
The focus is on, as the title suggests, better sex, by and for women. That said, it’s mostly because typically women are more likely to experience the problems described in the book; it’s nothing actually intrinsic to womanhood. A man with the same problems could read this book and benefit just the same.
While the book covers many possible problems between the sheets, the overarching theme is problems of the mind, such as:
- Not getting into the mood in the first place
- Losing the mood quickly and easily, such as by becoming distracted
- Difficulty achieving orgasm even when mechanically everything’s delightful
- Physical discomfort creating a barrier to enjoyment
…and yes, that last one is in part mind-stuff too! Though Dr. Brotto isn’t arguing that mindfulness is a panacea, just an incredibly useful tool. And, it’s one she not only explains very well, but also explains from the position of a wealth of scientific evidence… Enough so, that we see a one-star Amazon reviewer from Canada complained that it was too well-referenced! For us, though, it’s what we like to see.
Good science, presented clearly and usefully, giving practical tips that improve people’s lives.
Bottom line: if you’ve ever lost the mood because you got distracted into thinking about taxes or that meeting on Tuesday, this is the book for you.
Click here to check out Better Sex Through Mindfulness—you can thank us later!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
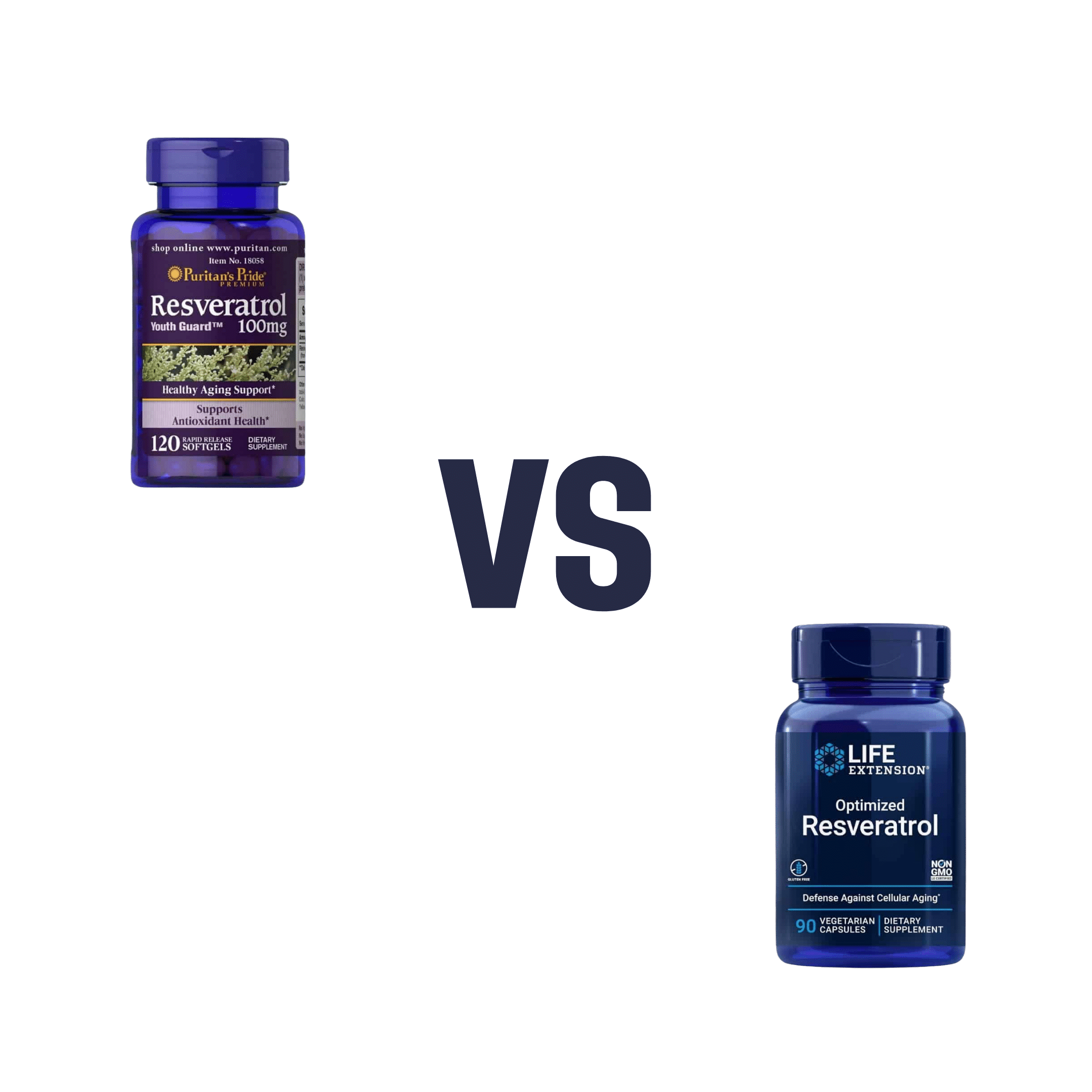
Puritans Pride Resveratrol vs Life Extension Resveratrol – Which is Healthier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Puritan’s Pride Resveratrol to Life Extension Resveratrol, we picked the Life Extension Resveratrol.
Why?
It contains not only more resveratrol per serving (250mg compared to Puritan’s Pride’s 100mg), but also contains other goodies too. Specifically, each capsule also contains:
- Quercetin (150mg)
- Grape & berry blend (85mg)
- Fisetin (10mg)
Whereas the Puritan’s Pride softgels? The other top ingredients are soybean oil and gelatin.
Want to check out the products for yourself? Here they are:
Puritan’s Pride Resveratrol | Life Extension Resveratrol
Want to know more about these supplements? Check out:
Resveratrol & Healthy Aging
Fight Inflammation & Protect Your Brain, With Quercetin
Berries & Other Polyphenol-rich Foods
Fisetin: The Anti-Aging AssassinEnjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Broccoli vs Cabbage – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing broccoli to cabbage, we picked the broccoli.
Why?
Here we go once again pitting two different cultivars of the same species (Brassica oleracea) against each other, and/but once again, there is one that comes out as nutritionally best.
In terms of macros, broccoli has more protein, carbs, and fiber, while they are both low glycemic index foods. The differences are small though, so it’s fairest to call this category a tie.
When it comes to vitamins, broccoli has more of vitamins A, B1, B2, B3, B5, B6, B7, B9, C, E, K, and choline, while cabbage is not higher in any vitamins. It should be noted that cabbage is still good for these, especially vitamins C and K, but broccoli is simply better.
In the category of minerals, broccoli has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while cabbage is not higher in any minerals. Again though, cabbage is still good, especially in calcium, iron, and manganese, but again, broccoli is simply better.
Of course, enjoy either or both! But if you want the nutritionally densest option, it’s broccoli.
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: