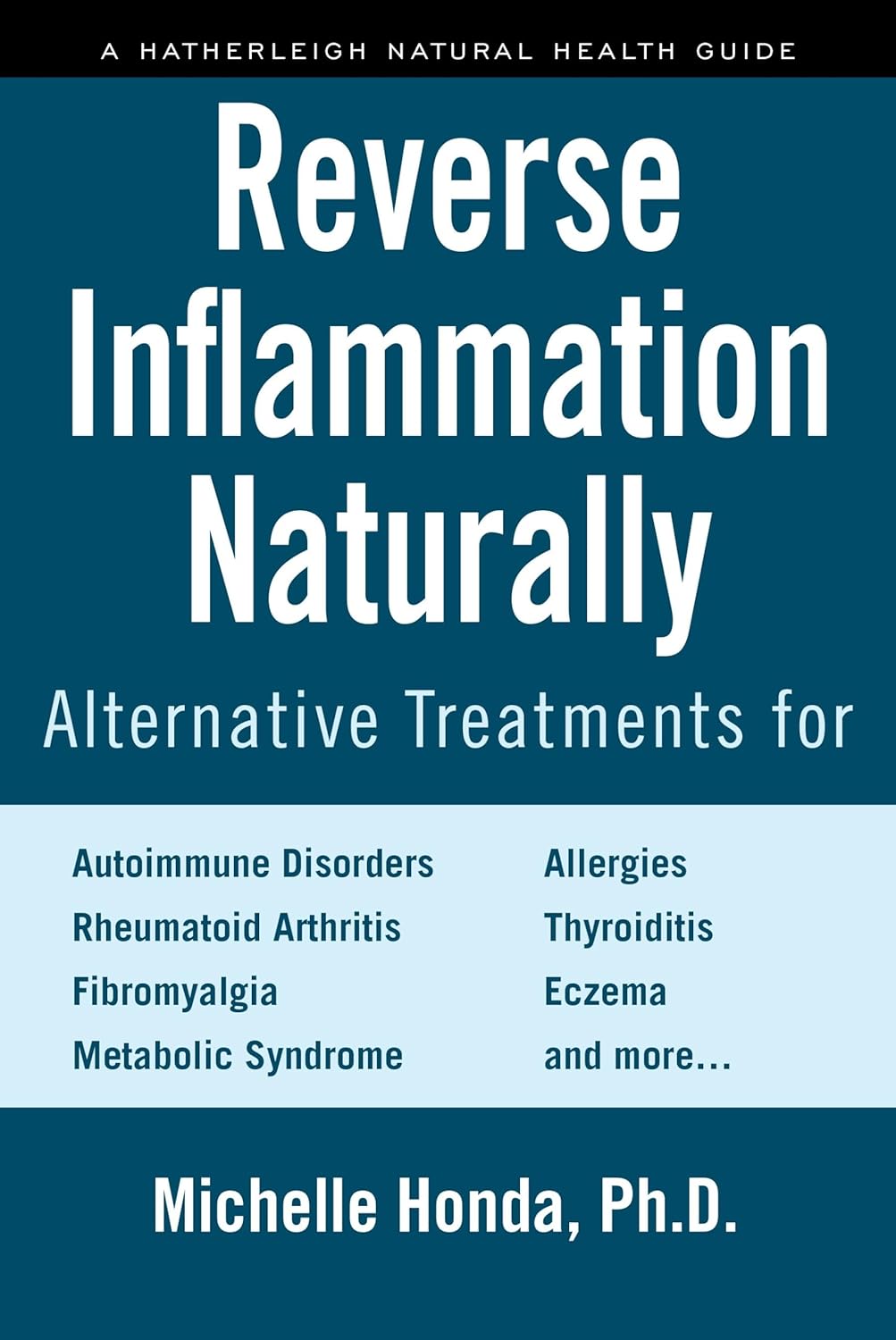
Reverse Inflammation Naturally – by Dr. Michelle Honda
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is in some ways not as marketable as some; it doesn’t have lots of colorful healthy food on the cover; it doesn’t even have a “woman laughing alone with salad” (you know the stock photo trope), let alone someone looking glamorous in a labcoat with a stethoscope draped over their shoulder despite listening to hearts not being a regular part of their job as an immunologist or such.
What it does have, instead, is a lot of very useful information, and much more than you’ll usually find in a book for laypeople.
For example, you probably know that for fighting inflammation, a green salad is better than a cheeseburger, say, and a black coffee is better than a glass of wine.
But do you know about the roles, for good or ill, of prostaglandins and linoleic fats vs dietary fats? How about delta-6-desaturase? Neu5Gc and arachidonic acid?
Dr. Honda demystifies all of these and more, as well as talking about the impacts of very many foods and related habits on various different inflammation-based disease. And of course, almost all disease involves some kind of inflammation (making fighting inflammation one of the best things you can do for your overall disease-avoidance strategy!), but she singles out some of the most relevant, as per the list on the front cover.
She also talks a lot of “pharmacy in your kitchen”, in other words, what herbs, spices, and plant extracts we can enjoy for (evidence-based!) benefits on top of our default healthy diet free (or at least mostly free, for surely none of us are perfect) from inflammatory agents.
Not content with merely giving a huge amount of information, she also gives recipes and a meal plan, but honestly, it’s the informational chapters that are the real value of the book.
Bottom line: if you’d like to reduce your body’s inflammation levels (and/or perhaps those of a loved one for whom you cook), then this book will be an invaluable resource.
Click here to check out Reverse Inflammation Naturally, and reverse inflammation naturally!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is TikTok right? Are there health benefits to eating sea moss?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sea moss is the latest “superfood” wellness influencers are swearing by. They claim sea moss products – usually in gel form – have multiple health benefits. These include supporting brain and immune function, or protecting against viruses and other microbes.
But do these health claims stack up? Let’s take a look.
Plataresca/Shutterstock What is sea moss?
Sea moss is produced using a kind of seaweed – particularly red algae – that grow in various locations all around the world. Three main species are used in sea moss products:
- Chondrus crispus (known as Irish moss or carrageenan moss)
- Eucheuma cottonii (sea moss or seabird’s nest)
- Gracilaria (Irish moss or ogonori).
Some products also contain the brown algae Fucus vesiculosus (commonly known as bladderwrack, black tang, rockweed, sea grapes, bladder fucus, sea oak, cut weed, dyers fucus, red fucus or rock wrack).
Most sea moss products are sold as a gel that can be added to recipes, used in smoothies, frozen into ice cubes or eaten on its own. The products also come in capsule form or can be purchased “raw” and used to make your own gels at home.
Several kinds of red algae are used in commercially-available sea moss products. Nancy Ann Bowe/Shutterstock What’s the evidence?
Sea moss products claim a host of potential health benefits, from supporting immunity, to promoting skin health and enhancing mood and focus, among many others.
But is there any evidence supporting these claims?
Recent studies have reviewed the biological properties of the main sea moss species (Chondrus crispus, Eucheuma cottonii, Gracilaria and Fucus vesiculosus).
They suggest these species may have anti-inflammatory, antioxidant, anticancer, antidiabetic and probiotic properties.
However, the vast majority of research relating to Chondrus crispus, Gracilaria and Fucus vesiculosus – and all of the research on Eucheuma cottonii – comes from studies done in test tubes or using cell and animal models. We should not assume the health effects seen would be the same in humans.
In cell and animal studies, researchers usually administer algae in a laboratory and use specific extracts rich in bioactive compounds rather than commercially available sea moss products.
They also use very different – often relatively larger – amounts compared to what someone would typically consume when they eat sea moss products.
This means the existing studies can’t tell us about the human body’s processes when eating and digesting sea moss.
Sea moss may have similar effects in humans. But so far there is very little evidence people who consume sea moss will experience any of the claimed health benefits.
Nutritional value
Eating sea moss does not replace the need for a balanced diet, including a variety of fruits and vegetables.
Chondrus crispus, Eucheuma cottonii and Gracilaria, like many seaweeds, are rich sources of nutrients such as fatty acids, amino acids, vitamin C and minerals. These nutrients are also likely to be present in sea moss, although some may be lost during the preparation of the product (for example, soaking may reduce vitamin C content), and those that remain could be present in relatively low quantities.
There are claims that sea moss may be harmful for people with thyroid problems. This relates to the relationship between thyroid function and iodine. The algae used to make sea moss are notable sources of iodine and excess iodine intake can contribute to thyroid problems, particularly for people with pre-existing conditions. That is why these products often carry disclaimers related to iodine sensitivity or thyroid health.
Is it worth it?
So you may be wondering if it’s worth trying sea moss. Here are a few things to consider before you decide whether to start scooping sea moss into your smoothies.
A 375mL jar costs around $A25–$30 and lasts about seven to ten days, if you follow the recommended serving suggestion of two tablespoons per day. This makes it a relatively expensive source of nutrients.
Sea moss is commonly sold as a gel that can be eaten on a kitchen bench. April Sims/Shutterstock Sea moss is often hyped for containing 92 different minerals. While there may be 92 minerals present, the amount of minerals in the algae will vary depending on growing location and conditions.
The efficiency with which minerals from algae can be absorbed and used by the body also varies for different minerals. For example, sodium is absorbed well, while only about 50% of iodine is absorbed.
But sea moss has also been shown to contain lead, mercury and other heavy metals – as well as radioactive elements (such as radon) that can be harmful to humans. Seaweeds are known for their ability to accumulate minerals from their environment, regardless of whether these are beneficial or harmful for human nutrition. Remember, more doesn’t always mean better.
What else am I eating?
While you won’t get a full nutritional breakdown on the jar, it is always wise to check what other ingredients you may be eating. Sea moss products can contain a range of other ingredients, such as lime, monk fruit powder, spirulina and ginger, among many others.
These ingredients differ between brands and products, so be aware of your needs and always check.
Despite their health claims, most sea moss products also carry disclaimers indicating that the products are not intended to diagnose, treat, cure or prevent any disease.
If you have concerns about your health, always speak to a health professional for accurate and personalised medical advice.
Margaret Murray, Senior Lecturer, Nutrition, Swinburne University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Children with traumatic experiences have a higher risk of obesity – but this can be turned around
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Children with traumatic experiences in their early lives have a higher risk of obesity. But as our new research shows, this risk can be reduced through positive experiences.
Childhood traumatic experiences are alarmingly common. Our analysis of data from nearly 5,000 children in the Growing Up in New Zealand study revealed almost nine out of ten (87%) faced at least one significant source of trauma by the time they were eight years old. Multiple adverse experiences were also prevalent, with one in three children (32%) experiencing at least three traumatic events.
Childhood trauma includes a range of experiences such as physical and emotional abuse, peer bullying and exposure to domestic violence. It also includes parental substance abuse, mental illness, incarceration, separation or divorce and ethnic discrimination.
We found children from financially disadvantaged households and Māori and Pasifika had the highest prevalence of nearly all types of adverse experiences, as well as higher overall numbers of adversities.
The consequences of these experiences were far-reaching. Children who experienced at least one adverse event were twice as likely to be obese by age eight. The risk increased with the number of traumatic experiences. Children with four or more adverse experiences were nearly three times more likely to be obese.
Notably, certain traumatic experiences (including physical abuse and parental domestic violence) related more strongly to obesity than others. This highlights the strong connection between early-life adversity and physical health outcomes.
PickPik, CC BY-SA Connecting trauma to obesity
One potential explanation could be that the accumulation of early stress in children’s family, school and social environments is associated with greater psychological distress. This in turn makes children more likely to adopt unhealthy weight-related behaviours.
This includes consuming excessive high-calorie “comfort” foods such as fast food and sugary drinks, inadequate intake of nutritious foods, poor sleep, excessive screen time and physical inactivity. In our research, children who experienced adverse events were more likely to adopt these unhealthy behaviours. These, in turn, were associated with a higher risk of obesity.
Despite these challenges, our research also explored a promising area: the protective and mitigating effects of positive experiences.
We defined positive experiences as:
- parents in a committed relationship
- mothers interacting well with their children
- mothers involved in social groups
- children engaged in enriching experiences and activities such as visiting libraries or museums and participating in sports and community events
- children living in households with routines and rules, including those regulating bedtime, screen time and mealtimes
- children attending effective early childhood education.
The findings were encouraging. Children with more positive experiences were significantly less likely to be obese by age eight.
For example, those with five or six positive experiences were 60% less likely to be overweight or obese compared to children with zero or one positive experience. Even two positive experiences reduced the likelihood by 25%.
Positive childhood experiences such as playing sports or visiting libraries can lower the risk of obesity. Getty Images How positive experiences counteract trauma
Positive experiences can help mitigate the negative effects of childhood trauma. But a minimum of four positive experiences was required to significantly counteract the impact of adverse events.
While nearly half (48%) of the study participants had at least four positive experiences, a concerning proportion (more than one in ten children) reported zero or only one positive experience.
The implications are clear. Traditional weight-loss programmes focused solely on changing behaviours are not enough to tackle childhood obesity. To create lasting change, we must also address the social environments, life experiences and emotional scars of early trauma shaping children’s lives.
Fostering positive experiences is a vital part of this holistic approach. These experiences not only help protect children from the harmful effects of adversity but also promote their overall physical and mental wellbeing. This isn’t just about preventing obesity – it’s about giving children the foundation to thrive and reach their full potential.
Creating supportive environments for vulnerable children
Policymakers, schools and families all have a role to play. Community-based programmes, such as after-school activities, healthy relationship initiatives and mental health services should be prioritised to support vulnerable families.
Trauma-informed care is crucial, particularly for children from disadvantaged households who face higher levels of adversity and fewer positive experiences. Trauma-informed approaches are especially crucial for addressing the effects of domestic violence and other adverse childhood experiences.
Comprehensive strategies should prioritise both safety and emotional healing by equipping families with tools to create safe, nurturing environments and providing access to mental health services and community support initiatives.
At the family level, parents can establish stable routines, participate in social networks and engage children in enriching activities. Schools and early-childhood education providers also play a key role in fostering supportive environments that help children build resilience and recover from trauma.
Policymakers should invest in resources that promote positive experiences across communities, addressing inequalities that leave some children more vulnerable than others. By creating nurturing environments, we can counterbalance the impacts of trauma and help children lead healthier, more fulfilling lives.
When positive experiences outweigh negative ones, children have a far greater chance of thriving – physically, emotionally and socially.
Ladan Hashemi, Senior Research Fellow in Health Sciences, University of Auckland, Waipapa Taumata Rau
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
How to Stop Negative Thinking – by Daniel Paul
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Just think positive thoughts” is all well and good, but it doesn’t get much mileage in the real world, does it?
What Daniel Paul offers is a lot better than that. Taking a CBT approach, he recommends tips and tricks, gives explanations and exercises, and in short, puts tools in the reader’s toolbox.
But it doesn’t stop at just stopping negative thinking. Rather, it takes a holistic approach to also improve your general life…
- Bookending your day with a good start and finish
- Scheduling a time for any negative thinking that does need to occur (again with the useful realism!)
- Inviting the reader to take on small challenges, of the kind that’ll have knock-on effects that add and multiply and compound as we go
The format is very easy-reading, and we love that there are clear section headings and chapter summaries, too.
Bottom line: definitely a book with the potential to improve your life from day one, and that’ll keep you coming back to it as a cheatsheet and references source.
Get your copy of “How to Stop Negative Thinking” from Amazon today!
Share This Post
Related Posts
-
When Bad Joints Stop You From Exercising (5 Things To Change)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The first trick to exercising with bad joints is to have better joints.
Now, this doesn’t necessarily mean you can take a supplement and magically your joint problems will be cured, but there are adjustable lifestyle factors that can and will make things relatively better or worse.
We say “and will”, because you don’t get a choice in that part. Everything we do, every little choice in our day, makes our health a little better or a little worse in some aspect(s). But we do get a choice between “relatively better” and “relatively worse”.
With that in mind, do check out:
- Avoiding/Managing Osteoarthritis
- Avoiding/Managing Rheumatoid Arthritis
- How To Really Look After Your Joints
Ok, you have bad joints though; what next?
Let’s assume you’re doing your best with the above, and/or have simply decided not to, which is your call. You know your circumstances best. Either way, your joints are still not in sufficiently good condition to be able to exercise the way you’d like.
First, the obvious: enjoy low-impact exercises
For example:
- Swimming
- Yoga (much more appropriate here than the commonly-paired “and tai chi”)*
- Isometric exercises (i.e. exercise without movement, e.g. squeezing things, or stationary stability exercises)
*This is not to say that tai chi is bad. But if your problem is specifically your knees, there are many movements in most forms of tai chi that require putting the majority of one’s weight on one bent leg, which means the knee of that leg is going to suffer. If your knees are fine, then this won’t be an issue and it will simply continue strengthening your knees without discomfort. But they have to be fine first.
See also: Exercising With Osteoporosis
Second: support your joints through a full range of motion
If you have bad joints, you probably know that there’s an unfortunate paradox whereby you get to choose between:
- Exercise, and inflame your joints
- Rest, and your joints seize up
This is the way to get around that damaging dilemma.
Moving your joints through a full range of motion regularly is critical for their maintenance, so do that in a way that isn’t straining them:
If it’s your shoulders, for example, you can do (slow, gentle!) backstroke or front-crawl or butterfly motions while standing in the comfort of your living room.
If it’s your knees, then supported squats can do you a world of good. That means, squat in front of a table or other stable object, with your fingertips (or as much of your hands as you need) on it, to take a portion of your weight (it can be a large portion; that’s fine too!) while you go through the full range of motion of the squat. Repeat.
And so forth for other joints.
See also: The Most Underrated Hip Mobility Exercise (Not Stretching)
Third: work up slowly, and stop early
You can do exercises that involve impact, and if you live a fairly normal life, you’ll probably have to (walking is an impact exercise). You can also enjoy cycling (low-impact, but not so low-impact as we discussed in the last section) and work up to running if you want to.
However…
While building up your joints’ mobility and strength, it is generally a good idea to stop before you think you need to.
This means that it’s important to do those exercises in a way that you can stop early. For example, an exercise bike or a treadmill can be a lot of use here, so that you don’t find you need to stop for the day while miles from your house.
If you get such a device, it doesn’t even have to be fancy and/or expensive. This writer got herself an inexpensive exercise bike like this one, and it’s perfectly adequate.
Fourth: prioritize recovery, even if it doesn’t feel like you need it
Everyone should do this anyway, but if your joints are bad, it goes double:
Overdone It? How To Speed Up Recovery After Exercise (According To Actual Science)
Fifth: get professional help
Physiotherapists are great for this. Find one, and take their advice for your specific body and your specific circumstances and goals.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Semaglutide for Weight Loss?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Semaglutide for weight loss?
Semaglutide is the new kid on the weight-loss block, but it’s looking promising (with some caveats!).
Most popularly by brand names Ozempic and Wegovy, it was first trialled to help diabetics*, and is now sought-after by the rest of the population too. So far, only Wegovy is FDA-approved for weight loss. It contains more semaglutide than Ozempic, and was developed specifically for weight loss, rather than for diabetes.
*Specifically: diabetics with type 2 diabetes. Because it works by helping the pancreas to make insulin, it’s of no help whatsoever to T1D folks, sadly. If you’re T1D and reading this though, today’s book of the day is for you!
First things first: does it work as marketed for diabetes?
It does! At a cost: a very common side effect is gastrointestinal problems—same as for tirzepatide, which (like semaglutide) is a GLP-1 agonist, meaning it works the same way. Here’s how they measure up:
- Head-to-head study: Effects of subcutaneous tirzepatide versus placebo or semaglutide on pancreatic islet function and insulin sensitivity in adults with type 2 diabetes
- Head-to-head systematic review: Semaglutide for the treatment of type 2 Diabetes Mellitus: A systematic review and network meta-analysis of safety and efficacy outcomes
As you can see, both of them work wonders for pancreatic function and insulin sensitivity!
And, both of them were quite unpleasant for around 20% of participants:
❝Tirzepatide, oral and SC semaglutide has a favourable efficacy in treating T2DM. Gastrointestinal adverse events were highly recorded in tirzepatide, oral and SC semaglutide groups.❞
What about for weight loss, if not diabetic?
It works just the same! With just the same likelihood of gastro-intestinal unpleasantries, though. There’s a very good study that was done with 1,961 overweight adults; here it is:
Once-Weekly Semaglutide in Adults with Overweight or Obesity
The most interesting things here are the positive results and the side effects:
❝The mean change in body weight from baseline to week 68 was −14.9% in the semaglutide group as compared with −2.4% with placebo, for an estimated treatment difference of −12.4 percentage points (95% confidence interval [CI], −13.4 to −11.5; P<0.001).❞
In other words: if you take this, you’re almost certainly going to get something like 6x better weight loss results than doing the same thing without it.
❝Nausea and diarrhea were the most common adverse events with semaglutide; they were typically transient and mild-to-moderate in severity and subsided with time. More participants in the semaglutide group than in the placebo group discontinued treatment owing to gastrointestinal events (59 [4.5%] vs. 5 [0.8%])❞
~ ibid.
In other words: you have about a 3% chance of having unpleasant enough side effects that you don’t want to continue treatment (contrast this with the 20%ish chance of unpleasant side effects of any extent)!
Any other downsides we should know about?
If you stop taking it, weight regain is likely. For example, a participant in one of the above-mentioned studies who lost 22% of her body weight with the drug’s help, says:
❝Now that I am no longer taking the drug, unfortunately, my weight is returning to what it used to be. It felt effortless losing weight while on the trial, but now it has gone back to feeling like a constant battle with food. I hope that, if the drug can be approved for people like me, my [doctor] will be able to prescribe the drug for me in the future.❞
~ Jan, a trial participant at UCLH
Is it injection-only, or is there an oral option?
An oral option exists, but (so far) is on the market only in the form of Rybelsus, another (slightly older) drug containing semaglutide, and it’s (so far) only FDA-approved for diabetes, not for weight loss. See:
A new era for oral peptides: SNAC and the development of oral semaglutide for the treatment of type 2 diabetes ← for the science
FDA approves first oral GLP-1 treatment for type 2 diabetes ← For the FDA statement
Where can I get these?
Availability and prescribing regulations vary by country (because the FDA’s authority stops at the US borders), but here is the website for each of them if you’d like to learn more / consider if they might help you:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
If You’re Poor, Fertility Treatment Can Be Out of Reach
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mary Delgado’s first pregnancy went according to plan, but when she tried to get pregnant again seven years later, nothing happened. After 10 months, Delgado, now 34, and her partner, Joaquin Rodriguez, went to see an OB-GYN. Tests showed she had endometriosis, which was interfering with conception. Delgado’s only option, the doctor said, was in vitro fertilization.
“When she told me that, she broke me inside,” Delgado said, “because I knew it was so expensive.”
Delgado, who lives in New York City, is enrolled in Medicaid, the federal-state health program for low-income and disabled people. The roughly $20,000 price tag for a round of IVF would be a financial stretch for lots of people, but for someone on Medicaid — for which the maximum annual income for a two-person household in New York is just over $26,000 — the treatment can be unattainable.
Expansions of work-based insurance plans to cover fertility treatments, including free egg freezing and unlimited IVF cycles, are often touted by large companies as a boon for their employees. But people with lower incomes, often minorities, are more likely to be covered by Medicaid or skimpier commercial plans with no such coverage. That raises the question of whether medical assistance to create a family is only for the well-to-do or people with generous benefit packages.
“In American health care, they don’t want the poor people to reproduce,” Delgado said. She was caring full-time for their son, who was born with a rare genetic disorder that required several surgeries before he was 5. Her partner, who works for a company that maintains the city’s yellow cabs, has an individual plan through the state insurance marketplace, but it does not include fertility coverage.
Some medical experts whose patients have faced these issues say they can understand why people in Delgado’s situation think the system is stacked against them.
“It feels a little like that,” said Elizabeth Ginsburg, a professor of obstetrics and gynecology at Harvard Medical School who is president-elect of the American Society for Reproductive Medicine, a research and advocacy group.
Whether or not it’s intended, many say the inequity reflects poorly on the U.S.
“This is really sort of standing out as a sore thumb in a nation that would like to claim that it cares for the less fortunate and it seeks to do anything it can for them,” said Eli Adashi, a professor of medical science at Brown University and former president of the Society for Reproductive Endocrinologists.
Yet efforts to add coverage for fertility care to Medicaid face a lot of pushback, Ginsburg said.
Over the years, Barbara Collura, president and CEO of the advocacy group Resolve: The National Infertility Association, has heard many explanations for why it doesn’t make sense to cover fertility treatment for Medicaid recipients. Legislators have asked, “If they can’t pay for fertility treatment, do they have any idea how much it costs to raise a child?” she said.
“So right there, as a country we’re making judgments about who gets to have children,” Collura said.
The legacy of the eugenics movement of the early 20th century, when states passed laws that permitted poor, nonwhite, and disabled people to be sterilized against their will, lingers as well.
“As a reproductive justice person, I believe it’s a human right to have a child, and it’s a larger ethical issue to provide support,” said Regina Davis Moss, president and CEO of In Our Own Voice: National Black Women’s Reproductive Justice Agenda, an advocacy group.
But such coverage decisions — especially when the health care safety net is involved — sometimes require difficult choices, because resources are limited.
Even if state Medicaid programs wanted to cover fertility treatment, for instance, they would have to weigh the benefit against investing in other types of care, including maternity care, said Kate McEvoy, executive director of the National Association of Medicaid Directors. “There is a recognition about the primacy and urgency of maternity care,” she said.
Medicaid pays for about 40% of births in the United States. And since 2022, 46 states and the District of Columbia have elected to extend Medicaid postpartum coverage to 12 months, up from 60 days.
Fertility problems are relatively common, affecting roughly 10% of women and men of childbearing age, according to the National Institute of Child Health and Human Development.
Traditionally, a couple is considered infertile if they’ve been trying to get pregnant unsuccessfully for 12 months. Last year, the ASRM broadened the definition of infertility to incorporate would-be parents beyond heterosexual couples, including people who can’t get pregnant for medical, sexual, or other reasons, as well as those who need medical interventions such as donor eggs or sperm to get pregnant.
The World Health Organization defined infertility as a disease of the reproductive system characterized by failing to get pregnant after a year of unprotected intercourse. It terms the high cost of fertility treatment a major equity issue and has called for better policies and public financing to improve access.
No matter how the condition is defined, private health plans often decline to cover fertility treatments because they don’t consider them “medically necessary.” Twenty states and Washington, D.C., have laws requiring health plans to provide some fertility coverage, but those laws vary greatly and apply only to companies whose plans are regulated by the state.
In recent years, many companies have begun offering fertility treatment in a bid to recruit and retain top-notch talent. In 2023, 45% of companies with 500 or more workers covered IVF and/or drug therapy, according to the benefits consultant Mercer.
But that doesn’t help people on Medicaid. Only two states’ Medicaid programs provide any fertility treatment: New York covers some oral ovulation-enhancing medications, and Illinois covers costs for fertility preservation, to freeze the eggs or sperm of people who need medical treatment that will likely make them infertile, such as for cancer. Several other states also are considering adding fertility preservation services.
In Delgado’s case, Medicaid covered the tests to diagnose her endometriosis, but nothing more. She was searching the internet for fertility treatment options when she came upon a clinic group called CNY Fertility that seemed significantly less expensive than other clinics, and also offered in-house financing. Based in Syracuse, New York, the company has a handful of clinics in upstate New York cities and four other U.S. locations.
Though Delgado and her partner had to travel more than 300 miles round trip to Albany for the procedures, the savings made it worthwhile. They were able do an entire IVF cycle, including medications, egg retrieval, genetic testing, and transferring the egg to her uterus, for $14,000. To pay for it, they took $7,000 of the cash they’d been saving to buy a home and financed the other half through the fertility clinic.
She got pregnant on the first try, and their daughter, Emiliana, is now almost a year old.
Delgado doesn’t resent people with more resources or better insurance coverage, but she wishes the system were more equitable.
“I have a medical problem,” she said. “It’s not like I did IVF because I wanted to choose the gender.”
One reason CNY is less expensive than other clinics is simply that the privately owned company chooses to charge less, said William Kiltz, its vice president of marketing and business development. Since the company’s beginning in 1997, it has become a large practice with a large volume of IVF cycles, which helps keep prices low.
At this point, more than half its clients come from out of state, and many earn significantly less than a typical patient at another clinic. Twenty percent earn less than $50,000, and “we treat a good number who are on Medicaid,” Kiltz said.
Now that their son, Joaquin, is settled in a good school, Delgado has started working for an agency that provides home health services. After putting in 30 hours a week for 90 days, she’ll be eligible for health insurance.
One of the benefits: fertility coverage.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: