7 Kinds Of Rest When Sleep Is Not Enough
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Taking Rest Seriously (More Than Just Sleep)
This is Dr. Matthew Edlund. He has 44 years experience as a psychiatrist, and is also a sleep specialist. He has a holistic view of health, which is reflected in his practice; he advocates for “a more complete health: physical, mental, social, and spiritual well-being”.
What does he want us to know?
Sleep, yes
Sleep cannot do all things for us in terms of rest, but it can do a lot, and it is critical. It is, in short, a necessary-but-not-sufficient condition for being well-rested.
See also: Why You Probably Need More Sleep
Rest actively
Rest is generally thought of as a passive activity, if you’ll pardon the oxymoron. Popular thinking is that it’s not something defined by what we do, so much what we stop doing.
In contrast, Dr. Edlund argues that to take rest seriously, we need do restful things.
Rest is as important as eating, and we wouldn’t want for that to “just happen”, would we?
Dr. Edlund advocates for restful activities such as going to the garden (or a nearby park) to relax. He also suggests we not underestimate the power of sex as an actively restful activity—this one is generally safer in the privacy of one’s home, though!
Rest physically
This is about actively relaxing our body—yoga is a great option here, practised in a way that is not physically taxing, but is physically rejuvenating; gentle stretches are key. Without such things, our body will keep tension, and that is not restful.
For the absolute most restful yogic practice? Check out:
Non-Sleep Deep Rest: A Neurobiologist’s Take
this is about yoga nidra!
Rest mentally
The flipside of the above is that we do need to rest our mind also. When we try to rest from a mental activity by taking on a different mental activity that uses the same faculties of the brain, it is not restful.
Writer’s example: as a writer, I could not rest from my writing by writing recreationally, or even by reading. An accountant, however, could absolutely rest from accounting by picking up a good book, should they feel so inclined.
Rest socially
While we all have our preferences when it comes to how much or how little social interaction we like in our lives, humans are fundamentally social creatures, and it is hardwired into us by evolution to function at our best in a community.
This doesn’t mean you have to go out partying every night, but it does mean you should take care to spend at least a little time with friends, even if just once or twice per week, and yes, even if it’s just a videocall (in person is best, but not everyone lives close by!)
If your social life is feeling a little thin on the ground these days, that’s a very common thing—not only as we get older, but also as many social institutions took a dive in functionality on account of the pandemic, and many are still floundering. Nevertheless, there are more options than you probably realize; yes, even for the naturally reclusive:
How To Beat Loneliness & Isolation
Rest spiritually
Be we religious or not, there are scientifically well-evidenced benefits to religious practices—some are because of the social aspect, and follow on from what we talked about just above. Other benefits come from activities such as prayer or meditation (which means that having some kind of faith, while beneficial, is not actually a requirement for spiritual rest—comparable practices without faith are fine too).
We discussed the overlapping practices of prayer and meditation, here:
The Science Of Mantra Meditation
Rest at home
Obviously, most people sleep at home. But…
Busy family homes can sometimes need a bit of conscious effort to create a restful environment, even if just for a while. A family dinner together is one great way to achieve this, and also ties in with the social element we mentioned before!
A different challenge faced by a lot of older people without live-in families, on the other hand, is the feeling of too much opportunity for rest—and then a feeling of shame for taking it. The view is commonly held that, for example, taking an afternoon nap is a sign of weakness.
On the contrary: taking an afternoon nap can be a good source of strength! Check out:
How To Nap Like A Pro (No More “Sleep Hangovers”!)
Rest at work
Our readership has a lot of retirees, but we know that’s not the case for everyone. How then, to rest while at work? Ideally we have breaks, of course, but most workplaces do not exactly have an amusement arcade in the break room. Nevertheless, there are some quick resets that can be done easily, anywhere, and (almost) any time:
Meditation Games: Meditation That You’ll Actually Enjoy
Want to know more?
You might also like:
How To Rest More Efficiently (Yes, Really)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
3 signs your diet is causing too much muscle loss – and what to do about it
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When trying to lose weight, it’s natural to want to see quick results. So when the number on the scales drops rapidly, it seems like we’re on the right track.
But as with many things related to weight loss, there’s a flip side: rapid weight loss can result in a significant loss of muscle mass, as well as fat.
So how you can tell if you’re losing too much muscle and what can you do to prevent it?
EvMedvedeva/Shutterstock Why does muscle mass matter?
Muscle is an important factor in determining our metabolic rate: how much energy we burn at rest. This is determined by how much muscle and fat we have. Muscle is more metabolically active than fat, meaning it burns more calories.
When we diet to lose weight, we create a calorie deficit, where our bodies don’t get enough energy from the food we eat to meet our energy needs. Our bodies start breaking down our fat and muscle tissue for fuel.
A decrease in calorie-burning muscle mass slows our metabolism. This quickly slows the rate at which we lose weight and impacts our ability to maintain our weight long term.
How to tell you’re losing too much muscle
Unfortunately, measuring changes in muscle mass is not easy.
The most accurate tool is an enhanced form of X-ray called a dual-energy X-ray absorptiometry (DXA) scan. The scan is primarily used in medicine and research to capture data on weight, body fat, muscle mass and bone density.
But while DEXA is becoming more readily available at weight-loss clinics and gyms, it’s not cheap.
There are also many “smart” scales available for at home use that promise to provide an accurate reading of muscle mass percentage.
Some scales promise to tell us our muscle mass. Lee Charlie/Shutterstock However, the accuracy of these scales is questionable. Researchers found the scales tested massively over- or under-estimated fat and muscle mass.
Fortunately, there are three free but scientifically backed signs you may be losing too much muscle mass when you’re dieting.
1. You’re losing much more weight than expected each week
Losing a lot of weight rapidly is one of the early signs that your diet is too extreme and you’re losing too much muscle.
Rapid weight loss (of more than 1 kilogram per week) results in greater muscle mass loss than slow weight loss.
Slow weight loss better preserves muscle mass and often has the added benefit of greater fat mass loss.
One study compared people in the obese weight category who followed either a very low-calorie diet (500 calories per day) for five weeks or a low-calorie diet (1,250 calories per day) for 12 weeks. While both groups lost similar amounts of weight, participants following the very low-calorie diet (500 calories per day) for five weeks lost significantly more muscle mass.
2. You’re feeling tired and things feel more difficult
It sounds obvious, but feeling tired, sluggish and finding it hard to complete physical activities, such as working out or doing jobs around the house, is another strong signal you’re losing muscle.
Research shows a decrease in muscle mass may negatively impact your body’s physical performance.
3. You’re feeling moody
Mood swings and feeling anxious, stressed or depressed may also be signs you’re losing muscle mass.
Research on muscle loss due to ageing suggests low levels of muscle mass can negatively impact mental health and mood. This seems to stem from the relationship between low muscle mass and proteins called neurotrophins, which help regulate mood and feelings of wellbeing.
So how you can do to maintain muscle during weight loss?
Fortunately, there are also three actions you can take to maintain muscle mass when you’re following a calorie-restricted diet to lose weight.
1. Incorporate strength training into your exercise plan
While a broad exercise program is important to support overall weight loss, strength-building exercises are a surefire way to help prevent the loss of muscle mass. A meta-analysis of studies of older people with obesity found resistance training was able to prevent almost 100% of muscle loss from calorie restriction.
Relying on diet alone to lose weight will reduce muscle along with body fat, slowing your metabolism. So it’s essential to make sure you’ve incorporated sufficient and appropriate exercise into your weight-loss plan to hold onto your muscle mass stores.
Strength-building exercises help you retain muscle. BearFotos/Shutterstock But you don’t need to hit the gym. Exercises using body weight – such as push-ups, pull-ups, planks and air squats – are just as effective as lifting weights and using strength-building equipment.
Encouragingly, moderate-volume resistance training (three sets of ten repetitions for eight exercises) can be as effective as high-volume training (five sets of ten repetitions for eight exercises) for maintaining muscle when you’re following a calorie-restricted diet.
2. Eat more protein
Foods high in protein play an essential role in building and maintaining muscle mass, but research also shows these foods help prevent muscle loss when you’re following a calorie-restricted diet.
But this doesn’t mean just eating foods with protein. Meals need to be balanced and include a source of protein, wholegrain carb and healthy fat to meet our dietary needs. For example, eggs on wholegrain toast with avocado.
3. Slow your weight loss plan down
When we change our diet to lose weight, we take our body out of its comfort zone and trigger its survival response. It then counteracts weight loss, triggering several physiological responses to defend our body weight and “survive” starvation.
Our body’s survival mechanisms want us to regain lost weight to ensure we survive the next period of famine (dieting). Research shows that more than half of the weight lost by participants is regained within two years, and more than 80% of lost weight is regained within five years.
However, a slow and steady, stepped approach to weight loss, prevents our bodies from activating defence mechanisms to defend our weight when we try to lose weight.
Ultimately, losing weight long-term comes down to making gradual changes to your lifestyle to ensure you form habits that last a lifetime.
At the Boden Group, Charles Perkins Centre, we are studying the science of obesity and running clinical trials for weight loss. You can register here to express your interest.
Nick Fuller, Charles Perkins Centre Research Program Leader, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
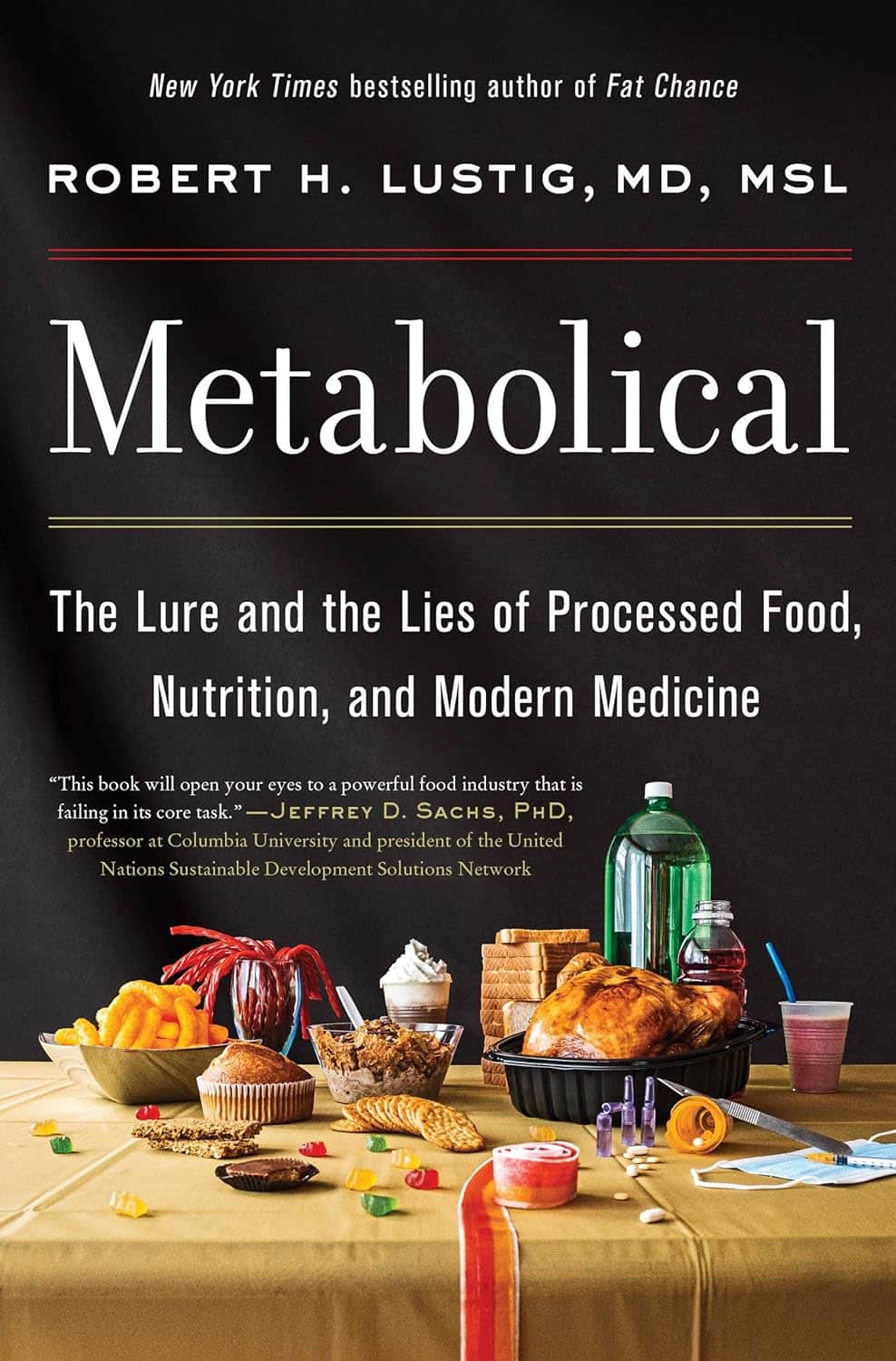
Metabolical – by Dr. Robert Lustig
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The premise of this book itself is not novel: processed food is bad, food giants lie to us, and eating better makes us less prone to disease (especially metabolic disease).
What this book does offer that’s less commonly found is a comprehensive guide, a walkthrough of each relevant what and why and how, with plenty of good science and practical real-world examples.
In terms of unique selling points, perhaps the greatest strength of this book is its focus on two things in particular that affect many aspects of health: looking after our liver, and looking after our gut.
The style is… A little dramatic perhaps, but that’s just the style; there’s no hyperbole, he is stating well-established scientific facts.
Bottom line: very much of chronic disease would be a lot less diseasey if we all ate with these aspects of our health in mind. This book’s a comprehensive guide to that.
Click here to check out Metabolical, and let food be thy medicine!
Share This Post
-
5 Ways To Make Your Smoothie Blood Sugar Friendly (Avoid the Spike!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At 10almonds, we are often saying “eat whole fruit; don’t drink your calories”. Whole fruit is great for blood sugars; fruit juices and many smoothies on the other hand, not so much. Especially juices, being near-completely or perhaps even completely stripped of fiber, but even smoothies have had a lot of the fiber broken down and are still a liquid, meaning they are very quickly and easily digestible, and thus their sugars (whatever carbs are in there) can just zip straight into your veins.
However, there are ways to mitigate this…
Slow it down
The theme here is “give the digestive process something else to do”; some things are more quickly and easily digestible than others, and if it’s working on breaking down some of the slower things, it’s not waving sugars straight on through; they have to wait their turn.
To that end, recommendations include:
- Full-fat Greek yogurt which provides both protein and fat, helping to slow down the absorption of sugar. Always choose unsweetened versions to avoid added sugars, though!
- Coconut milk (canned) which is low in sugar and carbs, high in fat. This helps reduce blood sugar spikes, as she found through personal experimentation too.
- Avocado which is rich in healthy fats that help stabilize blood sugar. As a bonus, it blends well into smoothies without affecting the taste much.
- Coconut oil which contains medium-chain triglycerides (MCTs) that are quickly absorbed for energy without involving glucose, promoting fat-burning and reducing blood sugar spikes.
- Collagen powder which is a protein that helps lower blood sugar spikes while also supporting muscle growth, skin, and joints.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
Related Posts
-
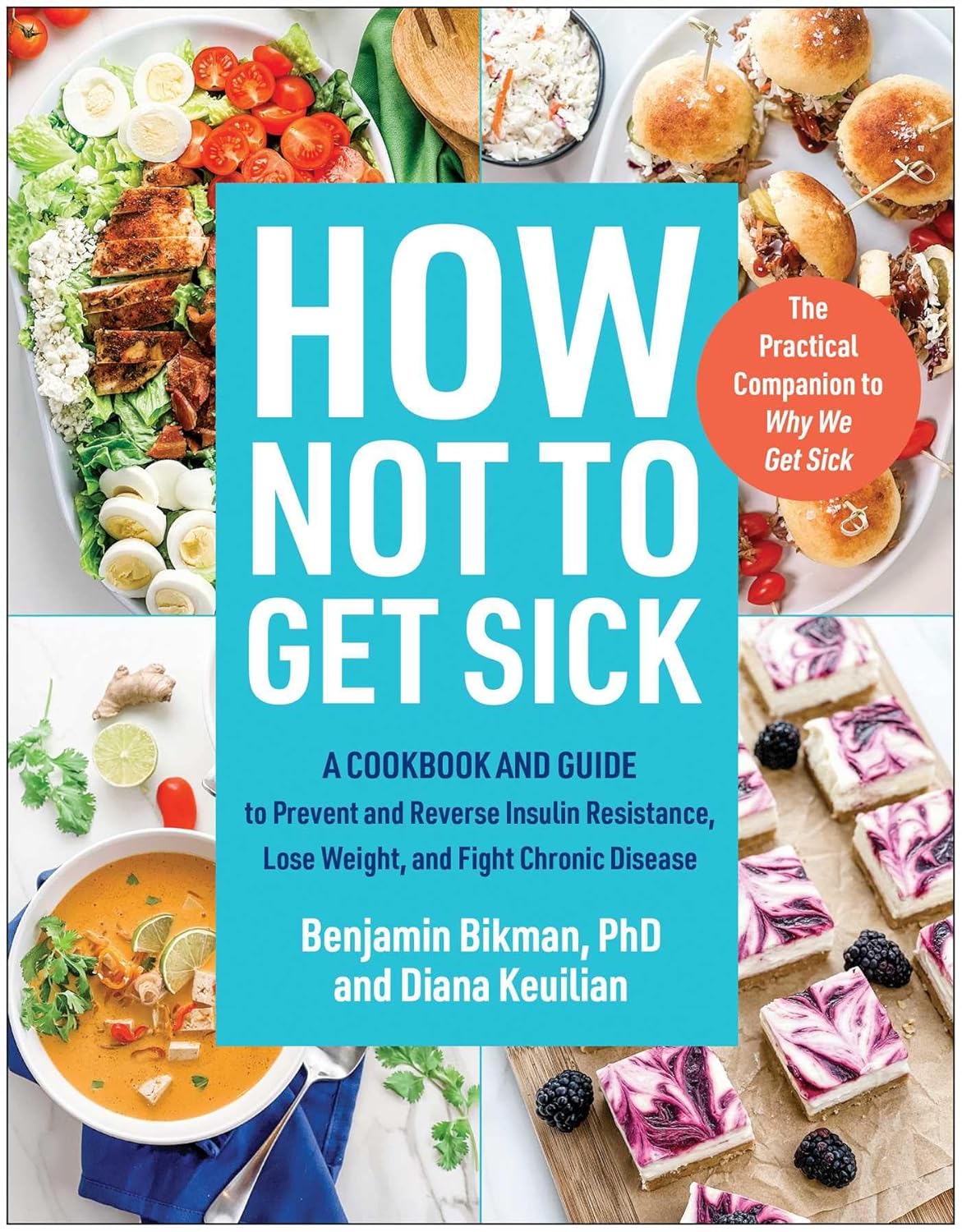
How Not To Get Sick: A Cookbook – by Dr. Benjamin Bikman and Diana Keuilian
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Dr. Bikman’s excellent “Why We Get Sick”, and if you haven’t read that yet, we recommend doing so.
Nevertheless, you don’t need to have read it to benefit from this one, which is about cooking with those learnings (from the other book) in mind.
Before getting to the recipes, we get a section recapping what we learned previously, as well as adding some more general lifestyle advices beyond the kitchen. The science is also expanded a bit, to include such things as the two-way relationship between insulin and aging, as well as the interplay with other metrics of health, including blood lipids, for example.
The authors then provide a plan, in the three stages: reverse (insulin resistance), prevent (insulin resistance), maintain (insulin sensitivity).
The recipes themselves, of which there are 70, are of course tailored to do the above three things; they’re also quite diverse, albeit if you are vegetarian or vegan, you should know in advance that most of these recipes are not.
Bottom line: if the above doesn’t apply to you, and you would like to improve your insulin sensitivity, this book can indeed help.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
High-Protein Plant-Based Diet for Beginners – by Maya Howard with Ariel Warren
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Seasoned vegans (well-seasoned vegans?) will know that getting enough protein from a plant-based diet is really not the challenge that many think it is, but for those just embarking on cutting out the meat, it’s not useful to say “it’s easy!”; it’s useful to show how.
That’s what this book does. And not just by saying “these foods” and leaving people to wonder if they need to eat a pound of tofu each day to get their protein in. Instead, recipes. Enough for a 4-week meal plan, and the idea is that after a month of eating that way, it won’t be nearly so mysterious.
The recipes are very easy to execute, while still having plenty of flavor (which is what happens when one uses a lot of flavorsome main ingredients and then seasons them well too). The ingredients are not obscure, and you should be able to find everything easily in any medium-sized supermarket.
As for the well-roundedness of the diet, we’ll mention that the “with Ariel Warren” in the by-line means that while the book was principally authored by Maya Howard (who is, at time of writing, a nutritionist-in-training), she had input throughout from Ariel Warren (a Registered Dietician Nutritionist) to ensure she didn’t go off-piste anyway and it gets the professional stamp of approval.
Bottom line: if you’d like to cook plant based while still prioritizing protein and you’re not sure how to make that exciting and fun instead of a chore, then this book will show you how to please your taste buds and improve your body composition at the same time.
Click here to check out High-Protein Plant-Based Diet for Beginners, and dig in!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Common Sense Labs: Blood Labs Demystified – by Dr. Ken Berry & Kim Howerton
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most people, if given their test results as a set of numbers, will have no idea what they mean.
And a doctor or nurse saying “this is good”, “this is a bit low”, “this is very high” etc isn’t that much more informative, as it doesn’t really give a true feel for the information.
Dr. Berry produced this book to bridge that knowledge gap, and in his words, “put the power of health back in the hands of the people”. The book also covers what blood tests to recommend annually (finding common recommendations insufficient), and how to go about asking for those if your doctor might be keen to brush you off.
This is a short book (weighing in at a lithe 78 pages), but the information contained therein is very dense, and very convenient to have it all in one place.
As one Amazon reviewer wrote,
❝Someone said you can find the information on the Internet, but I would say good luck with that. It will be many many many hours compiling the gold that is in this book.❞
Writer’s anecdote: indeed, I recently had 14 blood tests done as part of a regular checkup (I’m pleased to report I could not be in better health), and while interpreting the results, I had to look up a lot of things (which were often in the wrong units*), and if I’d had this book already, it would have been a breeze, as it covers everything I had done!
*On which note, this book does provide results in US and International units, so you won’t be left wondering how to convert mmol/mol into mmol/L or mg/dL or such.
Bottom line: if you are a person who has blood, this book will at some point be of immense value to you, if not immediately!
Click here to check out Common Sense Labs, and understand what your blood is saying!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: