Perfectionism, And How To Make Yours Work For You
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Harness The Power Of Your Perfectionism
A lot of people see perfectionism as a problem—and it can be that!
We can use perfectionism as a would-be shield against our fear of failure, by putting things off until we’re better prepared (repeat forever, or at least until the deadliniest deadline that ever deadlined), or do things but really struggle to draw a line under them and check them off as “done” because we keep tweaking and improving and improving… With diminishing returns (forever). So, that’s not helpful.
But, if we’re mindful, we can also leverage our perfectionism to our benefit.
Great! How?
First we need to be able to discern the ways in which perfectionism can be bad or good for us. Or as it’s called in psychology, ways in which our perfectionism can be maladaptive or adaptive.
- Maladaptive: describing a behavioral adaptation to our environment—specifically, a reactive behavioral adaptation that is unhealthy and really is not a solution to the problem at hand
- Adaptive: describing a behavioral adaptation to our environment—specifically, a responsive behavioral adaptation that is healthy and helps us to thrive
So in the case of perfectionism, one example for each might be:
- Maladaptive: never taking up that new hobby, because you’re just going to suck at it anyway, and what’s the point if you’re not going to excel? You’re a perfectionist, and you don’t settle for anything less than excellence.
- Adaptive: researching the new hobby, learning the basics, and recognizing that even if the results are not immediately perfect, the learning process can be… Yes, even with mistakes along the way, for they too are part of learning! You’re a perfectionist, and you’re going to be the best possible student of your new hobby.
Did you catch the key there?
When it comes to approaching things we do in life—either because we want to or because we must—there are two kinds of mindset: goal-oriented, and task-oriented.
Broadly speaking, each has their merits, and as a general topic, it’s beyond the scope of today’s main feature. Here we’re looking at it in the context of perfectionism, and in that frame, there’s a clear qualitative difference:
- The goal-oriented perfectionist will be frustrated to the point of torment, at not immediately attaining the goal. Everything short of that will be a means to an end, at best. Not fun.
- The task-oriented perfectionist will take joy in going about the task in the best way possible, and optimizing their process as they go. The journey itself will be rewarding and a tangible product of their consistent perfectionism.
The good news is: you get to choose! You’re not stuck in a box.
If you’re thinking “I’m a perfectionist and I’m generally a goal-oriented person”, that’s fine. You’re just going to need to reframe your goals.
- Instead of: my goal is to be fluent in Arabic
- …so you never speak it, because to err is human, all too human, and you’re a perfectionist, so you don’t want that!
- Let’s try: my goal is to study Arabic for at least 15 minutes per day, every day, without fail, covering at least some new material each time, no matter how small the increase
- …and then you go and throw yourself into conversation way out of your depth, make mistakes, and get corrections, because that’s how you learn, and you’re a perfectionist, so you want that!
This goes for any field of expertise, of course.
- If you want to play the violin solo in Carnegie Hall, you have to pick up your violin and practice each day.
- If you want to be a world-renowned pastry chef, you have to make a consistent habit of baking.
- If you want to write a bestselling book, you have to show up at your keyboard.
Be perfect all you want, but be the perfect student.
And as your skills grow, maybe you’ll upgrade that to also being the perfect practitioner, and perhaps later still, the perfect teacher.
But just remember:
Perfection comes not from the end goal (that would be backwards thinking!) but from the process (which includes mistakes; they’re an important part of learning; embrace them and grow!), so perfect that first.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Every Body Should Know This – by Dr. Federica Amati
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is very much a primer on how to eat healthily. The science is high-quality (the author is the head nutritionist at ZOE) and well-explained, and the advice is reasonable.
Limitations: this book is not very deep, which we might expect from a book with this title. So, if you’ve been a long-time 10almonds reader, you might not learn a lot here, and this book might make a better gift for someone else.
In particular, the book may be well-suited for someone who is thinking of having children soon, as there is an unusual amount of focus on fertility and young motherhood—perhaps because the author herself has young children and so was preoccupied with this when writing. For those of us who are definitely not having any more children, the focus on young motherhood is a little superfluous.
The writing style is very readable pop-science, and nobody who is able to read English is likely to struggle with this one. It’s also quite conversational in parts, as the author discusses her own experiences with implementing the science at hand.
Bottom line: if you want a good, solid, primer of how to eat well for a lifetime of health, especially if you are (or are thinking of becoming) a young mother, then this is a very good book. Otherwise, it’s probably a better to give it as a gift.
Click here to check out Every Body Should Know This, and know the things!
Share This Post
-
Robert F. Kennedy Jr says vitamin A protects you from deadly measles. Here’s what the study he cites actually says
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Robert F. Kennedy Jr, who oversees the health of more than 340 million Americans, says vitamin A can prevent the worst effects of measles rather than urging more people to get vaccinated.
In an opinion piece for Fox News, the US health secretary said he was “deeply concerned” about the current measles outbreak in Texas. However, he said the decision to vaccinate was a “personal one” and something for parents to discuss with their health-care provider.
Kennedy mentioned updated advice from the Centers for Disease Control (CDC) to treat measles with vitamin A. He also cited a study he said shows vitamin A can reduce the risk of dying from measles.
Here’s what the vitamin A study actually says and why public health officials are so concerned about Kennedy’s latest statement.
RobsPhoto/Shutterstock Why is a measles outbreak so worrying?
Measles is a highly contagious disease caused by a virus. It spreads easily including when an infected person breathes, coughs or sneezes.
Measles initially infects the respiratory tract and then the virus spreads throughout the body. Symptoms include a high fever, cough, red eyes, runny nose and a rash all over the body.
Measles can also be severe, can cause complications including blindness and swelling of the brain, and can be fatal. Measles can affect anyone but is most common in children.
The Texan health department has confirmed 150-plus cases of measles and one death of an unvaccinated child during the current outbreak. While this is by far the largest measles outbreak in the US in 2025, the CDC has reported smaller outbreaks in several other states so far this year.
Why vitamin A?
Vitamin A is essential for our overall health. It has many roles in the body, from supporting our growth and reproduction, to making sure we have healthy vision, skin and immune function.
Foods rich in vitamin A or related molecules include orange, yellow and red coloured fruits and vegetables, green leafy vegetables, as well as dairy, egg, fish and meat. You can take it as a supplement.
Vitamin A can also be used therapeutically. In other words, doctors may prescribe vitamin A to treat a deficiency. Vitamin A deficiency has long been associated with more severe cases of infectious disease, including measles. Vitamin A boosts immune cells and strengthens the respiratory tract lining, which is the body’s first defence against infections.
Because of this, the CDC has recently said vitamin A can also be prescribed as part of treatment for children with severe measles – such as those in hospital – under doctor supervision.
One key message from the CDC’s advice is that people are already sick enough with measles to be in hospital. They’re not taking vitamin A to prevent catching measles in the first place.
The other key message is vitamin A is taken under medical supervision, under specific circumstances, where patients can be closely monitored to prevent toxicity from high doses.
Vitamin A toxicity can cause birth defects and increase the risk of fractures in elderly people. Vitamin A and beta-carotene (which the body turns into vitamin A) from supplements may also increase your risk of cancer, especially if you smoke.
Taking too much vitamin A can lead to toxicity and cause birth defects. ChameleonsEye/Shutterstock How about the study Kennedy cites?
Kennedy cites and links to a 2010 study, a type known as a systematic review and meta-analysis. Researchers reviewed and analysed existing studies, which included ones that looked at the effectiveness of vitamin A in preventing measles deaths.
They found three studies that looked at vitamin A treatment by specific dose. There were different doses depending on the age of the children, measured in IU (international units). Having two doses of vitamin A (200,000IU for children over one year of age or 100,000IU for infants below one year) reduced mortality by 62% compared to children who did not have vitamin A.
The 2010 study did not show vitamin A reduced your risk of getting measles from another infected person. To my knowledge no study has shown this.
To be fair, Kennedy did not say that vitamin A stops you from catching measles from another infected person. Instead, he used the following vague statement:
Studies have found that vitamin A can dramatically reduce measles mortality.
It’s easy to see how a reader could misinterpret this as “take vitamin A if you want to avoid dying from measles”.
We know what works – vaccines
The World Health Organization recommends all children receive two doses of measles vaccine.
The CDC states two doses of the measles vaccine (measles-mumps-rubella or MMR vaccine) is 97% effective against getting measles. This means out of every 100 people who are vaccinated only three will get it, and this will be a milder form.
But these facts were missing from Kennedy’s statement. Should we be surprised? Kennedy is well known for his vaccine sceptism and for undermining vaccination efforts, including for the measles vaccine.
As Sue Kressly, president of the American Academy of Pediatrics, told the Washington Post:
relying on vitamin A instead of the vaccine is not only dangerous and ineffective […] it puts children at serious risk.
Evangeline Mantzioris, Program Director of Nutrition and Food Sciences, Accredited Practising Dietitian, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Children can be more vulnerable in the heat. Here’s how to protect them this summer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Extreme heat is increasingly common in Australia and around the world and besides making us uncomfortable, it can harm our health. For example, exposure to extreme heat can exacerbate existing medical conditions, or cause problems such as heat stroke.
Due to a combination of physiology and behaviour, children are potentially more vulnerable to severe heat-related illness such as heat stroke or heat exhaustion.
But these are not the only heat-related health issues children might experience on a very hot day. In a new study, we looked at emergency department (ED) visits and unplanned hospital admissions among children in New South Wales on heatwave days.
We found a significant increase in children attending hospital compared to milder days – with a range of health issues.
maxim ibragimov/Shutterstock Why are children more vulnerable in the heat?
Sweating is the main way we lose heat from our bodies and cool down.
Children have a greater skin surface area to body mass ratio, which can be an advantage for sweating – they can lose more heat through evaporation for a given body mass. But this also means children can lose fluids and electrolytes faster through sweating, theoretically making them more susceptible to dehydration.
Meanwhile, younger children, particularly babies, can’t sweat as much as older children and adults. This means they can’t cool down as effectively.
Children in general also tend to engage in more outdoor physical activity, which might see them more exposed to very hot temperatures.
Further, children may be less in-tune to the signals their body is giving them that they’re overheating, such as excessive sweating or red skin. So they might not stop and cool down when they need to. Young children especially may not recognise the early signs of heat stress or be able to express discomfort.
Children may not easily be able to communicate that they’re hot and bothered. christinarosepix/Shutterstock Our study
We wanted to examine children’s exposure to extreme heat stress and the associated risks to their health.
We measured extreme heat as “heatwave days”, at least two consecutive days with a daily maximum temperature above the 95th percentile for the relevant area on a universal thermal climate index. This ranged from 27°C to 45°C depending on the area.
We assessed health outcomes by looking at ED visits and unplanned hospital admissions among children aged 0–18 years from NSW between 2000 and 2020. This totalled around 8.2 million ED visits and 1.4 million hospital admissions.
We found hospital admissions for heat-related illness were 104% more likely on heatwave days compared to non-heatwave days, and ED visits were 78% more likely. Heat-related illness includes a spectrum of disorders from minor conditions such as dehydration to life-threatening conditions such as heat stroke.
But heat-related illness wasn’t the only condition that increased on heatwave days. There was also an increase in childhood infections, particularly infectious enteritis possibly related to food poisoning (up 6% for ED visits and 17% for hospital admissions), ear infections (up 30% for ED visits and 3% for hospital admissions), and skin and soft tissue infections (up 6% for ED visits and 4% for hospital admissions).
Kids can be more vulnerable in the heat because of their behaviour and physiology. K-FK/Shutterstock We know many infectious diseases are highly seasonal. Some, like the flu, peak in winter. But heat and humidity increase the risk of certain infections caused by bacterial, viral and fungal pathogens.
For example, warmer weather and higher humidity can increase the survival of bacteria, such as Salmonella, on foods, which increases the risk of food poisoning.
Hot weather can also increase the risk of ear infections. Children may be at greater risk during hot weather because they often swim or play at the beach or pool. Water can stay in the ear after swimming and a moist environment in the ear canal can cause growth of pathogens leading to ear infections.
Which children are most vulnerable?
During heatwaves, we found infants aged under one were at increased risk of ED visits and hospital admission for any reason compared to older children. This is not surprising, because babies can’t regulate their body temperature effectively and are reliant on their caregivers to keep them cool.
Our study also found children from the most disadvantaged areas were more vulnerable to heat-related illness on heatwave days. Although we don’t know exactly why, we hypothesised families from poorer areas might have limited access to air-conditioning and could be more likely to live in hotter neighbourhoods.
Keeping kids cool: tips for parents
The highest levels of heat exposure on hot days for young children is usually when they’re taken outside in prams and strollers. To protect their children from direct sunlight, parents often instinctively cover their stroller with a cloth such as a muslin.
However, a recent study from our group showed this actually increases temperatures inside a stroller to as much as 3–4˚C higher than outside.
But if the cloth is wet with water, and a small fan is used to circulate the air close to the child, stroller temperatures can be 4–5˚C lower than outside. Wetting the cloth every 15–20 minutes (for example, with a spray bottle) maintains the cooling effect.
When young children are not in a stroller, and for older children, there are a few things to consider to keep them cool and safe.
Remember temperatures reported on weather forecasts are measured in the shade, and temperatures in the sun can be up to 15˚C higher. So sticking to the shade as much as possible is important.
Exercise generates heat inside the body, so activities should be shortened, or rescheduled to cooler times of the day.
Sunscreen and hats are important when outdoors, but neither are especially effective for keeping cool. Spraying water on the child’s skin – not just the face but arms, legs and even the torso if possible – can help. Wetting their hats is another idea.
Proper hydration on hot days is also essential. Regular water breaks, including offering water before, during and after activity, is important. Offering foods with high water content such as watermelon and orange can help with hydration too.
Wen-Qiang He, Research Fellow in Biostatistics and Epidemiology, Faculty of Medicine and Health, University of Sydney; James Smallcombe, Post-doctoral Research Associate, Faculty of Medicine and Health, University of Sydney; Natasha Nassar, Professor of Paediatric and Perinatal Epidemiology and Chair in Translational Childhood Medicine, University of Sydney, and Ollie Jay, Professor of Heat & Health; Director of Heat & Health Research Incubator; Director of Thermal Ergonomics Laboratory, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Heal Your Nervous System – by Dr. Linnea Passaler
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book focuses on the oft-overlooked connection between nervous system dysregulation (i.e. sympathetic nervous system dominance, keeping the brain in “may have to fight for my life at any moment” mode) and the many symptoms—mental and physical—that can arise as a result.
While there is a lot of theory explained in here, there’s practicality too, providing the reader with tools to assess our own levels of nervous system dysregulation and what factors affect that.
In particular in that category, a lot of value is delivered in terms of practical guidance on avoiding common pitfalls in the healing journey. Dr. Passaler discusses the four biggest mistakes people make when attempting to heal, and gives clear strategies to sidestep each of them, with exercises to do and habits to implement.
Another thing that sets this book apart from many of its genre is her emphasis on the importance of sequencing healing practices in the right order. By offering a structured approach, the book helps us implement healing practices without getting overwhelmed or hitting the proverbial brick wall and getting frustrated, which makes a big difference.
The style is easy-to-understand pop-science, albeit with a reassuring 20 pages of references at the back.
Bottom line: if you feel like “peace of mind” is something that’s always just out of reach, this book can help you to get where you need to be, physically as well as mentally.
Click here to check out Heal Your Nervous System, and get things into much better order!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
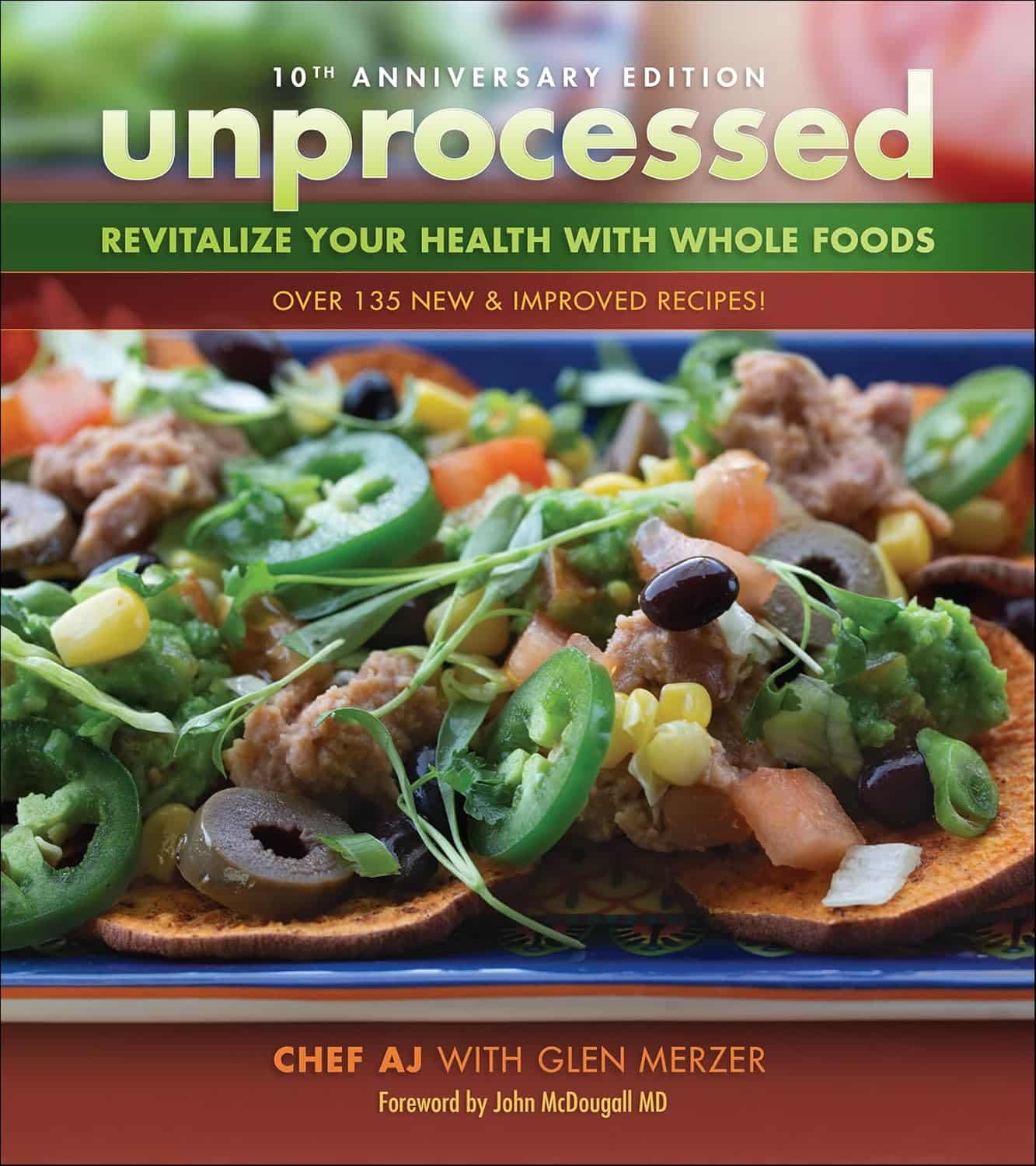
Unprocessed 10th Anniversary Edition – by Abbie Jay
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The main premise of this book is cooking…
- With nutritious whole foods
- Without salt, oil, sugar (“SOS”)
It additionally does it without animal products and without gluten, and (per “nutritious whole foods”), and, as the title suggests, avoiding anything that’s more than very minimally processed. Remember, for example, that if something is fermented, then that fermentation is a process, so the food has been processed—just, minimally.
This is a revised edition, and it’s been adjusted to, for example, strip some of the previous “no salt” low-sodium options (such as tamari with 233mg/tsp sodium, compared to salt’s 2,300mg/tsp sodium).
You may be wondering: what’s left? Tasty, well-seasoned, plant-based food, that leans towards the “comfort food” culinary niche.
Enough to sate the author, after her own battles with anorexia and obesity (in that order) and finally, after various hospital trips, getting her diet where it needed to be for the healthy lifestyle that she lives now, while still getting to eat such dishes as “Chef AJ’s Disappearing Lasagna” and peanut butter fudge truffles and 151 more.
Bottom line: if you want whole-food plant-based comfort-food cooking that’s healthy in general and especially heart-healthy, this book has plenty of that.
Click here to check out Unprocessed: 10th Anniversary Edition, and… Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Protein: How Much Do We Need, Really?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mythbusting Protein!
Yesterday, we asked you for your policy on protein consumption. The distribution of responses was as follows:
- A marginal majority (about 55%) voted for “Protein is very important, but we can eat too much of it”
- A large minority (about 35%) voted for “We need lots of protein; the more, the better!”
- A handful (about 4%) voted for “We should go as light on protein as possible”
- A handful (6%) voted for “If we don’t eat protein, our body will create it from other foods”
So, what does the science say?
If we don’t eat protein, our body will create it from other foods: True or False?
Contingently True on an absurd technicality, but for all practical purposes False.
Our body requires 20 amino acids (the building blocks of protein), 9 of which it can’t synthesize and absolutely must get from food. Normally, we get those amino acids from protein in our diet, and we can also supplement them by buying amino acid supplements.
Specifically, we require (per kg of bodyweight) a daily average of:
- Histidine: 10 mg
- Isoleucine: 20 mg
- Leucine: 39 mg
- Lysine: 30 mg
- Methionine: 10.4 mg
- Phenylalanine*: 25 mg
- Threonine: 15 mg
- Tryptophan: 4 mg
- Valine: 26 mg
*combined with the non-essential amino acid tyrosine
Source: Protein and Amino Acid Requirements In Human Nutrition: WHO Technical Report
However, to get the requisite amino acid amounts, without consuming actual protein, would require gargantuan amounts of supplementation (bearing in mind bioavailability will never be 100%, so you’ll always need to take more than it seems), using supplements that will have been made by breaking down proteins anyway.
So unless you live in a laboratory and have access to endless amounts of all of the required amino acids (you can’t miss even one; you will die), and are willing to do that for the sake of proving a point, then you do really need to eat protein.
Your body cannot, for example, simply break down sugar and use it to make the protein you need.
On another technical note… Do bear in mind that many foods that we don’t necessarily think of as being sources of protein, are sources of protein.
Grains and grain products, for example, all contain protein; we just don’t think of them as that because their macronutritional profile is heavily weighted towards carbohydrates.
For that matter, even celery contains protein. How much, you may ask? Almost none! But if something has DNA, it has protein. Which means all plants and animals (at least in their unrefined forms).
So again, to even try to live without protein would very much require living in a laboratory.
We can eat too much protein: True or False?
True. First on an easy technicality; anything in excess is toxic. Even water, or oxygen. But also, in practical terms, there is such a thing as too much protein. The bar is quite high, though:
❝Based on short-term nitrogen balance studies, the Recommended Dietary Allowance of protein for a healthy adult with minimal physical activity is currently 0.8 g protein per kg bodyweight per day❞
❝To meet the functional needs such as promoting skeletal-muscle protein accretion and physical strength, dietary intake of 1.0, 1.3, and 1.6 g protein per kg bodyweight per day is recommended for individuals with minimal, moderate, and intense physical activity, respectively❞
❝Long-term consumption of protein at 2 g per kg bodyweight per day is safe for healthy adults, and the tolerable upper limit is 3.5 g per kg bodyweight per day for well-adapted subjects❞
❝Chronic high protein intake (>2 g per kg bodyweight per day for adults) may result in digestive, renal, and vascular abnormalities and should be avoided❞
Source: Dietary protein intake and human health
To put this into perspective, if you weigh about 160lbs (about 72kg), this would mean eating more than 144g protein per day, which grabbing a calculator means about 560g of lean beef, or 20oz, or 1¼lb.
If you’re eating quarter-pounder burgers though, that’s not usually so lean, so you’d need to eat more than nine quarter-pounder burgers per day to get too much protein.
High protein intake damages the kidneys: True or False?
True if you have kidney damage already; False if you are healthy. See for example:
- Effects of dietary protein restriction on the progression of advanced renal disease in the modification of diet in renal disease study
- A high protein diet has no harmful effects: a one-year crossover study in healthy male athletes
High protein intake increases cancer risk: True or False?
True or False depending on the source of the protein, so functionally false:
- Eating protein from red meat sources has been associated with higher risk for many cancers
- Eating protein from other sources has been associated with lower risk for many cancers
Source: Red Meat Consumption and Mortality Results From 2 Prospective Cohort Studies
High protein intake increase risk of heart disease: True or False?
True or False depending on the source of the protein, so, functionally false:
- Eating protein from red meat sources has been associated with higher risk of heart disease
- Eating protein from other sources has been associated with lower risk of heart disease
Source: Major Dietary Protein Sources and Risk of Coronary Heart Disease in Women
In summary…
Getting a good amount of good quality protein is important to health.
One can get too much, but one would have to go to extremes to do so.
The source of protein matters:
- Red meat is associated with many health risks, but that’s not necessarily the protein’s fault.
- Getting plenty of protein from (ideally: unprocessed) sources such as poultry, fish, and/or plants, is critical to good health.
- Consuming “whole proteins” (that contain all 9 amino acids that we can’t synthesize) are best.
Learn more: Complete proteins vs. incomplete proteins (explanation and examples)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: