What’s behind rising heart attack rates in younger adults
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Deaths from heart attacks have been in decline for decades, thanks to improved diagnosis and treatments. But, among younger adults under 50 and those from communities that have been marginalized, the trend has reversed.
More young people have suffered heart attacks each year since the 2000s—and the reasons why aren’t always clear.
Here’s what you need to know about heart attack trends in younger adults.
Heart attack deaths began declining in the 1980s
Heart disease has been a leading cause of death in the United States for more than a century, but rates have declined for decades as diagnosis and treatments improved. In the 1950s, half of all Americans who had heart attacks died, compared to one in eight today.
A 2023 study found that heart attack deaths declined 4 percent a year between 1999 and 2020.
The downward trend plateaued in the 2000s as heart attacks in young adults rose
In 2012, the decline in heart disease deaths in the U.S. began to slow. A 2018 study revealed that a growing number of younger adults were suffering heart attacks, with women more affected than men. Additionally, younger adults made up one-third of heart attack hospitalizations, with one in five heart attack patients being under 40.
The following year, data showed that heart attack rates among adults under 40 had increased steadily since 2006. Even more troubling, young patients were just as likely to die from heart attacks as patients more than a decade older.
Why are more younger adults having heart attacks?
Heart attacks have historically been viewed as a condition that primarily affects older adults. So, what has changed in recent decades that puts younger adults at higher risk?
Higher rates of obesity, diabetes, and high blood pressure
Several leading risk factors for heart attacks are rising among younger adults.
Between 2009 and 2020, diabetes and obesity rates increased in Americans ages 20 to 44.
During the same period, hypertension, or high blood pressure, rates did not improve in younger adults overall and worsened in young Hispanic people. Notably, young Black adults had hypertension rates nearly twice as high as the general population.
Hypertension significantly increases the risk of heart attack and cardiovascular death in young adults.
Increased substance use
Substance use of all kinds increases the risk of cardiovascular issues, including heart attacks. A recent study found that cardiovascular deaths associated with substance use increased by 4 percent annually between 1999 and 2019.
The rise in substance use-related deaths has accelerated since 2012 and was particularly pronounced among women, younger adults (25-39), American Indians and Alaska Natives, and those in rural areas.
Alcohol was linked to 65 percent of the deaths, but stimulants (like methamphetamine) and cannabis were the substances associated with the greatest increase in cardiovascular deaths during the study period.
Poor mental health
Depression and poor mental health have been linked to cardiovascular issues in young adults. A 2023 study of nearly 600,000 adults under 50 found that depression and self-reported poor mental health are a risk factor for heart disease, regardless of socioeconomic or other cardiovascular risk factors.
Adults under 50 years consistently report mental health conditions at around twice the rate of older adults. Additionally, U.S. depression rates have trended up and reached an all-time high in 2023, when 17.8 percent of adults reported having depression.
Depression rates are rising fastest among women, adults under 44, and Black and Hispanic populations.
COVID-19
COVID-19 can cause real, lasting damage to the heart, increasing the risk of certain cardiovascular diseases for up to a year after infection. Vaccination reduces the risk of heart attack and other cardiovascular events caused by COVID-19 infection.
The first year of the pandemic marked the largest single-year spike in heart-related deaths in five years, including a 14 percent increase in heart attacks. In the second year of the pandemic, heart attacks in young adults increased by 30 percent.
Heart attack prevention
Not every heart attack is preventable, but everyone can take steps to reduce their risks. The American Heart Association recommends managing health conditions that increase heart disease risk, including diabetes, obesity, and high blood pressure.
Lifestyle changes like improving diet, reducing substance use, and increasing physical activity can also help reduce heart attack risk.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Rebuild Your Cartilage
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve covered before the topic of wear-and-tear on joints such as:
Avoiding/Managing Osteoarthritis
But what of cartilage, in particular? A common belief is “once it’s gone, it’s gone”, but that’s not quite right.
Cartilage is living tissue (metabolically active, with living cells). Within this tissue, specialist cells called chondrocytes produce extracellular cartilage matrix and collagen fibers, which provide smooth joint gliding as well as shock absorption.
Is exercise good or bad for cartilage?
Yes, yes it is. Exercise is good or bad for cartilage depending on the details:
- High-impact exercise e.g. running, jumping) places stress on cartilage, which is broadly bad
- However, impact loading strengthens the subchondral bone plate (layer under cartilage)
Strengthening this bone layer can help in long-term adaptation for high-impact sports.
See also: Resistance Is Useful! (Especially As We Get Older)
So, how to do that without wiping out your cartilage first?
Building up
A gradual process is what’s called-for here:
- Start with cyclic, non-impact moderate resistance exercises (e.g. cycling, rowing, swimming).
- Gradually add soft-impact loading (e.g. fast walking, soft jogging).
- Incorporate strength training to improve overall joint stability (e.g. leg press, for lower body joints)
- Slowly transition to running and jumping over a long period to allow tissues to adapt.
How exactly you go about that is a matter of personal taste, but here are some illustrative examples:
- Indoor* cycling
- Cross trainer
- Leg press machine
- Tennis
*Why indoor? It’s so that you can control the resistance level at the twist of a knob, and get on and off when you want.
See also: Treadmill vs Road ← for similar considerations when it comes to walking/running. Outdoor definitely has its advantages, but so does indoor!
And the very related: How To Do HIIT (Without Wrecking Your Body)
Note that HIIT is High Intensity Interval Training, not High Impact Interval Training!
Strength from the inside
One of the most important things for cartilage is collagen. You can supplement that, or if you’re vegetarian/vegan, you can take its constituent parts to improve your own synthesis of it.
See: Collagen For Your Skin, Joints, & Bones: We Are Such Stuff As Fish Are Made Of
Another supplement that can be helpful is glucosamine & chondroitin, which is best taken alongside a good omega-3 intake:
Want to know more?
This book is technically about (re)building strength and mobility in the case of arthritis specifically, but if your joints have more wear than you’d like, you may find this one an invaluable resource:
Take care!
Share This Post
-
General Tso’s Chickpeas
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A fiber-rich, heart-healthy take on a classic:
You will need
- 1 can chickpeas, drained
- ¾ cup vegetable stock; ideally you made this yourself from vegetable cuttings that you kept in the freezer for this purpose, but failing that, you should be able to get low-sodium stock cubes at your local supermarket.
- ¼ cup arrowroot starch (cornstarch will do at a pinch, but arrowroot is better and has no flavor of its own)
- 3 tbsp coconut oil
- 2 tbsp grated fresh ginger
- ¼ bulb garlic, minced
- 2 tbsp honey (or maple syrup if you prefer, and if you don’t like sweetness, reduce this to 1 tbsp or even omit entirely, though it won’t be quite so “General Tso” if you do, but it’s your meal!)
- 2 tbsp tomato paste
- 2 tsp hot sauce
- 1 tsp black pepper, coarse ground
- 3 green onions, sliced
Method
(we suggest you read everything at least once before doing anything)
1) Coat the chickpeas in the arrowroot starch by tossing them together in a bowl
2) Heat the coconut oil in a skillet on a medium-high heat, and when hot, add the chickpeas, stirring for 3 minutes
3) Add the remaining ingredients in the order we gave (except the vegetable stock, which goes in last), stirring for 5 more minutes, or until the sauce thickens
4) Serve with the carb of your choice; we recommend our Tasty Versatile Rice Recipe
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat More (Of This) For Lower Blood Pressure
- Honey vs Maple Syrup – Which is Healthier?
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Share This Post
-
Water Water Everywhere, But Which Is Best To Drink?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Well Well Well…
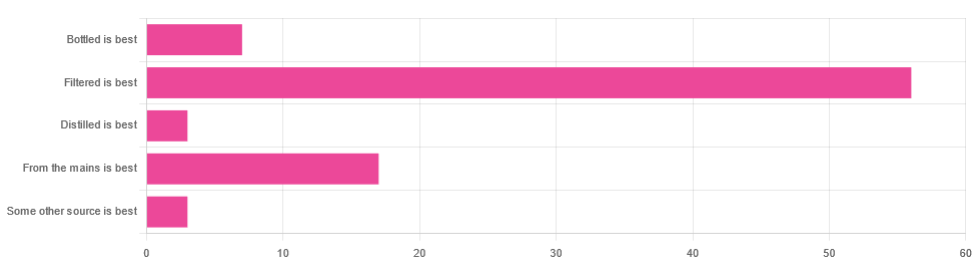
In Tuesday’s newsletter, we asked you for your (health-related) opinion on drinking water—with the understanding that this may vary from place to place. We got the above-depicted, below-described, set of responses:
- About 65% said “Filtered is best”
- About 20% said “From the mains is best”
- About 8% said “Bottled is best”
- About 3% said “Distilled is best”
- About 3% said “Some other source is best”
Of those who said “some other source is best”, one clarified that their preferred source was well water.
So what does the science say?
Fluoridated water is bad for you: True or False?
False, assuming a normal level of consumption. Rather than take up more space today though, we’ll link to what we previously wrote on this topic:
You may be wondering: but what if my level of consumption is higher than normal?
Let’s quickly look at some stats:
- The maximum permitted safety level varies from place to place, but is (for example) 2mg/l in the US, 1.5mg/l in Canada & the UK.
- The minimum recommended amount also varies from place to place, but is (for example) 0.7mg/l in Canada and the US, and 1mg/l in the UK.
It doesn’t take grabbing a calculator to realize that if you drink twice as much water as someone else, then depending on where you are, water fluoridated to the minimum may give you more than the recommended maximum.
However… Those safety margins are set so much lower than the actual toxicity levels of fluoride, that it doesn’t make a difference.
For example: your writer here takes a medication that has the side effect of causing dryness of the mouth, and consequently she drinks at least 3l of water per day in a climate that could not be described as hot (except perhaps for about 2 weeks of the year). She weighs 72kg (that’s about 158 pounds), and the toxicity of fluoride (for ill symptoms, not death) is 0.2mg/kg. So, she’d need 14.4mg of fluoride, which even if the water fluoridation here were 2mg/l (it’s not; it’s lower here, but let’s go with the highest figure to make a point), would require drinking more than 7l of water faster than the body can process it.
For more about the numbers, check out:
Acute Fluoride Poisoning from a Public Water System
Bottled water is the best: True or False?
False, if we consider “best” to be “healthiest”, which in turn we consider to be “most nutrients, with highest safety”.
Bottled water generally does have higher levels of minerals than most local mains supply water does. That’s good!
But you know what else is generally has? Microplastics and nanoplastics. That’s bad!
We don’t like to be alarmist in tone; it’s not what we’re about here, but the stats on bottled water are simply not good; see:
We Are Such Stuff As Bottles Are Made Of
You may be wondering: “but what about bottled water that comes in glass bottles?”
Indeed, water that comes in glass bottles can be expected to have lower levels of plastic than water that comes in plastic bottles, for obvious reasons.
However, we invite you to consider how likely you believe it to be that the water wasn’t stored in plastic while being processed, shipped and stored, before being portioned into its final store-ready glass bottles for end-consumer use.
Distilled water is the best: True or False?
False, generally, with caveats:
Distilled water is surely the safest water anywhere, because you know that you’ve removed any nasties.
However, it’s also devoid of nutrients, because you also removed any minerals it contained. Indeed, if you use a still, you’ll be accustomed to the build-up of these minerals (generally simplified and referenced as “limescale”, but it’s a whole collection of minerals).
Furthermore, that loss of nutrients can be more than just a “something good is missing”, because having removed certain ions, that water could now potentially strip minerals from your teeth. In practice, however, you’d probably have to swill it excessively to cause this damage.
Nevertheless, if you have the misfortune of living somewhere like Flint, Michigan, then a water still may be a fair necessity of life. In other places, it can simply be useful to have in case of emergency, of course.
Here’s an example product on Amazon if you’d like to invest in a water still for such cases.
PS: distilled water is also tasteless, and is generally considered bad, tastewise, for making tea and coffee. So we really don’t recommend distilling your water unless you have a good reason to do so.
Filtered water is the best: True or False?
True for most people in most places.
Let’s put it this way: it can’t logically be worse than whatever source of water you put into it…
Provided you change the filter regularly, of course.
Otherwise, after overusing a filter, at best it won’t be working, and at worst it’ll be adding in bacteria that have multiplied in the filter over however long you left it there.
You may be wondering: can water filters remove microplastics, and can they remove minerals?
The answer in both cases is: sometimes.
- For microplastics it depends on the filter size and the microplastic size (see our previous article for details on that).
- For minerals, it depends on the filter type. Check out:
The H2O Chronicles | 5 Water Filters That Remove Minerals
One other thing to think about: while most water filtration jugs are made of PFAS-free BPA-free plastics for obvious reasons, for greater peace of mind, you might consider investing in a glass filtration jug, like this one ← this is just one example product on Amazon; by all means shop around and find one you like
Take care!
Share This Post
Related Posts
-
Soap vs Sanitizer – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing soap to sanitizer, we picked the soap.
Why?
Both are good at killing bacteria / inactivating viruses, but there are several things that set them apart:
- Soap doesn’t just kill them; it slides them off and away down the drain. That means that any it failed to kill are also off and down the drain, not still on your hands. This is assuming good handwashing technique, of course!
- Sanitizer gel kills them, but can take up to 4 minutes of contact to do so. Given that people find 20 seconds of handwashing laborious, 240 seconds of sanitizer gel use seems too much to hope for.
Both can be dehydrating for the hands; both can have ingredients added to try to mitigate that.
We recommend a good (separate) moisturizer in either case, but the point is, the dehydration factor doesn’t swing it far either way.
So, we’ll go with the one that gets rid of the germs the most quickly: the soap
10almonds tip: splash out on the extra-nice hand-soaps for your home—this will make you and others more likely to wash your hands more often! Sometimes, making something a more pleasant experience makes all the difference.
Want to know more?
Check out:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Acorns vs Chestnuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing acorns to chestnuts, we picked the acorns.
Why?
In terms of macros, chestnuts are mostly water, so it’s not surprising that acorns have a lot more carbs, fat, protein, and fiber. Thus, unless you have personal reasons for any of those to be a problem, acorns are the better choice, offering a lot more nutritional value.
In the category of vitamins, acorns lead with a lot more of vitamins A, B2, B3, B5, B6, and B9, while chestnuts have more of vitamins B1 and C. However, that vitamin C is useless to us, because it is destroyed in the cooking process (by boiling or roasting), and both of these nuts can be harmful if consumed raw, so that cooking does need to be done. That leaves acorns with a 6:1 lead.
When it comes to minerals, things are more even; acorns have more copper, magnesium, manganese, and zinc, while chestnuts have more calcium, iron, phosphorus, and potassium. Thus, a 4:4 tie (and yes, the margins of difference are approximately equal too).
We mentioned “both of these nuts can be harmful if consumed raw”, so a note on that: it’s because, while both contain an assortment of beneficial phytochemicals, they also both contain tannins that, if consumed raw, chelate with iron, essentially taking it out of our diet and potentially creating an iron deficiency. Cooking tannins stops this from being an issue, and the same cooking process renders the tannins actively beneficial to the health, for their antioxidant powers.
You may have heard that acorns are poisonous; that’s not strictly speaking true, except insofar as anything could be deemed poisonous in excess (including such things as water, and oxygen). Rather, it’s simply the above-described matter of the uncooked tannins and iron chelation. Even then, you’re unlikely to suffer ill effects unless you consume them raw in a fair quantity. While acorns have fallen from popular favor sufficient that one doesn’t see them in supermarkets, the fact is they’ve been enjoyed as an important traditional part of the diet by various indigenous peoples of N. America for centuries*, and provided they are cooked first, they are a good healthy food for most people.
*(going so far as to cultivate natural oak savannah areas, by burning out young oaks to leave the old ones to flourish without competition, to maximize acorn production, and then store dried acorns in bulk sufficient to cover the next year or so in case of a bad harvest later—so these was not just an incidental food, but very important “our life may depend on this” food. Much like grain in many places—and yes, acorns can be ground into flour and used to make bread etc too)
Do note: they are both still tree nuts though, so if you have a tree nut allergy, these ones aren’t for you.
Otherwise, enjoy both; just cook them first!
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Mushrooms vs Eggplant – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mushrooms to eggplant, we picked the mushrooms.
Why?
First, you may be wondering: which mushrooms? Button mushrooms? White mushrooms? Chestnut mushrooms? Portobello mushrooms? And the answer is yes. Those (and more; it represents most mushrooms that are commonly sold fresh in western supermarkets) are all the same species at different ages; namely, Agaricus bisporus—not to be mistaken for fly agaric, which despite the name, is not even a member of the Agaricus genus, and is in fact Amanita muscari. This is an important distinction, because fly agaric is poisonous, though fatality is rare, and it’s commonly enjoyed recreationally (after some preparation, which reduces its toxicity) for its psychoactive effects. It’s the famous red one with white spots. Anyway, today we will be talking instead about Agaricus bisporus, which is most popular western varieties of “edible mushroom”.
With that in mind, let’s get down to it:
In terms of macros, mushrooms contain more than 3x the protein, while eggplant contains nearly 2x the carbs and 3x the fiber. We’ll call this a tie for macros.
As for vitamins, mushrooms contain more of vitamins B1, B2, B3, B5, B6, B7, B9, B12, D, and choline, while eggplant contains more of vitamins A, E, and K. Most notably for vegans, mushrooms are a good non-animal source of vitamins B12 and D, which nutrients are not generally found in plants. Mushrooms, of course, are not technically plants. In any case, the vitamins category is an easy win for mushrooms.
When it comes to minerals, mushrooms have more copper, iron, phosphorus, potassium, selenium, and zinc, while eggplant has more calcium, magnesium, and manganese. Another easy win for mushrooms.
One final thing worth noting is that mushrooms are a rich source of the amino acid ergothioneine, which has been called a “longevity vitamin” for its healthspan-increasing effects (see our article below).
Meanwhile, in the category of mushrooms vs eggplant, mushrooms don’t leave much room for doubt and are the clear winner here.
Want to learn more?
You might like to read:
The Magic of Mushrooms: “The Longevity Vitamin” (That’s Not A Vitamin)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: