Relationships: When To Stick It Out & When To Call It Quits
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Like A Ship Loves An Anchor?
Today’s article may seem a little bit of a downer to start with, but don’t worry, it picks up again too. Simply put, we’ve written before about many of the good parts of relationships, e.g:
Only One Kind Of Relationship Promotes Longevity This Much!
…but what if that’s not what we have?
Note: if you have a very happy, secure, fulfilling, joyous relationship, then, great! Or if you’re single and happy, then, also great! Hopefully you will still find today’s feature of use if you find yourself advising a friend or family member one day. So without further ado, let’s get to it…
You may be familiar with the “sunk cost fallacy”; if not: it’s what happens when a person or group has already invested into a given thing, such that even though the thing is not going at all the way they hoped, they now want to continue trying to make that thing work, lest their previous investment be lost. But the truth is: if it’s not going to work, then the initial investment is already lost, and pouring out extra won’t help—it’ll just lose more.
That “investment” in a given thing could be money, time, energy, or (often the case) a combination of the above.
In the field of romance, the “sunk cost fallacy” keeps a lot of bad relationships going for longer than perhaps they should, and looking back (perhaps after a short adjustment period), the newly-single person says “why did I let that go on?” and vows to not make the same mistake again.
But that prompts the question: how can we know when it’s right to “keep working on it, because relationships do involve work”, as perfectly reasonable relationship advice often goes, and when it’s right to call it quits?
Should I stay or should I go?
Some questions for you (or perhaps a friend you might find yourself advising) to consider:
- What qualities do you consider the most important for a partner to have—and does your partner have them?
- If you described the worst of your relationship to a close friend, would that friend feel bad for you?
- Do you miss your partner when they’re away, or are you glad of the break? When they return, are they still glad to see you?
- If you weren’t already in this relationship, would you seek to enter it now? (This takes away sunk cost and allows a more neutral assessment)
- Do you feel completely safe with your partner (emotionally as well as physically), or must you tread carefully to avoid conflict?
- If your partner decided tomorrow that they didn’t want to be with you anymore and left, would that be just a heartbreak, or an exciting beginning of a new chapter in your life?
- What things would you generally consider dealbreakers in a relationship—and has your partner done any of them?
The last one can be surprising, by the way. We often see or hear of other people’s adverse relationship situations and think “I would never allow…” yet when we are in a relationship and in love, there’s a good chance that we might indeed allow—or rather, excuse, overlook, and forgive.
And, patience and forgiveness certainly aren’t inherently bad traits to have—it’s just good to deploy them consciously, and not merely be a doormat.
Either way, reflect (or advise your friend/family member to reflect, as applicable) on the “score” from the above questions.
- If the score is good, then maybe it really is just a rough patch, and the tools we link at the top and bottom of this article might help.
- If the score is bad, the relationship is bad, and no amount of historic love or miles clocked up together will change that. Sometimes it’s not even anyone’s fault; sometimes a relationship just ran its course, and now it’s time to accept that and turn to a new chapter.
“At my age…”
As we get older, it’s easy for that sunk cost fallacy to loom large. Inertia is heavy, the mutual entanglement of lives is far-reaching, and we might not feel we have the same energy for dating that we did when we were younger.
And there may sometimes be a statistical argument for “sticking it out” at least for a while, depending on where we are in the relationship, per this study (with 165,039 participants aged 20–76), which found:
❝Results on mean levels indicated that relationship satisfaction decreased from age 20 to 40, reached a low point at age 40, then increased until age 65, and plateaued in late adulthood.
As regards the metric of relationship duration, relationship satisfaction decreased during the first 10 years of the relationship, reached a low point at 10 years, increased until 20 years, and then decreased again.❞
Source: Development of Relationship Satisfaction Across the Life Span: A Systematic Review and Meta-Analysis
And yet, when it comes to prospects for a new relationship…
- If our remaining life is growing shorter, then it’s definitely too short to spend in an unhappy relationship
- Maybe we really won’t find romance again… And maybe that’s ok, if w’re comfortable making our peace with that and finding joy in the rest of life (this widowed writer (hi, it’s me) plans to remain single now by preference, and her life is very full of purpose and beauty and joy and yes, even love—for family, friends, etc, plus the memory of my wonderful late beloved)
- Nevertheless, the simple fact is: many people do find what they go on to describe as their best relationship yet, late in life ← this study is with a small sample size, but in this case, even anecdotal evidence seems sufficient to make the claim reasonable; probably you personally know someone who has done so. If they can, so can you, if you so wish.
- Adding on to that last point… Later life relationships can also offer numerous significant advantages unique to such (albeit some different challenges too—but with the right person, those challenges are just a fun thing to tackle together). See for example:
An exploratory investigation into dating among later‐life women
And about those later-life relationships that do work? They look like this:
this one looks like the title says it all, but it really doesn’t, and it’s very much worth at least reading the abstract, if not the entire paper—because it talks a lot about the characteristics that make for happy or unhappy relationships, and the effect that those things have on people. It really is very good, and quite an easy read.
See again: Healthy Relationship, Healthy Life
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A New $16,000 Postpartum Depression Drug Is Here. How Will Insurers Handle It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A much-awaited treatment for postpartum depression, zuranolone, hit the market in December, promising an accessible and fast-acting medication for a debilitating illness. But most private health insurers have yet to publish criteria for when they will cover it, according to a new analysis of insurance policies.
The lack of guidance could limit use of the drug, which is both novel — it targets hormone function to relieve symptoms instead of the brain’s serotonin system, as typical antidepressants do — and expensive, at $15,900 for the 14-day pill regimen.
Lawyers, advocates, and regulators are watching closely to see how insurance companies will shape policies for zuranolone because of how some handled its predecessor, an intravenous form of the same drug called brexanolone, which came on the market in 2019. Many insurers required patients to try other, cheaper medications first — known as the fail-first approach — before they could be approved for brexanolone, which was shown in early trials reviewed by the FDA to provide relief within days. Typical antidepressants take four to six weeks to take effect.
“We’ll have to see if insurers cover this drug and what fail-first requirements they put in” for zuranolone, said Meiram Bendat, a licensed psychotherapist and an attorney who represents patients.
Most health plans have yet to issue any guidelines for zuranolone, and maternal health advocates worry that the few that have are taking a restrictive approach. Some policies require that patients first try and fail a standard antidepressant before the insurer will pay for zuranolone.
In other cases, guidelines require psychiatrists to prescribe it, rather than obstetricians, potentially delaying treatment since OB-GYN practitioners are usually the first medical providers to see signs of postpartum depression.
Advocates are most worried about the lack of coverage guidance.
“If you don’t have a published policy, there is going to be more variation in decision-making that isn’t fair and is less efficient. Transparency is really important,” said Joy Burkhard, executive director of the nonprofit Policy Center for Maternal Mental Health, which commissioned the study.
With brexanolone, which was priced at $34,000 for the three-day infusion, California’s largest insurer, Kaiser Permanente, had such rigorous criteria for prescribing it that experts said the policy amounted to a blanket denial for all patients, according to an NPR investigation in 2021.
KP’s written guidelines required patients to try and fail four medications and electroconvulsive therapy before they would be eligible for brexanolone. Because the drug was approved only for up to six months postpartum, and trials of typical antidepressants take four to six weeks each, the clock would run out before a patient had time to try brexanolone.
An analysis by NPR of a dozen other health plans at the time showed Kaiser Permanente’s policy on brexanolone to be an outlier. Some did require that patients fail one or two other drugs first, but KP was the only one that recommended four.
Miriam McDonald, who developed severe postpartum depression and suicidal ideation after giving birth in late 2019, battled Kaiser Permanente for more than a year to find effective treatment. Her doctors put her on a merry-go-round of medications that didn’t work and often carried unbearable side effects, she said. Her doctors refused to prescribe brexanolone, the only FDA-approved medication specifically for postpartum depression at the time.
“No woman should suffer like I did after having a child,” McDonald said. “The policy was completely unfair. I was in purgatory.”
One month after NPR published its investigation, KP overhauled its criteria to recommend that women try just one medication before becoming eligible for brexanolone.
Then, in March 2023, after the federal Department of Labor launched an investigation into the insurer — citing NPR’s reporting — the insurer revised its brexanolone guidelines again, removing all fail-first recommendations, according to internal documents recently obtained by NPR. Patients need only decline a trial of another medication.
“Since brexanolone was first approved for use, more experience and research have added to information about its efficacy and safety,” the insurer said in a statement. “Kaiser Permanente is committed to ensuring brexanolone is available when physicians and patients determine it is an appropriate treatment.”
“Kaiser basically went from having the most restrictive policy to the most robust,” said Burkhard of the Policy Center for Maternal Mental Health. “It’s now a gold standard for the rest of the industry.”
McDonald is hopeful that her willingness to speak out and the subsequent regulatory actions and policy changes for brexanolone will lead Kaiser Permanente and other health plans to set patient-friendly policies for zuranolone.
“This will prevent other women from having to go through a year of depression to find something that works,” she said.
Clinicians were excited when the FDA approved zuranolone last August, believing the pill form, taken once a day at home over two weeks, will be more accessible to women compared with the three-day hospital stay for the IV infusion. Many perinatal psychiatrists told NPR it is imperative to treat postpartum depression as quickly as possible to avoid negative effects, including cognitive and social problems in the baby, anxiety or depression in the father or partner, or the death of the mother to suicide, which accounts for up to 20% of maternal deaths.
So far, only one of the country’s six largest private insurers, Centene, has set a policy for zuranolone. It is unclear what criteria KP will set for the new pill. California’s Medicaid program, known as Medi-Cal, has not yet established coverage criteria.
Insurers’ policies for zuranolone will be written at a time when the regulatory environment around mental health treatment is shifting. The U.S. Department of Labor is cracking down on violations of the Mental Health Parity and Addiction Equity Act of 2008, which requires insurers to cover psychiatric treatments the same as physical treatments.
Insurers must now comply with stricter reporting and auditing requirements intended to increase patient access to mental health care, which advocates hope will compel health plans to be more careful about the policies they write in the first place.
In California, insurers must also comply with an even broader state mental health parity law from 2021, which requires them to use clinically based, expert-recognized criteria and guidelines in making medical decisions. The law was designed to limit arbitrary or cost-driven denials for mental health treatments and has been hailed as a model for the rest of the country. Much-anticipated regulations for the law are expected to be released this spring and could offer further guidance for insurers in California setting policies for zuranolone.
In the meantime, Burkhard said, patients suffering from postpartum depression should not hold back from asking their doctors about zuranolone. Insurers can still grant access to the drug on a case-by-case basis before they formalize their coverage criteria.
“Providers shouldn’t be deterred from prescribing zuranolone,” Burkhard said.
This article is from a partnership that includes KQED, NPR and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
You could be stress eating these holidays – or eating your way to stress. 5 tips for the table
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The holiday season can be a time of joy, celebration, and indulgence in delicious foods and meals. However, for many, it can also be an emotional and stressful period.
This stress can manifest in our eating habits, leading to what is known as emotional or stress eating.
There are certain foods we tend to eat more of when we’re stressed, and these can affect our health. What’s more, our food choices can influence our stress levels and make us feel worse. Here’s how.
Dean Clarke/Shutterstock Why we might eat more when stressed
The human stress response is a complex signalling network across the body and brain. Our nervous system then responds to physical and psychological events to maintain our health. Our stress response – which can be subtle or trigger a fight-or-flight response – is essential and part of daily life.
The stress response increases production of the hormones cortisol and insulin and the release of glucose (blood sugars) and brain chemicals to meet demand. Eating when we experience stress is a normal behaviour to meet a spike in energy needs.
But sometimes our relationship with food becomes strained in response to different types of stress. We might attach shame or guilt to overeating. And anxiety or insecurity can mean some people under-eat in stressful times.
Over time, people can start to associate eating with negative emotions – such as anger, sadness, fear or worry. This link can create behavioural cycles of emotional eating. “Emotional eaters” may go on to develop altered brain responses to the sight or smell of food.
What stress eating can do to the body
Stress eating can include binge eating, grazing, eating late at night, eating quickly or eating past the feeling of fullness. It can also involve craving or eating foods we don’t normally choose. For example, stressed people often reach for ultra-processed foods. While eating these foods is not necessarily a sign of stress, having them can activate the reward system in our brain to alleviate stress and create a pattern.
Short-term stress eating, such as across the holiday period, can lead to symptoms such as acid reflux and poor sleep – particularly when combined with drinking alcohol.
In the longer term, stress eating can lead to weight gain and obesity, increasing the risks of cancer, heart diseases and diabetes.
While stress eating may help reduce stress in the moment, long-term stress eating is linked with an increase in depressive symptoms and poor mental health.
If you do over eat at a big gathering, don’t try and compensate by eating very little the next day. Peopleimage.com – Yuri A/Shutterstock What we eat can make us more or less stressed
The foods we choose can also influence our stress levels.
Diets high in refined carbohydrates and sugar (such as sugary drinks, sweets, crackers, cakes and most chocolates) can make blood sugar levels spike and then crash.
Diets high in unhealthy saturated and trans fats (processed foods, animal fats and commercially fried foods) can increase inflammatory responses.
Rapid changes in blood sugar and inflammation can increase anxiety and can change our mood.
Meanwhile, certain foods can improve the balance of neurotransmitters in the brain that regulate stress and mood.
Omega-3 fatty acids, found in fish and flaxseeds, are known to reduce inflammation and support brain health. Magnesium, found in leafy greens and nuts, helps regulate cortisol levels and the body’s stress response.
Vitamin Bs, found in whole grains, nuts, seeds, beans and animal products (mostly B12), help maintain a healthy nervous system and energy metabolism, improving mood and cognitive performance.
5 tips for the holiday table and beyond
Food is a big part of the festive season, and treating yourself to delicious treats can be part of the fun. Here are some tips for enjoying festive foods, while avoiding stress eating:
1. slow down: be mindful about the speed of your eating. Slow down, chew food well and put down your utensils after each bite
2. watch the clock: even if you’re eating more food than you normally would, sticking to the same timing of eating can help maintain your body’s response to the food. If you normally have an eight-hour eating window (the time between your first meal and last meal of the day) then stick to this even if you’re eating more
3. continue other health behaviours: even if we are eating more food or different food during the festive season, try to keep up other healthy behaviours, such as sleep and exercise
4. stay hydrated: make sure to drink plenty of fluids, especially water. This helps our body function and can help with feelings of hunger. When our brain gets the message something has entered the stomach (what we drink) this can provide a temporary reduction in feelings of hunger
5. don’t restrict: if we have a big day of eating, it can be tempting to restrict eating in the days before or after. But it is never a good idea to overly constrain food intake. It can lead to more overeating and worsen stress.
Reaching for cookies late at night can be characteristic of stress eating. Stokkete/Shutterstock Plus 3 bonus tips to manage holiday stress
1. shift your thinking: try reframing festive stress. Instead of viewing it as “something bad”, see it as “providing the energy” to reach your goals, such as a family gathering or present shopping
2. be kind to yourself and others: practise an act of compassion for someone else or try talking to yourself as you would a friend. These actions can stimulate our brains and improve wellbeing
3. do something enjoyable: being absorbed in enjoyable activities – such as crafting, movement or even breathing exercises – can help our brains and bodies to return to a more relaxed state, feel steady and connected.
For support and more information about eating disorders, contact the Butterfly Foundation on 1800 33 4673 or Kids Helpline on 1800 551 800. If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14. In an emergency, call 000.
Saman Khalesi, Senior Lecturer and Discipline Lead in Nutrition, School of Health, Medical and Applied Sciences, CQUniversity Australia; Charlotte Gupta, Senior Postdoctoral Research Fellow, Appleton Institute, HealthWise research group, CQUniversity Australia, and Talitha Best, Professor of Psychology, NeuroHealth Lab, Appleton Institute, CQUniversity Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
How light tells you when to sleep, focus and poo
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is the next article in our ‘Light and health’ series, where we look at how light affects our physical and mental health in sometimes surprising ways. Read other articles in the series.
Exposure to light is crucial for our physical and mental health, as this and future articles in the series will show.
But the timing of that light exposure is also crucial. This tells our body to wake up in the morning, when to poo and the time of day to best focus or be alert. When we’re exposed to light also controls our body temperature, blood pressure and even chemical reactions in our body.
But how does our body know when it’s time to do all this? And what’s light got to do with it?
nymphoenix/Shutterstock What is the body clock, actually?
One of the key roles of light is to re-set our body clock, also known as the circadian clock. This works like an internal oscillator, similar to an actual clock, ticking away as you read this article.
But rather than ticking you can hear, the body clock is a network of genes and proteins that regulate each other. This network sends signals to organs via hormones and the nervous system. These complex loops of interactions and communications have a rhythm of about 24 hours.
In fact, we don’t have one clock, we have trillions of body clocks throughout the body. The central clock is in the hypothalamus region of the brain, and each cell in every organ has its own. These clocks work in concert to help us adapt to the daily cycle of light and dark, aligning our body’s functions with the time of day.
However, our body clock is not precise and works to a rhythm of about 24 hours (24 hours 30 minutes on average). So every morning, the central clock needs to be reset, signalling the start of a new day. This is why light is so important.
The central clock is directly connected to light-sensing cells in our retinas (the back of the eye). This daily re-setting of the body clock with morning light is essential for ensuring our body works well, in sync with our environment.
In parallel, when we eat food also plays a role in re-setting the body clock, but this time the clock in organs other than the brain, such as the liver, kidneys or the gut.
So it’s easy to see how our daily routines are closely linked with our body clocks. And in turn, our body clocks shape how our body works at set times of the day.
What time of day?
Matt Garrow/The Conversation. Adapted from Delos, CC BY Let’s take a closer look at sleep
The naturally occurring brain hormone melatonin is linked to our central clock and makes us feel sleepy at certain times of day. When it’s light, our body stops making melatonin (its production is inhibited) and we are alert. Closer to bedtime, the hormone is made, then secreted, making us feel drowsy.
Our sleep is also partly controlled by our genes, which are part of our central clock. These genes influence our chronotype – whether we are a “lark” (early riser), “night owl” (late sleeper) or a “dove” (somewhere in between).
But exposure to light at night when we are supposed to be sleeping can have harmful effects. Even dim light from light pollution can impair our heart rate and how we metabolise sugar (glucose), may lead to psychiatric disorders such as depression, anxiety and bipolar disorder, and increases the overall risk of premature death.
The main reason for these harmful effects is that light “at the wrong time” disturbs the body clock, and these effects are more pronounced for “night owls”.
This “misaligned” exposure to light is also connected to the detrimental health effects we often see in people who work night shifts, such as an increased risk of cancer, diabetes and heart disease.
How about the gut?
Digestion also follows a circadian rhythm. Muscles in the colon that help move waste are more active during the day and slow down at night.
The most significant increase in colon movement starts at 6.30am. This is one of the reasons why most people feel the urge to poo in the early morning rather than at night.
The gut’s day-night rhythm is a direct result of the action of the gut’s own clock and the central clock (which synchronises the gut with the rest of the body). It’s also influenced by when we eat.
At 6.30am, your gut really begins to get going for the day. Rendra Dria Septia Aji/Shutterstock How about focusing?
Our body clock also helps control our attention and alertness levels by changing how our brain functions at certain times of day. Attention and alertness levels improve in the afternoon and evening but dip during the night and early morning.
Those fluctuations impact performance and can lead to decreased productivity and an increased risk of errors and accidents during the less-alert hours.
So it’s important to perform certain tasks that require our attention at certain times of day. That includes driving. In fact, disruption of the circadian clock at the start of daylight savings – when our body hasn’t had a chance to adapt to the clocks changing – increases the risk of a car accident, particularly in the morning.
What else does our body clock control?
Our body clock influences many other aspects of our biology, including:
- physical performance by controlling the activity of our muscles
- blood pressure by controlling the system of hormones involved in regulating our blood volume and blood vessels
- body temperature by controlling our metabolism and our level of physical activity
- how our body handles drugs and toxins by controlling enzymes involved in how the liver and kidneys eliminate these substances from the body.
If you can, avoid driving long distances at night, as you’ll be less alert. trendobjects/Shutterstock Morning light is important
But what does this all mean for us? Exposure to light, especially in the morning, is crucial for synchronising our circadian clock and bodily functions.
As well as setting us up for a good night’s sleep, increased morning light exposure benefits our mental health and reduces the risk of obesity. So boosting our exposure to morning light – for example, by going for a walk, or having breakfast outside – can directly benefit our mental and metabolic health.
However, there are other aspects about which we have less control, including the genes that control our body clock.
Frederic Gachon, Associate Professor, Physiology of Circadian Rhythms, Institute for Molecular Bioscience, The University of Queensland and Benjamin Weger, NHMRC Emerging Leadership Fellow Institute for Molecular Bioscience, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
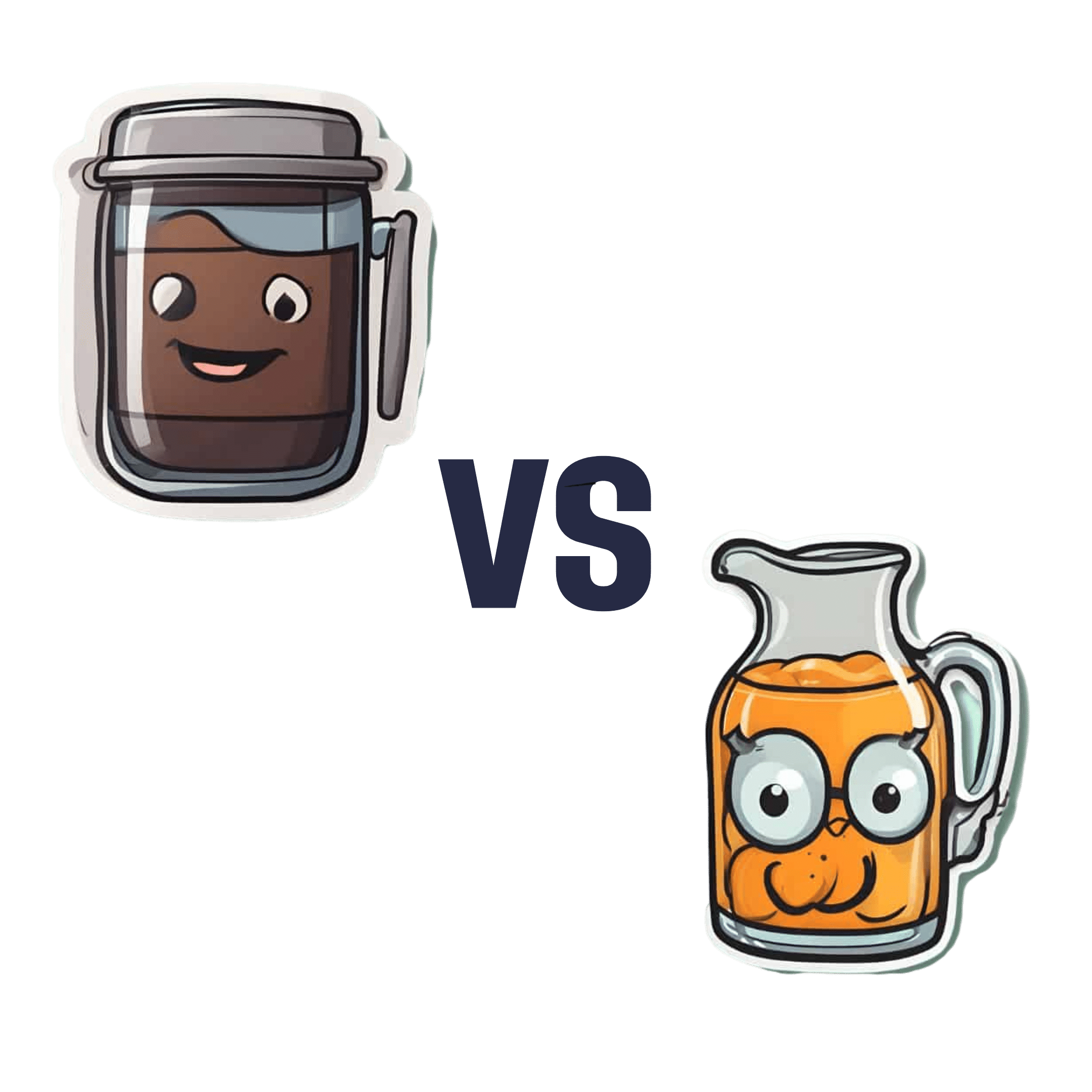
Black Coffee vs Orange Juice – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing black coffee to orange juice, we picked the coffee.
Why?
While this one isn’t a very like-for-like choice, it’s a choice often made, so it bears examining.
In favor of the orange juice, it has vitamins A and C and the mineral potassium, while the coffee contains no vitamins or minerals beyond trace amounts.
However, to offset that: drinking juice is one of the worst ways to consume sugar; the fruit has not only been stripped of its fiber, but also is in its most readily absorbable state (liquid), meaning that this is going to cause a blood sugar spike, which if done often can lead to insulin resistance, type 2 diabetes, non-alcoholic fatty liver disease, and more. Now, the occasional glass of orange juice (and resultant blood sugar spike) isn’t going to cause disease by itself, but everything we consume tips the scales of our health towards wellness or illness (or sometimes both, in different ways), and in this case, juice has a rather major downside that ought not be ignored.
In favor of the coffee, it has a lot of beneficial phytochemicals (mostly antioxidant polyphenols of various kinds), with no drawbacks worth mentioning unless you have a pre-existing condition of some kind.
Coffee can of course be caffeinated or decaffeinated, and we didn’t specify which here. Caffeine has some pros and cons that at worst, balance each other out, and whether or not it’s caffeinated, there’s nothing in coffee to offset the beneficial qualities of the antioxidants we mentioned before.
Obviously, in either case we are assuming consuming in moderation.
In short:
- orange juice has negatives that at least equal, if not outweigh, its positives
- coffee‘s benefits outweigh any drawbacks for most people
Want to learn more?
You might like to read:
- The Bitter Truth About Coffee (or is it?)
- Caffeine: Cognitive Enhancer Or Brain-Wrecker?
- Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fasting, eating earlier in the day or eating fewer meals – what works best for weight loss?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Globally, one in eight people are living with obesity. This is an issue because excess fat increases the risk of type 2 diabetes, heart disease and certain cancers.
Modifying your diet is important for managing obesity and preventing weight gain. This might include reducing your calorie intake, changing your eating patterns and prioritising healthy food.
But is one formula for weight loss more likely to result in success than another? Our new research compared three weight-loss methods, to see if one delivered more weight loss than the others:
- altering calorie distribution – eating more calories earlier rather than later in the day
- eating fewer meals
- intermittent fasting.
We analysed data from 29 clinical trials involving almost 2,500 people.
We found that over 12 weeks or more, the three methods resulted in similar weight loss: 1.4–1.8kg.
So if you do want to lose weight, choose a method that works best for you and your lifestyle.
chalermphon_tiam/Shutterstock Eating earlier in the day
When our metabolism isn’t functioning properly, our body can’t respond to the hormone insulin properly. This can lead to weight gain, fatigue and can increase the risk of a number of chronic diseases such as diabetes.
Eating later in the day – with a heavy dinner and late-night snacking – seems to lead to worse metabolic function. This means the body becomes less efficient at converting food into energy, managing blood sugar and regulating fat storage.
In contrast, consuming calories earlier in the day appears to improve metabolic function.
However, this might not be the case for everyone. Some people naturally have an evening “chronotype”, meaning they wake up and stay up later.
People with this chronotype appear to have less success losing weight, no matter the method. This is due to a combination of factors including genes, an increased likelihood to have a poorer diet overall and higher levels of hunger hormones.
Eating fewer meals
Skipping breakfast is common, but does it hinder weight loss? Or is a larger breakfast and smaller dinner ideal?
While frequent meals may reduce disease risk, recent studies suggest that compared to eating one to two meals a day, eating six times a day might increase weight loss success.
However, this doesn’t reflect the broader research, which tends to show consuming fewer meals can lead to greater weight loss. Our research suggests three meals a day is better than six. The easiest way to do this is by cutting out snacks and keeping breakfast, lunch and dinner.
Most studies compare three versus six meals, with limited evidence on whether two meals is better than three.
However, front-loading your calories (consuming most of your calories between breakfast and lunch) appears to be better for weight loss and may also help reduce hunger across the day. But more studies with a longer duration are needed.
Fasting, or time-restricted eating
Many of us eat over a period of more than 14 hours a day.
Eating late at night can throw off your body’s natural rhythm and alter how your organs function. Over time, this can increase your risk of type 2 diabetes and other chronic diseases, particularly among shift workers.
Time-restricted eating, a form of intermittent fasting, means eating all your calories within a six- to ten-hour window during the day when you’re most active. It’s not about changing what or how much you eat, but when you eat it.
Some people limit their calories to a six hour window, while others opt for ten hours. Shutterstock/NIKS ADS Animal studies suggest time-restricted eating can lead to weight loss and improved metabolism. But the evidence in humans is still limited, especially about the long-term benefits.
It’s also unclear if the benefits of time-restricted eating are due to the timing itself or because people are eating less overall. When we looked at studies where participants ate freely (with no intentional calorie limits) but followed an eight-hour daily eating window, they naturally consumed about 200 fewer calories per day.
What will work for you?
In the past, clinicians have thought about weight loss and avoiding weight gain as a simile equation of calories in and out. But factors such as how we distribute our calories across the day, how often we eat and whether we eat late at night may also impact our metabolism, weight and health.
There are no easy ways to lose weight. So choose a method, or combination of methods, that suits you best. You might consider
- aiming to eat in an eight-hour window
- consuming your calories earlier, by focusing on breakfast and lunch
- opting for three meals a day, instead of six.
The average adult gains 0.4 to 0.7 kg per year. Improving the quality of your diet is important to prevent this weight gain and the strategies above might also help.
Finally, there’s still a lot we don’t know about these eating patterns. Many existing studies are short-term, with small sample sizes and varied methods, making it hard to make direct comparisons.
More research is underway, including well-controlled trials with larger samples, diverse populations and consistent methods. So hopefully future research will help us better understand how altering our eating patterns can result in better health.
Hayley O’Neill, Assistant Professor, Faculty of Health Sciences and Medicine, Bond University and Loai Albarqouni, Assistant Professor | NHMRC Emerging Leadership Fellow, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
To Medicate or Not? That is the Question! – by Dr. Asha Bohannon
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Medications are, of course, a necessity of life (literally!) for many, especially as we get older. Nevertheless, overmedication is also a big problem that can cause a lot of harm too, and guess what, it comes with the exact same “especially as we get older” tag too.
So, what does Dr. Bohannon (a doctor of pharmacy, diabetes educator, and personal trainer too) recommend?
Simply put: she recommends starting with a comprehensive health history assessment and analysing one’s medication/supplement profile, before getting lab work done, tweaking all the things that can be tweaked along the way, and—of course—not neglecting lifestyle medicine either.
The book is prefaced and ended with pep talks that probably a person who has already bought the book does not need, but they don’t detract from the practical content either. Nevertheless, it feels a little odd that it takes until chapter 4 to reach “step 1” of her 7-step method!
The style throughout is conversational and energetic, but not overly padded with hype; it’s just a very casual style. Nevertheless, she brings to bear her professional knowledge and understanding as a doctor of pharmacy, to include her insights into the industry that one might not observe from outside of it.
Bottom line: if you’d like to do your own personal meds review and want to “know enough to ask the right questions” before bringing it up with your doctor, this book is a fine choice for that.
Click here to check out To Medicate Or Not, and make informed choices!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: