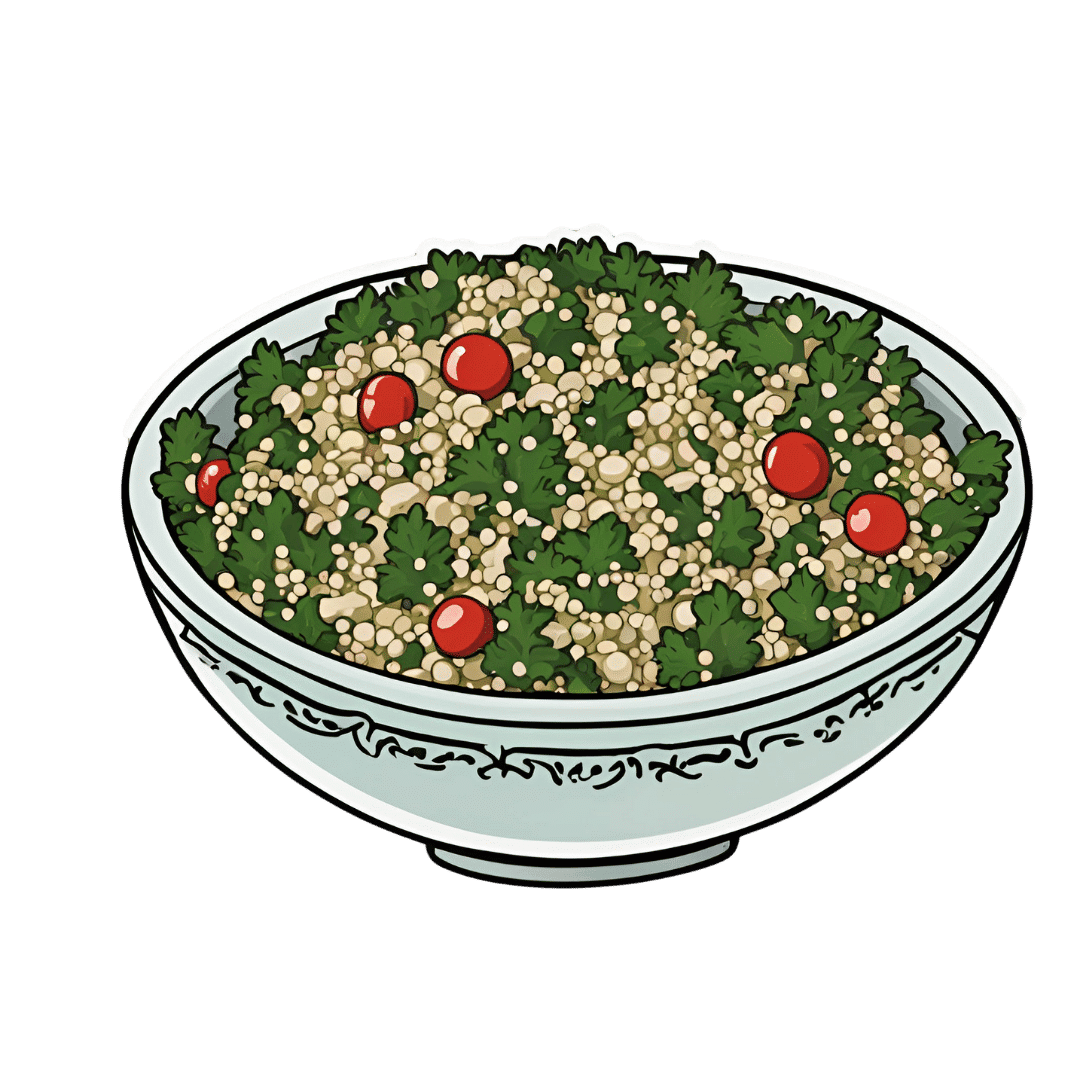
Quercetin Quinoa Probiotic Salad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This quercetin-rich salad is a bit like a tabbouleh in feel, with half of the ingredients switched out to maximize phenolic and gut-healthy benefits.
You will need
- ½ cup quinoa
- ½ cup kale, finely chopped
- ½ cup flat leaf parsley, finely chopped
- ½ cup green olives, thinly sliced
- ½ cup sun-dried tomatoes, roughly chopped
- 1 pomegranate, peel and pith removed
- 1 preserved lemon, finely chopped
- 1 oz feta cheese or plant-based equivalent, crumbled
- 1 tsp black pepper, coarse ground
- 1 tbsp capers
- 1 tbsp chia seeds
- 1 tbsp extra virgin olive oil
Note: you shouldn’t need salt or similar here, because of the diverse gut-healthy fermented products bringing their own salt with them
Method
(we suggest you read everything at least once before doing anything)
1) Rinse the quinoa, add the tbsp of chia seeds, cook as normal for quinoa (i.e. add hot water, bring to boil, simmer for 15 minutes or so until pearly and tender), carefully (don’t lose the chia seeds; use a sieve) drain and rinse with cold water to cool. Shake off excess water and/or pat dry on kitchen paper if necessary.
2) Mix everything gently but thoroughly.
3) Serve:

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Tasty Tabbouleh with Tahini ← in case you want an actual tabbouleh
- Making Friends With Your Gut (You Can Thank Us Later)
- Fight Inflammation & Protect Your Brain, With Quercetin
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Walking can prevent low back pain, a new study shows
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Do you suffer from low back pain that recurs regularly? If you do, you’re not alone. Roughly 70% of people who recover from an episode of low back pain will experience a new episode in the following year.
The recurrent nature of low back pain is a major contributor to the enormous burden low back pain places on individuals and the health-care system.
In our new study, published today in The Lancet, we found that a program combining walking and education can effectively reduce the recurrence of low back pain.
PeopleImages.com – Yuri A/Shutterstock The WalkBack trial
We randomly assigned 701 adults who had recently recovered from an episode of low back pain to receive an individualised walking program and education (intervention), or to a no treatment group (control).
Participants in the intervention group were guided by physiotherapists across six sessions, over a six-month period. In the first, third and fifth sessions, the physiotherapist helped each participant to develop a personalised and progressive walking program that was realistic and tailored to their specific needs and preferences.
The remaining sessions were short check-ins (typically less than 15 minutes) to monitor progress and troubleshoot any potential barriers to engagement with the walking program. Due to the COVID pandemic, most participants received the entire intervention via telehealth, using video consultations and phone calls.
Low back pain can be debilitating. Karolina Kaboompics/Pexels The program was designed to be manageable, with a target of five walks per week of roughly 30 minutes daily by the end of the six-month program. Participants were also encouraged to continue walking independently after the program.
Importantly, the walking program was combined with education provided by the physiotherapists during the six sessions. This education aimed to give people a better understanding of pain, reduce fear associated with exercise and movement, and give people the confidence to self-manage any minor recurrences if they occurred.
People in the control group received no preventative treatment or education. This reflects what typically occurs after people recover from an episode of low back pain and are discharged from care.
What the results showed
We monitored the participants monthly from the time they were enrolled in the study, for up to three years, to collect information about any new recurrences of low back pain they may have experienced. We also asked participants to report on any costs related to their back pain, including time off work and the use of health-care services.
The intervention reduced the risk of a recurrence of low back pain that limited daily activity by 28%, while the recurrence of low back pain leading participants to seek care from a health professional decreased by 43%.
Participants who received the intervention had a longer average period before they had a recurrence, with a median of 208 days pain-free, compared to 112 days in the control group.
In our study, regular walking appeared to help with low back pain. PeopleImages.com – Yuri A/Shutterstock Overall, we also found this intervention to be cost-effective. The biggest savings came from less work absenteeism and less health service use (such as physiotherapy and massage) among the intervention group.
This trial, like all studies, had some limitations to consider. Although we tried to recruit a wide sample, we found that most participants were female, aged between 43 and 66, and were generally well educated. This may limit the extent to which we can generalise our findings.
Also, in this trial, we used physiotherapists who were up-skilled in health coaching. So we don’t know whether the intervention would achieve the same impact if it were to be delivered by other clinicians.
Walking has multiple benefits
We’ve all heard the saying that “prevention is better than a cure” – and it’s true. But this approach has been largely neglected when it comes to low back pain. Almost all previous studies have focused on treating episodes of pain, not preventing future back pain.
A limited number of small studies have shown that exercise and education can help prevent low back pain. However, most of these studies focused on exercises that are not accessible to everyone due to factors such as high cost, complexity, and the need for supervision from health-care or fitness professionals.
On the other hand, walking is a free, accessible way to exercise, including for people in rural and remote areas with limited access to health care.
Walking has a variety of advantages. Cast Of Thousands/Shutterstock Walking also delivers many other health benefits, including better heart health, improved mood and sleep quality, and reduced risk of several chronic diseases.
While walking is not everyone’s favourite form of exercise, the intervention was well-received by most people in our study. Participants reported that the additional general health benefits contributed to their ongoing motivation to continue the walking program independently.
Why is walking helpful for low back pain?
We don’t know exactly why walking is effective for preventing back pain, but possible reasons could include the combination of gentle movements, loading and strengthening of the spinal structures and muscles. It also could be related to relaxation and stress relief, and the release of “feel-good” endorphins, which block pain signals between your body and brain – essentially turning down the dial on pain.
It’s possible that other accessible and low-cost forms of exercise, such as swimming, may also be effective in preventing back pain, but surprisingly, no studies have investigated this.
Preventing low back pain is not easy. But these findings give us hope that we are getting closer to a solution, one step at a time.
Tash Pocovi, Postdoctoral research fellow, Department of Health Sciences, Macquarie University; Christine Lin, Professor, Institute for Musculoskeletal Health, University of Sydney; Mark Hancock, Professor of Physiotherapy, Macquarie University; Petra Graham, Associate Professor, School of Mathematical and Physical Sciences, Macquarie University, and Simon French, Professor of Musculoskeletal Disorders, Macquarie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
The Painkilling Power Of Opioids, Without The Harm?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to painkilling medications, they can generally be categorized into two kinds:
- non-opioids (e.g. ibuprofen, paracetamol/acetaminophen, aspirin)
- ones that actually work for something more serious than a headache
That’s an oversimplification, but broadly speaking, when there is serious painkilling to be done, that’s when doctors consider it’s time to break out the opioids.
Nor are all opioids created equal—there’s a noteworthy difference between codeine and morphine, for instance—but the problems of opioids are typically the same (tolerance, addiction, and eventual likelihood of overdose when one tries to take enough to make it work after developing a tolerance), and it becomes simply a matter of degree.
See also: I’ve been given opioids after surgery to take at home. What do I need to know?
So, what’s the new development?
A team of researchers have found that the body can effectively produce its own targetted painkilling peptides, similar in function to benzodiazepines (an opioid drug), but—and which is a big difference—confined to the peripheral nervous system (PNS), meaning that it doesn’t enter the brain.
- The peptides killing the pain before it can reach the brain is obviously good because that means the pain is simply not experienced
- The peptides not having any effect on the brain, however, means that the mechanism of addiction of opioids simply does not apply here
- The peptides not having any effect on the brain also means that the CNS can’t be “put to sleep” by these peptides in the same way it can if a high dose of opioids is taken (this is what typically causes death in opioid overdoses; the heart simply beats too slowly to maintain life)
The hope, therefore, is to now create medications that target the spinal ganglia that produce these peptides, to “switch them on” at will.
Obviously, this won’t happen overnight; there will need to be first a lot of research to find a drug that does that (likely this will involve a lot of trial and error and so many mice/rats), and then multiple rounds of testing to ascertain that the drug is safe and effective for humans, before it can then be rolled out commercially.
But, this is still a big breakthrough; there arguably hasn’t been a breakthrough this big in pain research since various opioid-related breakthroughs in the 70s and 80s.
You can see a pop-science article about it here:
And you can see the previous research (from earlier this year) that this is now building from, about the glial cells in the spinal ganglia, here:
Peripheral gating of mechanosensation by glial diazepam binding inhibitor
But wait, there’s more!
Remember what we said about affecting the PNS without affecting the CNS, to kill the pain without killing the brain?
More researchers are already approaching the same idea to deal with the same problem, but from the angle of gene therapy, and have already had some very promising results with mice:
Structure-guided design of a peripherally restricted chemogenetic system
…which you can read about in pop-science terms (with diagrams!) here:
New gene therapy could alleviate chronic pain, researchers find
While you’re waiting…
In the meantime, approaches that are already available include:
- The 7 Approaches To Pain Management
- Managing Chronic Pain (Realistically!)
- Science-Based Alternative Pain Relief ← when painkillers aren’t helping, these things might!
Take care!
Share This Post
-
Plant-Based Alternatives for Meat Recipes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝How about providing a plant-based alternative when you post meat-based recipes? I appreciate how much you advocate for veggie diets and think offering an alternative with your recipes would support that❞
Glad you’re enjoying! And yes, we do usually do that. But: pardon, we missed one (the Tuna Steak with Protein Salad) because it’d be more than a simple this-for-that substitution, we didn’t already have an alternative recipe up (as with the salmon recipes such as the Chili Hot-Bedded Salmon and Thai Green Curry Salmon Burgers).
Our recipes, by the way, will tend towards being vegan, vegetarian, or at least pescatarian. This is for several reasons:
- Good science suggests the best diet for general purpose good health is one that is mostly plants, with optional moderate amounts of fermented dairy products, fish, and/or eggs.
- Your writer here (it’s me, hi) has been vegan for many years, transitioning to such via pescatarianism and ovo-lacto vegetarianism, and so the skill of cooking meat is least fresh in my memory, meaning I’d not be confident writing about that, especially as cooking meat has the gravest health consequences for messing it up.
Note on biases: notwithstanding this writer being vegan, we at 10almonds are committed to reporting the science as it stands with no agenda besides good health. Hence, there will continue to be unbiased information about animal products’ health considerations, positive as well as negative.
See also: Do We Need Animal Products To Be Healthy?
…as well as, of course, some animal-based classics from our archives including:
We Are Such Stuff As Fish Are Made Of & Eggs: All Things In Moderation?
Finishing with one for the vegans though, you might enjoy:
Which Plant Milk? We Compare 6 Of The Most Popular
Some previous articles you might enjoy meanwhile:
- Pinpointing The Usefulness Of Acupuncture
- Science-Based Alternative Pain Relief
- Peripheral Neuropathy: How To Avoid It, Manage It, Treat It
- What Does Lion’s Mane Actually Do, Anyway?
Take care!
Share This Post
Related Posts
-
What Seasonal Allergies Mean For Your Heart
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most people associate seasonal allergies with itchy eyes and stuffy noses, but the effects can go a lot deeper.
This is because allergic reactions don’t just affect the respiratory system; they trigger chronic inflammation throughout the body, and in fact:
❝Allergic disease is a systemic and inflammatory condition❞
~ Dr. Rauno Joks, whose work we will cite in a moment
The important thing to understand in terms of heart health, is that chronic* systemic inflammation can contribute to coronary artery disease, where plaque buildup in arteries (bearing in mind, arterial plaque is in large part made of dead immune cells) raises the risk of heart attacks and strokes.
*Yes, a season once or twice per year counts as “chronic”.
A large (n=603,140) study found that allergic rhinitis (hay fever) increased the odds of coronary heart disease by 25% and heart attacks by 20%. Asthma, especially during flare-ups, posed an even greater risk:
Beyond biology
The effects aren’t just biological; allergies can limit physical activity, leading to a sedentary lifestyle that harms heart health.
In other words: if you’re not going outdoors because there’s pollen, and you’re not exercising because you’re exhausted, then the rest of your health is going to take a nose-dive (so to speak) too.
So, one more reason to take it seriously and not just dismiss it as “it’s just allergies, I’ll survive”.
Practical takeaways
Some things we can all do:
- Monitor your risk factors; i.e. keep on top of your heart health metrics, especially blood pressure and cholesterol, as well as any known genetic predisposition to cardiovascular disease.
- Watch out for alternative causes: symptoms like fatigue or shortness of breath may not always be allergies; they could signal asthma, reflux (for example if wheezing), or even heart disease. An allergist is a good first port-of-call, though.
- Be cautious with medications: some decongestants / allergy meds / asthma meds can raise blood pressure and/or interfere with other medications. Your pharmacist is the best person to speak to about this; they know this kind of thing much better than doctors, as a rule. And whenever you get a new medication, it is good practice to make a habit of always reading the information leaflet that comes with it, and/or look it up on a reputable website such as Drugs.com or the the BNF, to learn about what it is, how it works, what the risks are, what its contraindications are, etc.
- Don’t ignore warning signs: lightheadedness or chest pain could indicate a heart issue and should be addressed immediately. It’s better to be wrong and temporarily embarrassed, than wrong and permanently dead. Besides, even if it’s not a heart issue, it may be something else that would benefit from attention, so taking it seriously is always a good idea.
Want to know more?
Check out:
- What Your Mucus Says About Your Health
- Antihistamines’ Generation Gap
- Oh, Honey: The Bee’s Knees? ← what science has to say about “honey will inoculate you against allergies”
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Your Metabolism Says About How Aggressive Breast Cancer Is Likely To Be For You
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ll get straight to it:
More than 120 million Americans have diabetes or pre-diabetes, and Triple-Negative Breast Cancer (TNBC)* is the most aggressive breast cancer form.
These may seem like unrelated statements, until we consider that patients with obesity-driven** diabetes have much worse TNBC outcomes.
*The “triple-negative” refers to:
- the cancer cells don’t have estrogen receptors
- the cancer cells don’t have progesterone receptors
- the cancer cells don’t make the protein HER2, or at least not in clinically relevant amounts.
**with regard to “obesity-driven”, that is what it is called, and the presence of excess fat does play an important role as we will see, but the fundamental culprit is insulin resistance, as we will also see.
The connection
Superficially, the connection between obesity-driven diabetes and worse TNBC outcomes could be put down to “a person who is already unhealthy will generally fare worse in most health things than an otherwise healthy person”. And, in and of itself, that’s a fair point. Comorbidities certainly do tend to flock together and make each other worse.
On the flipside, this does also mean that the more points of good health we have in our favor, the greater our chances of faring better if something (such as a cancer) does strike us regardless. So, there’s a fair motivation to always keep on top of all aspects of health, so far as reasonably possible.
However, there’s more to it than that.
Dr. Naomi Ko et al., a team of researchers at Boston University, found that diabetes alters breast cancer biology, making TNBC more aggressive and increasing the risk of brain metastasis (i.e., the cancer spreading to the brain).
Specifically, exosomes from fat cells carry microRNAs that worsen TNBC behavior, enhancing the cancer’s:
- cell growth
- movement
- survival under stress
- brain colonization
This also means that certain microRNA patterns predict breast cancer progression and/or survival.
You can find the paper itself here:
Insulin Resistance Increases TNBC Aggressiveness and Brain Metastasis via Adipocyte-derived Exosomes
Why this matters
The researchers argue that their findings suggest the need for special monitoring and treatment for TNBC patients with metabolic disorders like diabetes, and that treating underlying conditions (such as diabetes) alongside cancer is likely to improve outcomes.
On an individual level rather than systemic (assuming you, dear reader, to be a private individual who is not, for example, in charge of health policy for a region, or something like that), what this means is:
We must avoid carrying too much excess fat yes, and/but we must also particularly focus on avoiding/reversing insulin resistance, which can be a silent killer even without excess adiposity, because the noticeable signs and symptoms (including blood sugar irregularities) occur only well into insulin resistance, when the poor overworked pancreas can no longer crank out enough insulin to keep things ticking over.
With that in mind, do check out in particular the two following articles:
How To Lose Weight (Healthily!) ← if applicable. If on the other hand you’re already in the “healthy” body fat percentage range of 20–25% for women or 15–20% for men, then losing what fat you have will not be beneficial, and may even be harmful, depending on other factors.
How To Avoid & Reverse Insulin Resistance ← this one’s super-important!
And of course:
How To Triple Your Breast Cancer Survival Chances
And if you want to get really well-informed, then we highly recommend checking out:
The Smart Woman’s Guide to Breast Cancer – by Dr. Jenn Simmons
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
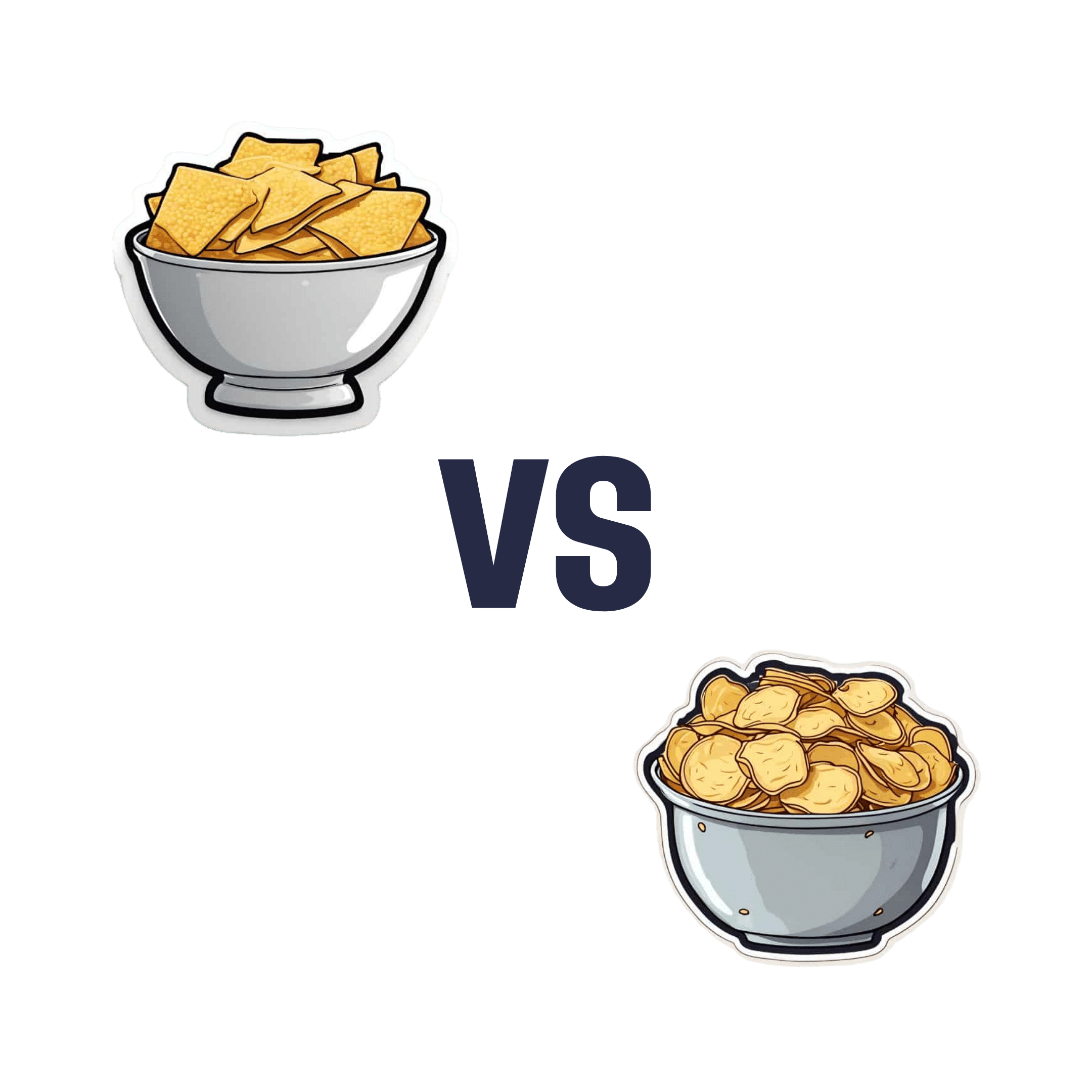
Corn Chips vs Potato Chips: Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing corn chips to potato chips, we picked the corn chips.
Why?
First, let it be said, this was definitely a case of “lesser evil voting” as there was no healthy choice here. But as for which is relatively least unhealthy…
Most of the macronutrient and micronutrient profile is quite similar. Both foods are high carb, moderately high fat, negligible protein, and contain some trace minerals and even some tiny amounts of vitamins. Both are unhealthily salty.
Exact numbers will of course vary from one brand’s product to another, but you can see some indicative aggregate scores here in the USDA’s “FoodData Central” database:
The biggest health-related difference that doesn’t have something to balance it out is that the glycemic index of corn chips averages around 63, whereas the glycemic index of potato chips averages around 70 (that is worse).
That’s enough to just about tip the scales in favor of corn chips.
The decision thus having been made in favor of corn chips (and the next information not having been part of that decision), we’ll mention one circumstantial extra benefit to corn chips:
Corn chips are usually eaten with some kind of dip (e.g. guacamole, sour cream, tomato salsa, etc) which can thus deliver actual nutrients. Potato chips meanwhile are generally eaten with no additional nutrients. So while we can’t claim the dip as being part of the nutritional make-up of the corn chips, we can say:
If you’re going to have a habit of eating one or the other, then corn chips are probably the least unhealthy of the two.
And yes, getting vegetables (e.g. in the dips) in ways that are not typically associated with “healthy eating” is still better than not getting vegetables at all!
Check out: Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: