Psychoactive Drugs Are Having a Moment. The FDA Will Soon Weigh In.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Lori Tipton is among the growing number of people who say that MDMA, also known as ecstasy, saved their lives.
Raised in New Orleans by a mother with untreated bipolar disorder who later killed herself and two others, Tipton said she endured layers of trauma that eventually forced her to seek treatment for crippling anxiety and hypervigilance. For 10 years nothing helped, and she began to wonder if she was “unfixable.”
Then she answered an ad for a clinical trial for MDMA-assisted therapy to treat post-traumatic stress disorder. Tipton said the results were immediate, and she is convinced the drug could help a lot of people. But even as regulators weigh approval of the first MDMA-based treatment, she’s worried that it won’t reach those who need it most.
“The main thing that I’m always concerned about is just accessibility,” the 43-year-old nonprofit project manager said. “I don’t want to see this become just another expensive add-on therapy for people who can afford it when people are dying every day by their own hand because of PTSD.”
MDMA is part of a new wave of psychoactive drugs that show great potential for treating conditions such as severe depression and PTSD. Investors are piling into the nascent field, and a host of medications based on MDMA, LSD, psychedelic mushrooms, ketamine, the South American plant mixture ayahuasca, and the African plant ibogaine are now under development, and in some cases vying for approval by the Food and Drug Administration.
Proponents hope the efforts could yield the first major new therapies for mental illness since the introduction of modern antidepressants in the 1980s. But not all researchers are convinced that their benefits have been validated, or properly weighed against the risks. And they can be difficult to assess using traditional clinical trials.
The first MDMA-assisted assisted therapy appeared to be on track for FDA approval this August, but a recent report from an independent review committee challenged the integrity of the trial data from the drug’s maker, Lykos Therapeutics, a startup founded by a psychedelic research and advocacy group. The FDA will convene a panel of independent investigators on June 4 to determine whether to recommend the drug’s approval.
Proponents of the new therapies also worry that the FDA will impose treatment protocols, such as requiring multiple trained clinicians to monitor a patient for extended periods, that will render them far too expensive for most people.
Tipton’s MDMA-assisted therapy included three eight-hour medication sessions overseen by two therapists, each followed by an overnight stay at the facility and an integration session the following day.
“It does seem that some of these molecules can be administered safely,” said David Olson, director of the University of California-Davis Institute for Psychedelics and Neurotherapeutics. “I think the question is can they be administered safely at the scale needed to really make major improvements in mental health care.”
Breakthrough Therapies?
Psychedelics and other psychoactive substances, among the medicines with the oldest recorded use, have long been recognized for their potential therapeutic benefits. Modern research on them started in the mid-20th century, but clinical trial results didn’t live up to the claims of advocates, and they eventually got a bad name both from their use as party drugs and from rogue CIA experiments that involved dosing unsuspecting individuals.
The 1970 Controlled Substances Act made most psychoactive drugs illegal before any treatments were brought to market, and MDMA was classified as a Schedule 1 substance in 1985, which effectively ended any research. It wasn’t until 2000 that scientists at Johns Hopkins University were granted regulatory approval to study psilocybin anew.
Ketamine was in a different category, having been approved as an anesthetic in 1970. In the early 2000s, researchers discovered its antidepressant effects, and a ketamine-based therapy, Spravato, received FDA approval in 2019. Doctors can also prescribe generic ketamine off-label, and hundreds of clinics have sprung up across the nation. A clinical trial is underway to evaluate ketamine’s effectiveness in treating suicidal depression when used with other psychiatric medications.
Ketamine’s apparent effectiveness sparked renewed interest in the therapeutic potential of other psychoactive substances.
They fall into distinct categories: MDMA is an entactogen, also known as an empathogen, which induces a sense of connectedness and emotional communion, while LSD, psylocibin, and ibogaine are psychedelics, which create altered perceptual states. Ketamine is a dissociative anesthetic, though it can produce hallucinations at the right dose.
Despite the drugs’ differences, Olson said they all create neuroplasticity and allow the brain to heal damaged neural circuits, which imaging shows can be shriveled up in patients with addiction, depression, and PTSD.
“All of these brain conditions are really disorders of neural circuits,” Olson said. “We’re basically looking for medicines that can regrow these neurons.”
Psychedelics are particularly good at doing this, he said, and hold promise for treating diseases including Alzheimer’s.
A number of psychoactive drugs have now received the FDA’s “breakthrough therapy” designation, which expedites development and review of drugs with the potential to treat serious conditions.
But standard clinical trials, in which one group of patients is given the drug and a control group is given a placebo, have proven problematic, for the simple reason that people have no trouble determining whether they’ve gotten the real thing.
The final clinical trial for Lykos’ MDMA treatment showed that 71% of participants no longer met the criteria for PTSD after 18 weeks of taking the drug versus 48% in the control group.
A March report by the Institute for Clinical and Economic Review, an independent research group, questioned the company’s clinical trial results and challenged the objectivity of MDMA advocates who participated in the study as both patients and therapists. The institute also questioned the drug’s cost-effectiveness, which insurers factor into coverage decisions.
Lykos, a public benefit company, was formed in 2014 as an offshoot of the Multidisciplinary Association for Psychedelic Studies, a nonprofit that has invested more than $150 million into psychedelic research and advocacy.
The company said its researchers developed their studies in partnership with the FDA and used independent raters to ensure the reliability and validity of the results.
“We stand behind the design and results of our clinical trials,” a Lykos spokesperson said in an email.
There are other hazards too. Psychoactive substances can put patients in vulnerable states, making them potential victims for financial exploitation or other types of abuse. In Lykos’ second clinical trial, two therapists were found to have spooned, cuddled, blindfolded, and pinned down a female patient who was in distress.
The substances can also cause shallow breathing, heart issues, and hyperthermia.
To mitigate risks, the FDA can put restrictions on how drugs are administered.
“These are incredibly potent molecules and having them available in vending machines is probably a bad idea,” said Hayim Raclaw of Negev Capital, a venture capital fund focused on psychedelic drug development.
But if the protocols are too stringent, access is likely to be limited.
Rachel del Dosso, a trauma therapist in the greater Los Angeles area who offers ketamine-assisted therapy, said she’s been following the research on drugs like MDMA and psilocybin and is excited for their therapeutic potential but has reservations about the practicalities of treatment.
“As a therapist in clinical practice, I’ve been thinking through how could I make that accessible,” she said. “Because it would cost a lot for [patients] to have me with them for the whole thing.”
Del Dosso said a group therapy model, which is sometimes used in ketamine therapy, could help scale the adoption of other psychoactive treatments, too.
Artificial Intelligence and Analogs
Researchers expect plenty of new discoveries in the field. One of the companies Negev has invested in, Mindstate Design Labs, uses artificial intelligence to analyze “trip reports,” or self-reported drug experiences, to identify potentially therapeutic molecules. Mindstate has asked the FDA to green-light a clinical trial of the first molecule identified through this method, 5-MeO-MiPT, also known as moxy.
AlphaFold, an AI program developed by Google’s DeepMind, has identified thousands of potential psychedelic molecules.
There’s also a lot of work going into so-called analog compounds, which have the therapeutic effects of hallucinogens but without the hallucinations. The maker of a psilocybin analog announced in March that the FDA had granted it breakthrough therapy status.
“If you can harness the neuroplasticity-promoting properties of LSD while also creating an antipsychotic version of it, then that can be pretty powerful,” Olson said.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Coca-Cola vs Diet Coke – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Coca-Cola to Diet Coke, we picked the Diet Coke.
Why?
While the Diet Coke is bad, the Coca-Cola has mostly the same problems plus sugar.
The sugar in a can of Coca-Cola is 39g high-fructose corn syrup (the worst kind of sugar yet known to humanity), and of course it’s being delivered in liquid form (the most bioavailable way to get, which in this case, is bad).
To put those 39g into perspective, the daily recommended amount of sugar is 36g for men or 25g for women, according to the AHA.
The sweetener in Diet Coke is aspartame, which has had a lot of health risk accusations made against it, most of which have not stood up to scrutiny, and the main risk it does have is “it mimics sugar too well” and it can increase cravings for sweetness, and therefore higher consumption of sugars in other products. For this reason, the World Health Organization has recommended to simply reduce sugar intake without looking to artificial sweeteners to help.
Nevertheless, aspartame has been found safe (in moderate doses; the upper tolerance level would equate to more than 20 cans of diet coke per day) by food safety agencies ranging from the FDA to the EFSA, based on a large body of science.
Other problems that Diet Coke has are present in Coca-Cola too, such as its acidic nature (bad for tooth enamel) and gassy nature (messes with leptin/ghrelin balance).
Summary: the Diet Coke is relatively less unhealthy, but is still bad in numerous ways, and remains best avoided.
Read more:
Share This Post
-
Survival of the Prettiest – by Dr. Nancy Etcoff
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Beauty is in the eye of the beholder, right? And what does it matter, in this modern world, especially if we are already in a happy stable partnership?
The science of it, as it turns out, is less poetic. Not only is evolutionary psychology still the foundation of our perception of human beauty (yes, even if we have zero possibility of further procreation personally), but also, its effects are far, far wider than partner selection.
From how nice people are to you, to how much they trust you, to how easily they will forgive a (real or perceived) misdeed, to what kind of medical care you get (or don’t), your looks shape your experiences.
In this very easy-reading work that nevertheless contains very many references, Dr. Etcoff explores the science of beauty. Not just what traits are attractive and why, but also, what they will do for (or against) us—in concrete terms, with numbers.
Bottom line: if you’d like to better understand the subconscious biases held by yourself and others, this book is a top-tier primer.
Share This Post
-
Unwell Women – by Dr. Elinor Cleghorn
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For a demographic that makes up a little over half of the world’s population, women are paradoxically marginalized in healthcare. And in other ways too, but this book is about health.
Dr. Cleghorn had to fight for seven (!) years to get her own lupus condition recognized as such, and continues to have to fight for it to be taken seriously on an ongoing basis. And yet, 95% of the book is not about her and her experiences, but rather, the bigger picture.
The book is divided into sections, by period in history. From Hippocrates to the modern day, Dr. Cleghorn gives us a well-researched, incredibly well-referenced overview of the marginalization of women’s health. Far from being a dry history book in the early parts though, it’s fascinating and engaging throughout.
The modern day sections are part shining a light into dark areas, part practical information-and-advice “did you know this happens, and you can do this about it”, and part emphatic call-to-action to demand better.
Bottom line: this book is in this reviewer’s “top 5 books read this year”, and we highly recommend it to you.
Share This Post
Related Posts
-
5 Golden Rules To Lose Belly Fat
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our belly is often the first place we gain fat and the last to lose it—due to hormonal changes, poor blood flow, and fat cell types. This also means that weight loss efforts can result in it looking worse before it looks better, as we lose weight from elsewhere around it. But, there is a way forwards:
What to do about it
Cori Lefkowith, of “Redefining Strength” and “Strength At Any Age” fame, advise that we follow the following “5 golden rules”:
- Mindset: avoid “All or Nothing” thinking; focus on small, sustainable changes and consistent habits.
- Macros: prioritize protein (40%+ of calories), balance fats and carbs for hormonal health, and avoid extreme calorie deficits (your body will try to save you from starvation by slowing your metabolism to conserve energy, and storing fat).
- Nutrition quality: focus on whole, nutrient-dense foods for better satiety, gut health, and energy. Get plenty of fiber and water; your body still needs those too.
- Muscle building: strength training preserves muscle, boosts metabolism, and improves body composition—don’t ditch your strength training for cardio; it won’t help and that swap would hinder..
- Daily walks: 15–20 minutes of walking after dinner aids digestion, and reduces stress (remember: stress invites your body to store extra fat, especially at the belly). It also incidentally burns calories without stressing the body, but honestly, it’s really not very many calories, so that’s not the main reason to do it.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Visceral Belly Fat & How To Lose It ← this is not the same thing as subcutaneous fat; the remedy is partly the same though, and it’s important to do both if you’re carrying excess weight both on your belly and in your viscera, if you want to reduce your overall waist size.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
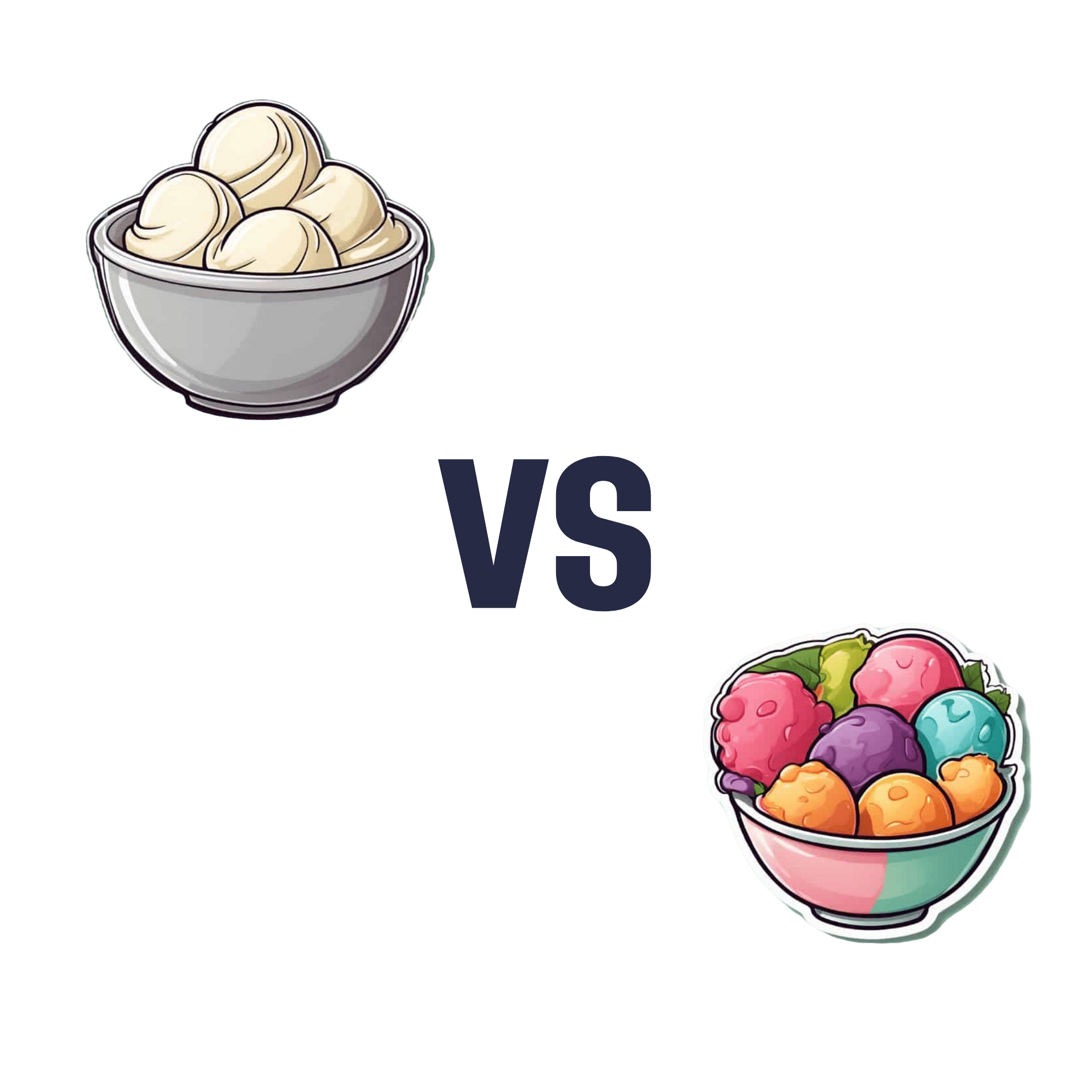
Ice Cream vs Fruit Sorbet – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing ice cream to fruit sorbet, we picked the ice cream.
Why?
Well, neither are great!
But the deciding factor is simple: ice cream has more nutrients to go with its sugar.
While “fruit is good” is a very reliable truism in and of itself, sorbet tends to be made with fruit juice (or at best, purée, which for these purposes is more or less the same) and sugar. The small vitamin content is nowhere near enough to make up for this. The fiber having been removed by juicing or puréeing, the fruit juice with added sugar is basically shooting glucose and fructose into your veins while doing little else.
Fruit juice (even freshly-pressed) is nowhere near in the same league of healthiness as actual fruit!
See also: Which Sugars Are Healthier, And Which Are Just The Same?
Ice cream, meanwhile, is also not exactly a health food. But it has at least some minerals worth speaking of (mostly: calcium, potassium, phosphorus), and some fat that a) can be used b) helps slightly slow the absorption of the sugars.
In short: please do not consider either of these things to be a health food. But if you’re going to choose one or the other (and are not lactose-intolerant), then ice cream has some small positives to go with its negatives.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is It Dementia?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Spot The Signs (Because None Of Us Are Immune)
Dementia affects increasingly many people, and unlike a lot of diseases, it disproportionately affects people in wealthy industrialized nations.
There are two main reasons for this:
- Longevity (in poorer countries, more people die of other things sooner; can’t get age-related cognitive decline if you don’t age)
- Lifestyle (in the age of convenience, it has never been easier to live an unhealthy lifestyle)
The former is obviously no bad thing for those of us lucky enough to be in wealthier countries (though even in such places, good healthcare access is of course sadly not a given for all).
The latter, however, is less systemic and more epidemic. But it does cut both ways:
- An unhealthy lifestyle is much easier here, yes
- A healthier lifestyle is much easier here, too!
This then comes down to two factors in turn:
- Information: knowing about dementia, what things lead to it, what to look out for, what to do
- Motivation: priorities, and how much attention we choose to give this matter
So, let’s get some information, and then give it our attention!
More than just memory
It’s easy to focus on memory loss, but the four key disabilities directly caused by dementia (each person may not get all four), can be remembered by the mnemonic: “AAAA!”
No, somebody didn’t just murder your writer. It’s:
- Amnesia: memory loss, in one or more of its many forms
- e.g. short term memory loss, and/or inability to make new memories
- Aphasia: loss of ability to express oneself, and/or understand what is expressed
- e.g. “More people have been to Berlin than I have”
- Or even less communication-friendly, Broca’s (Expressive) Aphasia and Wernicke’s (Receptive) Aphasia
- Apraxia: loss of ability to do things, through no obvious physical disability
- e.g. staring at the bathroom mirror wondering how to brush one’s teeth
- Agnosia: loss of ability to recognize things
- e.g. prosopagnosia, also called face-blindness.
If any of those seem worryingly familiar, be aware that while yes, it could be a red flag, what’s most important is patterns of these things.
Another difference between having a momentary brainlapse and having dementia might be, for example, the difference between forgetting your keys, and forgetting what keys do or how to use one.
That said, some are neurological deficits that may show up quite unrelated to dementia, including most of those given as examples above. So if you have just one, then that’s probably worthy of note, but probably not dementia.
Writer’s anecdote: I have had prosopagnosia all my life. To give an example of what that is like and how it’s rather more than just “bad with faces”…
Recently I saw my neighbor, and I could tell something was wrong with her face, but I couldn’t put my finger on what it was. Then some moments later, I realized I had mistaken her hat for her face. It was a large beanie with a panda design on it, and that was facelike enough for me to find myself looking at the wrong face.
Subjective memory matters as much as objective
Objective memory tests are great indicators of potential cognitive decline (or improvement!), but even a subjective idea of having memory problems, that one’s memory is “not as good as it used to be”, can be an important indicator too:
Subjective memory may be marker for cognitive decline
And more recently:
If your memory feels like it’s not what it once was, it could point to a future dementia risk
If you’d like an objective test of memory and other cognitive impairments, here’s the industry’s gold standard test (it’s free):
SAGE: A Test to Detect Signs of Alzheimer’s and Dementia
(The Self-Administered Gerocognitive Exam (SAGE) is designed to detect early signs of cognitive, memory or thinking impairments)
There are things that can look like dementia that aren’t
A person with dementia may be unable to recognize their partner, but hey, this writer knows that feeling very well too. So what sets things apart?
More than we have room for today, but here’s a good overview:
What are the early signs of dementia, and how does it differ from normal aging?
Want to read more?
You might like our previous article more specifically about reducing Alzheimer’s risk:
Reducing Alzheimer’s Risk Early!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: