Rapamycin Can Slow Aging By 20% (But Watch Out)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Rapamycin’s Pros & Cons
Rapamycin is generally heralded as a wonderdrug that (according to best evidence so far) can slow down aging, potentially adding decades to human lifespan—and yes, healthspan.
It comes from a kind of soil bacteria, which in turn comes from the island of Rapa Nui (a Chilean territory best known for its monumental moai statues), hence the name rapamycin.
Does it work?
Yes! Probably! With catches!
Like most drugs that are tested for longevity-inducing properties, research in humans is very slow. Of course for drugs in general, they must go through in vitro and in vivo animal testing first before they can progress to human randomized clinical trials, but for longevity-inducing drugs, it’s tricky to even test in humans, without waiting entire human lifetimes for the results.
Nevertheless, mouse studies are promising:
Rapamycin: An InhibiTOR of Aging Emerges From the Soil of Easter Island
(“Easter Island” is another name given to the island of Rapa Nui)
That’s not a keysmash in the middle there, it’s a reference to rapamycin’s inhibitory effect on the kinase mechanistic target of rapamycin, sometimes called the mammalian target of rapamycin, and either way generally abbreviated to “mTOR”—also known as “FK506-binding protein 12-rapamycin-associated protein 1” or “FRAP1“ to its friends, but we’re going to stick with “mTOR”.
What’s relevant about this is that mTOR regulates cell growth, cell proliferation, cell motility, cell survival, protein synthesis, autophagy, and transcription.
Don’t those words usually get associated with cancer?
They do indeed! Rapamycin and its analogs have well-demonstrated anti-cancer potential:
❝Rapamycin, the naturally occurring inhibitor of mTOR, along with a number of recently developed rapamycin analogs (rapalogs) consisting of synthetically derived compounds containing minor chemical modifications to the parent structure, inhibit the growth of cell lines derived from multiple tumor types in vitro, and tumor models in vivo.
Results from clinical trials indicate that the rapalogs may be useful for the treatment of subsets of certain types of cancer.❞
…and as such, gets used sometimes as an anticancer drug—especially against renal cancer. See also:
Research perspective: Cancer prevention with rapamycin
What’s the catch?
Aside from the fact that its longevity-inducing effects are not yet proven in humans, the mouse models find its longevity effects to be sex-specific, extending the life of male mice but not female ones:
Rapamycin‐mediated mouse lifespan extension: Late‐life dosage regimes with sex‐specific effects
One hypothesis about this is that it may have at least partially to do with rapamycin’s immunomodulatory effect, bearing in mind that estrogen is immune-enhancing and testosterone is immunosuppressant.
And rapamycin? That’s another catch: it is an immunosuppressant.
This goes in rapamycin’s favor for its use to avoiding rejection when it comes to some transplants (most notably including for kidneys), though the very same immunosuppressant effect is a reason it is contraindicated for certain other transplants (such as in liver or lung transplants), where it can lead to an unacceptable increase in risk of lymphoma and other malignancies:
Prescribing Information: Rapamune, Sirolimus Solution / Sirolimus Tablet
(Sirolimus is another name for rapamycin, and Rapamune is a brand name)
What does this mean for the future?
Researchers think that rapamycin may be able to extend human lifespan to a more comfortable 120–125 years, but acknowledge there’s quite a jump to get there from the current mouse studies, and given the current drawbacks of sex-specificity and immunosuppression:
Advances in anti-aging: Rapamycin shows potential to extend lifespan and improve health
Noteworthily, rapamycin has also shown promise in simultaneously staving off certain diseases associated most strongly with aging, including Alzheimer’s and cardiac disease—or even, starting earlier, to delay menopause, in turn kicking back everything else that has an uptick in risk peri- or post-menopause:
Effect of Rapamycin in Ovarian Aging (Rapamycin)
👆 an upcoming study whose results are thus not yet published, but this is to give an idea of where research is currently at. See also:
Pilot Study Evaluates Weekly Pill to Slow Ovarian Aging, Delay Menopause
Where can I try it?
Not from Amazon, that’s for sure!
It’s still tightly regulated, but you can speak with your physician, especially if you are at risk of cancer, especially if kidney cancer, about potentially being prescribed it as a preventative—they will be able to advise about safety and applicability in your personal case.
Alternatively, you can try getting your name on the list for upcoming studies, like the one above. ClinicalTrials.gov is a great place to watch out for those.
Meanwhile, take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Singledom & Healthy Longevity
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Statistically, those who live longest, do so in happy, fulfilling, committed relationships.
Note: happy, fulfilling, committed relationships. Less than that won’t do. Your insurance company might care about your marital status for its own sake, but your actual health doesn’t—it’s about the emotional safety and security that a good, healthy, happy, fulfilling relationship offers.
We wrote about this here:
Only One Kind Of Relationship Promotes Longevity This Much!
But that’s not the full story
For a start, while being in a happy fulfilling committed relationship statistically adds healthy life years, being in a relationship that falls short of those adjectives certainly does not. See also:
Relationships: When To Stick It Out & When To Call It Quits
But also, life satisfaction steadily improves with age, for single people (the results are more complicated for partnered people—probably because of the range of difference in quality of relationships). At least, this held true in this large (n=6,188) study of people aged 40–85 years:
❝With advancing age, partnership status became less predictive of loneliness and the satisfaction with being single increased. Among later-born cohorts, the association between partnership status and loneliness was less strong than among earlier-born cohorts. Later-born single people were more satisfied with being single than their earlier-born counterparts.❞
Note that this does mean that while life satisfaction indeed improves with age for single people, that’s a generalized trend, and the greatest life satisfaction within this set of singles comes hand-in-hand with being single by choice rather than by perceived obligation, i.e., those who are “single and not looking” will generally be the most content, and this contentedness will improve with age, but for those who are “single and looking”, in that case it’s the younger people who have it better, likely due to a greater sense of having plenty of time.
For that matter, gender plays a role; this large survey of singles found that (despite the popular old pop-up ads advising that “older women in your area are looking to date”), in reality older single women were the least likely to actively look for a partner:
See: A Profile Of Single Americans
…which also shows that about half of single Americans are “not looking”, and of those who are, about half are open to a serious relationship, though this is more common under the age of 40, while being over the age of 40 sees more people looking only for something casual.
Take-away from this section: being single only decreases life satisfaction if one doesn’t enjoy being single, and even then, and increases it if one does enjoy being single.
But that’s about life satisfaction, not longevity
We found no studies specifically into longevity of singledom, only the implications that may be drawn from the longevity of partnered people.
However, there is a lot of research that shows it’s not being single that kills, it’s being socially isolated. It’s a function of neurodegeneration from a lack of conversation, and it’s a function of what happens when someone slips in the shower and is found a week later. Things like that.
For example: Is Living Alone “Aging Alone”? Solitary Living, Network Types, and Well-Being
What if you are alone and don’t want to be?
We’ve not, at time of writing, written dating advice in our Psychology Sunday section, but this writer’s advice is: don’t even try.
That’s not nihilism or even cynicism, by the way; it’s actually a kind of optimism. The trick is just to let them come to you.
(sample size of one here, but this writer has never looked for a relationship in her life, they’ve always just found me, and now that I’m widowed and intend to remain single, I still get offers—and no, I’m not a supermodel, nor rich, nor anything like that)
Simply: instead of trying to find a partner, just work on expanding your social relationships in general (which is much easier, because the process is something you can control, whereas the outcome of trying to find a suitable partner is not), and if someone who’s right for you comes along, great! If not, then well, at least you have a flock of friends now, and who knows what new unexpected romance may lie around the corner.
As for how to do that,
How To Beat Loneliness & Isolation
Take care!
Share This Post
-
The Mindgym: Wake Your Mind Up – by Dr. Sebastian Bailey and Octavius Black
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Since this reviewer got her copy, the subtitle and marketing of the book have changed, but the content has not. It’s now being marketed as “achieve more by thinking differently” like a pop-psychology business book. But it’s not that. What, then, is it?
It’s 20 chapters of exercises for different kinds of thinking. And yes, the exercises will help those hungry 25–35-year-old MBAs too, but it’s more of a complete how-to-think overhaul.
Its exercises cover psychology and philosophy, creativity and communication, logic and relaxation, cognition and motivation, and lots more.
The style of the book is that of a workbook, and as such, it’s very clearly laid-out; one can go through them methodically, or get an overview and then dive in to whatever one wants/needs most at the moment.
Bottom line: if you’d like a book that’s a one-stop shop for honing many different kinds of thinking, this is the book for you.
Click here to check out The Mindgym, and get training yours!
Share This Post
-
Which B Vitamins? It Makes A Difference
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Everyone knows “B vitamins are for energy!” and that is definitely a theme, but there’s a lot more to it than that, and in some cases, there are big mistakes that people make when it comes to supplementing their diet.
First, let’s do a quick overview of what each of the B vitamins do, by number, and putting names to them:
B1 (Thiamine)
- Function: helps convert carbohydrates into energy, supports nerve function
- Forms: thiamine hydrochloride, thiamine mononitrate, benfotiamine (fat-soluble form)
- Example foods: lentils, sunflower seeds
B2 (Riboflavin)
- Function: supports energy production, skin health, and eye function, turns your pee fluorescent yellow (the latter is really only if you consume exciting amounts of it; this will usually occur from supplementation, not from normal diet)
- Forms: riboflavin, riboflavin-5’-phosphate
- Example foods: almonds, mushrooms
B3 (Niacin)
- Function: aids metabolism, supports skin, nerves, and cholesterol levels
- Forms: niacin (nicotinic acid), niacinamide (nicotinamide), inositol hexanicotinate (flush-free niacin)
- Example foods: whole grains, peanuts (literally the best nut for this)
B5 (Pantothenic Acid)
- Function: essential for fatty acid metabolism and hormone production
- Forms: pantothenic acid, calcium pantothenate, panthenol (alcohol form!)
- Example foods: it’s in pretty much everything (hence the name); it’s almost impossible to be deficient in this vitamin unless you are literally starving
B6 (Pyridoxine)
- Function: needed for red blood cell production, supports brain function, as well as specifically being a part of neurotransmitter production (including dopamine and serotonin, despite them being made in different places—the brain and the gut, respectively),
- Forms: pyridoxine hydrochloride, pyridoxal-5’-phosphate (active form)
- Example foods: bananas, potatoes
B7 (Biotin)
- Function: helps with fatty acid synthesis, skin, hair, and nail health
- Forms: d-biotin, biotinylated compounds of various kinds
- Example foods: fava beans, walnuts
B9 (Folate/Folic Acid)
- Function: crucial for DNA synthesis, cell division, and fetal development
- Forms: folic acid, folinic acid, 5-methyltetrahydrofolate (5-MTHF, active form)
- Example foods: chickpeas, spinach ← we only mentioned one leafy green here for fairness, but leafy greens in general are great sources of vitamin B9, hence the name, from the Latin “folium”, meaning leaf.
B12 (Cobalamin)
- Function: supports red blood cell formation, nerve function, and DNA synthesis
- Forms: cyanocobalamin, methylcobalamin (active), hydroxocobalamin (active), adenosylcobalamin (active)
- Example foods: nutritional yeast, nori
You may be wondering: what about vitamins B4, B8, B10, and B11? Those are now vacant spots, that once contained things that are no longer considered vitamins.
Three Critical Vitamin B Mistakes That May Be Sabotaging Your Health
Some mistakes that people make include:
Not supplementing when necessary
This occurs most often after midlife, especially in women, and the most common deficiencies are B1, B9, and B12.
See also: These Signs Often Mean These Nutrient Deficiencies (Do You Have Any?)
While it’s tempting to think “if I have a good balanced diet, I won’t need…” but the fact is sometimes our diet isn’t as nutrient dense as we hope—often through no fault of our own! But many modern farming methods prioritize yield over nutritional value, and that can result in plants and animals that do not have the nutritional qualities they “should”.
We wrote about this a while back, weighing up the “supplementation vs diet alone” dilemma:
Does Our Diet Need A Little Help? ← this also has a very useful chart of which vitamins people usually get too little or too much of. Note however that the statement of marginally excessive folate is slightly misleading, as the data pool contains men and women aged 18–65, while B9 is mostly needed more by women, and especially around childbirth or menopause, so B9 is actually a very common deficiency, but here it’s being balanced out lots of men getting too much (because every multivitamin has it).
Supplementing to excess
Most B vitamins have a very high maximum tolerable dose, because (with the exception of where we marked otherwise) they are water-soluble, which means that if you take more than you need, you’ll just pee it out later. Hence the famous fluorescence, for example.
However, the fat soluble form of vitamin B1 is harder to get in and harder to get out.
As for the others, problems usually only occur if you take enough to cause toxicity, faster than you pee it out. In other words, go easy on those Berocca drinks!
Nevertheless, there are other problems that can arise:
Vitamin B6 is essential—but too much can be toxic. Here’s what to know to stay safe ← tl;dr: there are issues with it causing peripheral neuropathy at doses over 10mg (the safe dose is disputed, so we’re mentioning the lowest safe dose here, but you can read about the others in the article)
Getting forms that don’t work so well
Those different forms we listed? They are not all created equal! For example:
- Folic acid is cheap; unfortunately, it’s not absorbed or used well
- Cyanocobalamin is cheap; unfortunately, it’s not absorbed or used well
Let us quote a recent book review of ours:
❝Rather, the most common forms of vitamins B9 and B12 provided in supplements are folic acid and cyanocobalamin, respectively, which as he demonstrates with extensive research to back up his claims, cannot be easily absorbed or used especially well.
About those vitamers: a vitamer is simply a form of a vitamin—most vitamins we need can arrive in a variety of forms. In the case of vitamins B9 and B12, he advocates for ditching vitamers folic acid and cyanocobalamin, cheap as they are, and springing for bioactive vitamers L-methylfolate, methylcobalamin, and adenosylcobalamin.
He also discusses (again, just as well-evidenced as the above things) why we might struggle to get enough from our diet after a certain age. For example, if trying to get these vitamins from meat, 50% of people over 50 cannot manufacture enough stomach acid to break down that protein to release the vitamins.
And as for methyl-B12 vitamers, you might expect you can get those from meat, and technically you can, but they don’t occur in all animals, just in one kind of animal. Specifically, the kind that has the largest brain-to-body ratio. However, eating the meat of this animal can result in protein folding errors in general and Creutzfeldt–Jakob disease in particular, so the author does not recommend eating humans, however nutritionally convenient that would be.
All this means that supplementation after a certain age really can be a sensible way to do it—but do it wisely, and pick the right vitamers.❞
You can read that review in full here: Your Vitamins are Obsolete: The Vitamer Revolution – by Dr. Sheldon Zablow
Want to try those latter two?
We don’t sell them, but here for your convenience are example products on Amazon:
L-methylfolate (active form of vitamin B9)
Methylcobalamin, adenosylcobalamin, & hydroxocobalamin (active forms of vitamin B12)
Take care!
Share This Post
Related Posts
-
A short history of sunscreen, from basting like a chook to preventing skin cancer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Australians have used commercial creams, lotions or gels to manage our skin’s sun exposure for nearly a century.
But why we do it, the preparations themselves, and whether they work, has changed over time.
In this short history of sunscreen in Australia, we look at how we’ve slathered, slopped and spritzed our skin for sometimes surprising reasons.
At first, suncreams helped you ‘tan with ease’
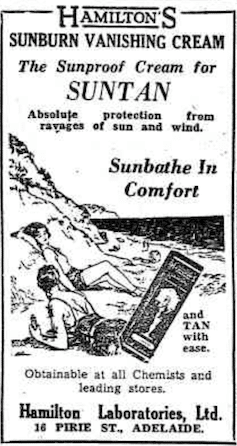
This early sunscreen claimed you could ‘tan with ease’.
Trove/NLASunscreens have been available in Australia since the 30s. Chemist Milton Blake made one of the first.
He used a kerosene heater to cook batches of “sunburn vanishing cream”, scented with French perfume.
His backyard business became H.A. Milton (Hamilton) Laboratories, which still makes sunscreens today.
Hamilton’s first cream claimed you could “
Sunbathe in Comfort and TAN with ease”. According to modern standards, it would have had an SPF (or sun protection factor) of 2.The mirage of ‘safe tanning’
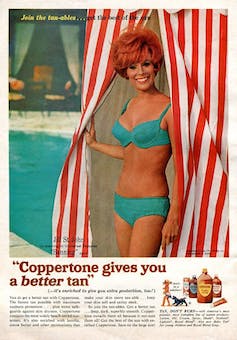
A tan was considered a “modern complexion” and for most of the 20th century, you might put something on your skin to help gain one. That’s when “safe tanning” (without burning) was thought possible.
This 1967 Coppertone advertisement urged you to ‘tan, not burn’.
SenseiAlan/Flickr, CC BY-SASunburn was known to be caused by the UVB component of ultraviolet (UV) light. UVA, however, was thought not to be involved in burning; it was just thought to darken the skin pigment melanin. So, medical authorities advised that by using a sunscreen that filtered out UVB, you could “safely tan” without burning.
But that was wrong.
From the 70s, medical research suggested UVA penetrated damagingly deep into the skin, causing ageing effects such as sunspots and wrinkles. And both UVA and UVB could cause skin cancer.
Sunscreens from the 80s sought to be “broad spectrum” – they filtered both UVB and UVA.
Researchers consequently recommended sunscreens for all skin tones, including for preventing sun damage in people with dark skin.
Delaying burning … or encouraging it?
Up to the 80s, sun preparations ranged from something that claimed to delay burning, to preparations that actively encouraged it to get that desirable tan – think, baby oil or coconut oil. Sun-worshippers even raided the kitchen cabinet, slicking olive oil on their skin.
One manufacturer’s “sun lotion” might effectively filter UVB; another’s merely basted you like a roast chicken.
Since labelling laws before the 80s didn’t require manufacturers to list the ingredients, it was often hard for consumers to tell which was which.
At last, SPF arrives to guide consumers
In the 70s, two Queensland researchers, Gordon Groves and Don Robertson, developed tests for sunscreens – sometimes experimenting on students or colleagues. They printed their ranking in the newspaper, which the public could use to choose a product.
An Australian sunscreen manufacturer then asked the federal health department to regulate the industry. The company wanted standard definitions to market their products, backed up by consistent lab testing methods.
In 1986, after years of consultation with manufacturers, researchers and consumers, Australian Standard AS2604 gave a specified a testing method, based on the Queensland researchers’ work. We also had a way of expressing how well sunscreens worked – the sun protection factor or SPF.
This is the ratio of how long it takes a fair-skinned person to burn using the product compared with how long it takes to burn without it. So a cream that protects the skin sufficiently so it takes 40 minutes to burn instead of 20 minutes has an SPF of 2.
Manufacturers liked SPF because businesses that invested in clever chemistry could distinguish themselves in marketing. Consumers liked SPF because it was easy to understand – the higher the number, the better the protection.
Australians, encouraged from 1981 by the Slip! Slop! Slap! nationwide skin cancer campaign, could now “slop” on a sunscreen knowing the degree of protection it offered.
How about skin cancer?
It wasn’t until 1999 that research proved that using sunscreen prevents skin cancer. Again, we have Queensland to thank, specifically the residents of Nambour. They took part in a trial for nearly five years, carried out by a research team led by Adele Green of the Queensland Institute of Medical Research. Using sunscreen daily over that time reduced rates of squamous cell carcinoma (a common form of skin cancer) by about 60%.
Follow-up studies in 2011 and 2013 showed regular sunscreen use almost halved the rate of melanoma and slowed skin ageing. But there was no impact on rates of basal cell carcinoma, another common skin cancer.
By then, researchers had shown sunscreen stopped sunburn, and stopping sunburn would prevent at least some types of skin cancer.
What’s in sunscreen today?
An effective sunscreen uses one or more active ingredients in a cream, lotion or gel. The active ingredient either works:
-
“chemically” by absorbing UV and converting it to heat. Examples include PABA (para-aminobenzoic acid) and benzyl salicylate, or
-
“physically” by blocking the UV, such as zinc oxide or titanium dioxide.
Physical blockers at first had limited cosmetic appeal because they were opaque pastes. (Think cricketers with zinc smeared on their noses.)
With microfine particle technology from the 90s, sunscreen manufacturers could then use a combination of chemical absorbers and physical blockers to achieve high degrees of sun protection in a cosmetically acceptable formulation.
Where now?
Australians have embraced sunscreen, but they still don’t apply enough or reapply often enough.
Although some people are concerned sunscreen will block the skin’s ability to make vitamin D this is unlikely. That’s because even SPF50 sunscreen doesn’t filter out all UVB.
There’s also concern about the active ingredients in sunscreen getting into the environment and whether their absorption by our bodies is a problem.
Sunscreens have evolved from something that at best offered mild protection to effective, easy-to-use products that stave off the harmful effects of UV. They’ve evolved from something only people with fair skin used to a product for anyone.
Remember, slopping on sunscreen is just one part of sun protection. Don’t forget to also slip (protective clothing), slap (hat), seek (shade) and slide (sunglasses).
Laura Dawes, Research Fellow in Medico-Legal History, Australian National University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
-
Why does alcohol make my poo go weird?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As we enter the festive season it’s a good time to think about what all those celebratory alcoholic drinks can do to your gut.
Alcohol can interfere with the time it takes for food to go through your gut (also known as the “transit time”). In particular, it can affect the muscles of the stomach and the small bowel (also known as the small intestine).
So, how and why does alcohol make your poos goes weird? Here’s what you need to know.
Diarrhoea and the ‘transit time’
Alcohol’s effect on stomach transit time depends on the alcohol concentration.
In general, alcoholic beverages such as whisky and vodka with high alcohol concentrations (above 15%) slow down the movement of food in the stomach.
Beverages with comparatively low alcohol concentrations (such as wine and beer) speed up the movement of food in the stomach.
These changes in gut transit explain why some people can get a sensation of fullness and abdominal discomfort when they drink vodka or whisky.
How long someone has been drinking a lot of alcohol can affect small bowel transit.
We know from experiments with rats that chronic use of alcohol accelerates the transit of food through the stomach and small bowel.
This shortened transit time through the small bowel also happens when humans drink a lot of alcohol, and is linked to diarrhoea.
Alcohol can also reduce the absorption of carbohydrates, proteins and fats in the duodenum (the first part of the small bowel).
Alcohol can lead to reduced absorption of xylose (a type of sugar). This means diarrhoea is more likely to occur in drinkers who also consume a lot of sugary foods such as sweets and sweetened juices.
Chronic alcohol use is also linked to:
- lactose intolerance
- overgrowth of small bowel bacteria and
- reduced absorption of fats from the pancreas not producing enough digestive enzymes.
This means chronic alcohol use may lead to diarrhoea and loose stools.
How might a night of heavy drinking affect your poos?
When rats are exposed to high doses of alcohol over a short period of time, it results in small bowel transit delay.
This suggests acute alcohol intake (such as an episode of binge drinking) is more likely to lead to constipation than diarrhoea.
This is backed up by recent research studying the effects of alcohol in 507 university students.
These students had their stools collected and analysed, and were asked to fill out a stool form questionnaire known as the Bristol Stool Chart.
The research found a heavy drinking episode was associated with harder, firm bowel motions.
In particular, those who consumed more alcohol had more Type 1 stools, which are separate hard lumps that look or feel a bit like nuts.
The researchers believed this acute alcohol intake results in small bowel transit delay; the food stayed for longer in the intestines, meaning more water was absorbed from the stool back into the body. This led to drier, harder stools.
Interestingly, the researchers also found there was more of a type of bacteria known as “Actinobacteria” in heavy drinkers than in non-drinkers.
This suggests bacteria may have a role to play in stool consistency.
But binge drinking doesn’t always lead to constipation. Binge drinking in patients with irritable bowel syndrom (IBS), for example, clearly leads to diarrhoea, nausea and abdominal pain.
What can I do about all this?
If you’re suffering from unwanted bowel motion changes after drinking, the most effective way to address this is to limit your alcohol intake.
Some alcoholic beverages may affect your bowel motions more than others. If you notice a pattern of troubling poos after drinking certain drinks, it may be sensible to cut back on those beverages.
If you tend to get diarrhoea after drinking, avoid mixing alcohol with caffeinated drinks. Caffeine is known to stimulate contractions of the colon and so could worsen diarrhoea.
If constipation after drinking is the problem, then staying hydrated is important. Drinking plenty of water before drinking alcohol (and having water in between drinks and after the party is over) can help reduce dehydration and constipation.
You should also eat before drinking alcohol, particularly protein and fibre-rich foods.
Food in the stomach can slow the absorption of alcohol and may help protect against the negative effects of alcohol on the gut lining.
Is it anything to worry about?
Changes in bowel motions after drinking are usually short term and, for the most part, resolve themselves pretty efficiently.
But if symptoms such as diarrhoea persist beyond a couple of days after stopping alcohol, it may signify other concerning issues such as an underlying gut disorder like inflammatory bowel disease.
Researchers have also linked alcohol consumption to the development of irritable bowel syndrome.
If problems persist or if there are alarming symptoms such as blood in your stool, seek medical advice from a general practitioner.
Vincent Ho, Associate Professor and clinical academic gastroenterologist, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How to Be Your Own Therapist – by Owen O’Kane
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Finding the right therapist can be hard. Sometimes, even just accessing a therapist, any therapist, can be hard, if circumstances are adverse. Sometimes we’d like therapy, but want to feel “better prepared for it” before we do.
Owen O’Kane, a highly qualified and well-respected psychotherapist, wants to put some tools in our hands. The premise of this book is that “in 10 minutes a day” one can give oneself an amount of therapy that will be beneficial.
Naturally, in 10 minutes a day, this isn’t going to be the kind of therapy that will work through major traumas, so what can it do?
Those 10 minutes are spread into three sessions:
- 4 minutes in the morning
- 3 minutes in the afternoon
- 3 minutes in the evening
The idea is:
- To do a quick mental health “check-in” before the day gets started, ascertain what one needs in that context, and make a simple plan to get/have it.
- To keep one’s mental health on track by taking a little pause to reassess and adjust if necessary
- To reflect on the day, amplify the positive, and let go of the negative to what extent is practical, in order to rest well ready for the next day
Where O’Kane excels is in explaining how to do those things in a way that is neither overly simplistic and wishy-washy, nor so arcane and convoluted as to create more work and render the day more difficult.
In short, this book is a great prelude to (or adjunct to) formal therapy, and for those for whom therapy isn’t accessible and/or desired, a great way to keep oneself on a mentally healthy track.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: