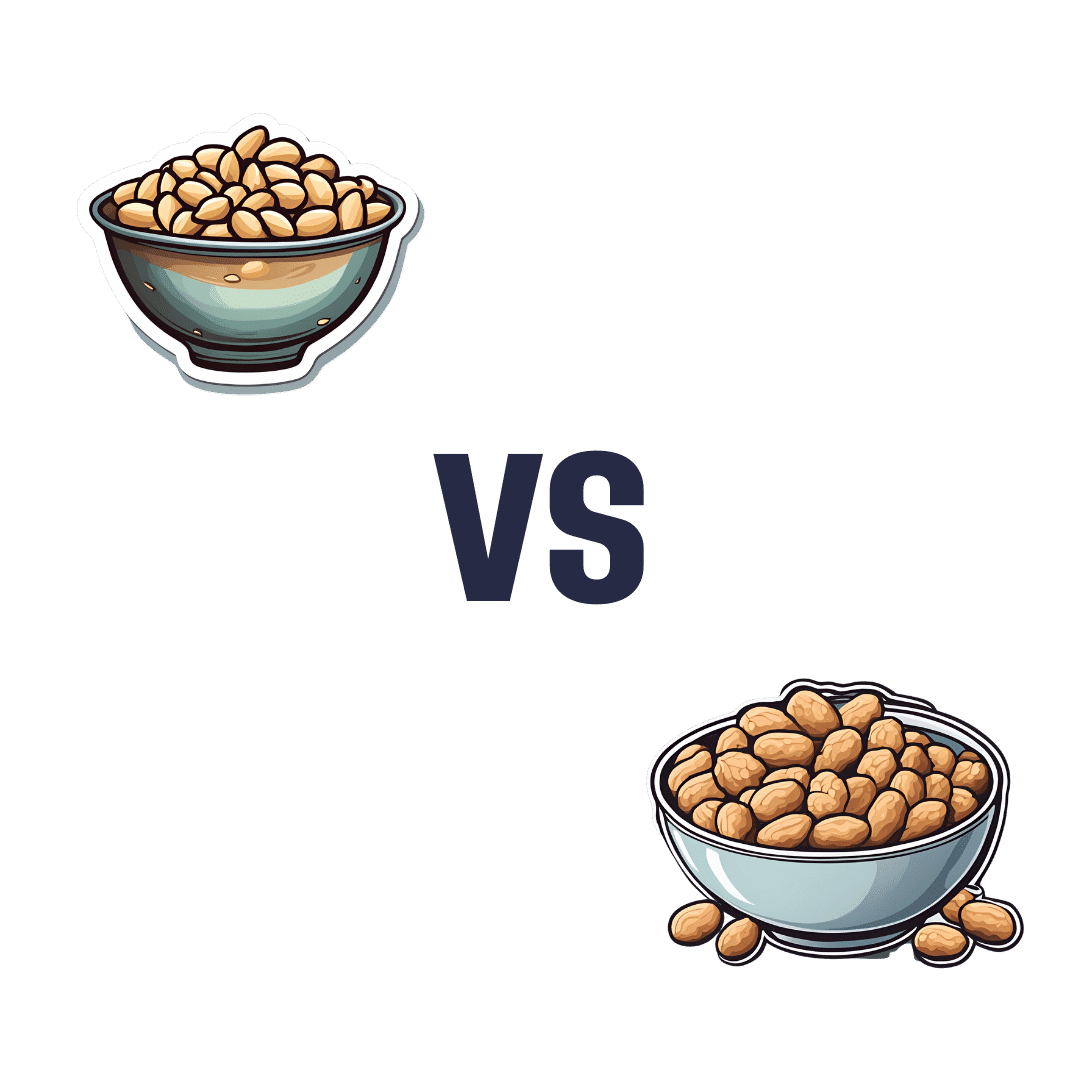
Pine Nuts vs Peanuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pine nuts to peanuts, we picked the pine nuts.
Why?
An argument could be made for either, honestly, as it depends on what we prioritize the most. These are both very high-calorie foods, and/but are far from empty calories, as they both contain main nutrients. Obviously, if you are allergic to nuts, this one is just not a comparison for you, sorry.
Looking at the macros first, peanuts are higher in protein, carbs, and fiber, while pine nuts are higher in fats—though the fats are healthy, being mostly polyunsaturated, with about a third of the total fats monounsaturated, and a low amount of saturated fat (peanuts have nearly 2x the saturated fat). On balance, we’ll call the macros category a moderate win for peanuts, though.
In terms of vitamins, peanuts have more of vitamins B1, B3, B5, B6, and B9, while pine nuts have more of vitamins A, B2, C, E, K, and choline. All in all, a marginal win for pine nuts.
In the category of minerals, peanuts have more calcium and selenium, while pine nuts have more copper, iron, magnesium, manganese, phosphorus, and zinc. An easy win for pine nuts, even before we take into account that peanuts have nearly 10x as much sodium. And yes, we are talking about the raw nuts, not nuts that have been roasted and salted.
Adding up the categories gives a win for pine nuts—but if you have certain particular priorities, you might still prefer peanuts for the areas in which peanuts are stronger.
Of course, the best solution is to enjoy both!
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Our ‘food environments’ affect what we eat. Here’s how you can change yours to support healthier eating
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In January, many people are setting new year’s resolutions around healthy eating. Achieving these is often challenging – it can be difficult to change our eating habits. But healthy diets can enhance physical and mental health, so improving what we eat is a worthwhile goal.
One reason it’s difficult to change our eating habits relates to our “food environments”. This term describes:
The collective physical, economic, policy and sociocultural surroundings, opportunities and conditions that influence people’s food and beverage choices and nutritional status.
Our current food environments are designed in ways that often make it easier to choose unhealthy foods than healthy ones. But it’s possible to change certain aspects of our personal food environments, making eating healthier a little easier.
Unhealthy food environments
It’s not difficult to find fast-food restaurants in Australian cities. Meanwhile, there are junk foods at supermarket checkouts, service stations and sporting venues. Takeaway and packaged foods and drinks routinely come in large portion sizes and are often considered tastier than healthy options.
Our food environments also provide us with various prompts to eat unhealthy foods via the media and advertising, alongside health and nutrition claims and appealing marketing images on food packaging.
At the supermarket, unhealthy foods are often promoted through prominent displays and price discounts.
We’re also exposed to various situations in our everyday lives that can make healthy eating challenging. For example, social occasions or work functions might see large amounts of unhealthy food on offer.
Not everyone is affected in the same way
People differ in the degree to which their food consumption is influenced by their food environments.
This can be due to biological factors (for example, genetics and hormones), psychological characteristics (such as decision making processes or personality traits) and prior experiences with food (for example, learned associations between foods and particular situations or emotions).
People who are more susceptible will likely eat more and eat more unhealthy foods than those who are more immune to the effects of food environments and situations.
Those who are more susceptible may pay greater attention to food cues such as advertisements and cooking smells, and feel a stronger desire to eat when exposed to these cues. Meanwhile, they may pay less attention to internal cues signalling hunger and fullness. These differences are due to a combination of biological and psychological characteristics.
These people might also be more likely to experience physiological reactions to food cues including changes in heart rate and increased salivation.
It’s common to eat junk food in front of the TV.
PR Image Factory/ShutterstockOther situational cues can also prompt eating for some people, depending on what they’ve learned about eating. Some of us tend to eat when we’re tired or in a bad mood, having learned over time eating provides comfort in these situations.
Other people will tend to eat in situations such as in the car during the commute home from work (possibly passing multiple fast-food outlets along the way), or at certain times of day such as after dinner, or when others around them are eating, having learned associations between these situations and eating.
Being in front of a TV or other screen can also prompt people to eat, eat unhealthy foods, or eat more than intended.
Making changes
While it’s not possible to change wider food environments or individual characteristics that affect susceptibility to food cues, you can try to tune into how and when you’re affected by food cues. Then you can restructure some aspects of your personal food environments, which can help if you’re working towards healthier eating goals.
Although both meals and snacks are important for overall diet quality, snacks are often unplanned, which means food environments and situations may have a greater impact on what we snack on.
Foods consumed as snacks are often sugary drinks, confectionery, chips and cakes. However, snacks can also be healthy (for example, fruits, nuts and seeds).
Try removing unhealthy foods, particularly packaged snacks, from the house, or not buying them in the first place. This means temptations are removed, which can be especially helpful for those who may be more susceptible to their food environment.
Planning social events around non-food activities can help reduce social influences on eating. For example, why not catch up with friends for a walk instead of lunch at a fast-food restaurant.
Creating certain rules and habits can reduce cues for eating. For example, not eating at your desk, in the car, or in front of the TV will, over time, lessen the effects of these situations as cues for eating.
You could also try keeping a food diary to identify what moods and emotions trigger eating. Once you’ve identified these triggers, develop a plan to help break these habits. Strategies may include doing another activity you enjoy such as going for a short walk or listening to music – anything that can help manage the mood or emotion where you would have typically reached for the fridge.
Write (and stick to) a grocery list and avoid shopping for food when hungry. Plan and prepare meals and snacks ahead of time so eating decisions are made in advance of situations where you might feel especially hungry or tired or be influenced by your food environment.
Georgie Russell, Senior Lecturer, Institute for Physical Activity and Nutrition (IPAN), Deakin University and Rebecca Leech, NHMRC Emerging Leadership Fellow, School of Exercise and Nutrition Sciences, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
STI rates are increasing among midlife and older adults. We need to talk about it
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Globally, the rates of common sexually transmissible infections (STIs) are increasing among people aged over 50. In some cases, rates are rising faster than among younger people.
Recent data from the United States Centers for Disease Control and Prevention shows that, among people aged 55 and older, rates of gonorrhoea and chlamydia, two of the most common STIs, more than doubled between 2012 and 2022.
Australian STI surveillance data has reflected similar trends. Between 2013 and 2022, there was a steady increase in diagnoses of chlamydia, gonorrhoea and syphilis among people aged 40 and older. For example, there were 5,883 notifications of chlamydia in Australians 40 plus in 2013, compared with 10,263 in 2022.
A 2020 study of Australian women also showed that, between 2000 and 2018, there was a sharper increase in STI diagnoses among women aged 55–74 than among younger women.
While the overall rate of common STIs is highest among young adults, the significant increase in STI diagnoses among midlife and older adults suggests we need to pay more attention to sexual health across the life course.
Fit Ztudio/Shutterstock Why are STI rates rising among older adults?
STI rates are increasing globally for all age groups, and an increase among midlife and older people is in line with this trend.
However, increases of STIs among older people are likely due to a combination of changing sex and relationship practices and hidden sexual health needs among this group.
The “boomer” generation came of age in the 60s and 70s. They are the generation of free love and their attitude to sex, even as they age, is quite different to that of generations before them.
Given the median age of divorce in Australia is now over 43, and the internet has ushered in new opportunities for post-separation dating, it’s not surprising that midlife and older adults are exploring new sexual practices or finding multiple sexual partners.
People may start new relationships later in life. Tint Media/Shutterstock It’s also possible midlife and older people have not had exposure to sexual health education in school or do not relate to current safe sex messages, which tend to be directed toward young people. Condoms may therefore seem unnecessary for people who aren’t trying to avoid pregnancy. Older people may also lack confidence negotiating safe sex or accessing STI screening.
Hidden sexual health needs
In contemporary life, the sex lives of older adults are largely invisible. Ageing and older bodies are often associated with loss of power and desirability, reflected in the stereotype of older people as asexual and in derogatory jokes about older people having sex.
With some exceptions, we see few positive representations of older sexual bodies in film or television.
Older people’s sexuality is also largely invisible in public policy. In a review of Australian policy relating to sexual and reproductive health, researchers found midlife and older adults were rarely mentioned.
Sexual health policy generally targets groups with the highest STI rates, which excludes most older people. As midlife and older adults are beyond childbearing years, they also do not feature in reproductive health policy. This means there is a general absence of any policy related to sex or sexual health among midlife or older adults.
Added to this, sexual health policy tends to be focused on risk rather than sexual wellbeing. Sexual wellbeing, including freedom and capacity to pursue pleasurable sexual experiences, is strongly associated with overall health and quality of life for adults of all ages. Including sexual wellbeing as a policy priority would enable a focus on safe and respectful sex and relationships across the adult life course.
Without this priority, we have limited knowledge about what supports sexual wellbeing as people age and limited funding for initiatives to engage with midlife or older adults on these issues.
Midlife and older adults may have limited knowledge about STIs. Southworks/Shutterstock How can we support sexual health and wellbeing for older adults?
Most STIs are easily treatable. Serious complications can occur, however, when STIs are undiagnosed and untreated over a long period. Untreated STIs can also be passed on to others.
Late diagnosis is not uncommon as some STIs can have no symptoms and many people don’t routinely screen for STIs. Older, heterosexual adults are, in general, less likely than other groups to seek regular STI screening.
For midlife or older adults, STIs may also be diagnosed late because some doctors do not initiate testing due to concerns they will cause offence or because they assume STI risk among older people is negligible.
Many doctors are reluctant to discuss sexual health with their older patients unless the patient explicitly raises the topic. However, older people can be embarrassed or feel awkward raising matters of sex.
Resources for health-care providers and patients to facilitate conversations about sexual health and STI screening with older patients would be a good first step.
To address rising rates of STIs among midlife and older adults, we also need to ensure sexual health promotion is targeted toward these age groups and improve accessibility of clinical services.
More broadly, it’s important to consider ways to ensure sexual wellbeing is prioritised in policy and practice related to midlife and older adulthood.
A comprehensive approach to older people’s sexual health, that explicitly places value on the significance of sex and intimacy in people’s lives, will enhance our ability to more effectively respond to sexual health and STI prevention across the life course.
Jennifer Power, Associate Professor and Principal Research Fellow, Australian Research Centre in Sex, Health and Society, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
The #1 Foot Health Secret Everyone Over 50 Should Know
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our favorite over-50s specialist physio Will Harlow is here to keep us on our toes:
Mobility requires mobilization
As we age, our toes are inclined to become stiffer. Stiff toes lead to balance issues and increased risk of falling.
A study cited in the video showed that two weeks of toe mobilization improved foot-ground contact by 30% in older adults, enhancing balance and reducing falls.
Here’s the routine:
- Toe flexion:
- Apply moisturizer or oil to your hands.
- Pull your toes downwards, then let them return their normal position.
- Repeat for one minute per foot.
- Toe extension:
- Rub hands from the heel under the toes.
- Push your toes upwards, then let them return to their normal position.
- Repeat for one minute per foot.
- Foot rotation:
- Hold both sides of your foot and twist it in one direction, then the other.
- This helps loosen foot joints and improve flexibility.
- Perform for one minute in each direction per foot.
For more on each of these plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Steps For Keeping Your Feet A Healthy Foundation
Take care!
Share This Post
- Toe flexion:
Related Posts
-
Alpha, beta, theta: what are brain states and brain waves? And can we control them?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s no shortage of apps and technology that claim to shift the brain into a “theta” state – said to help with relaxation, inward focus and sleep.
But what exactly does it mean to change one’s “mental state”? And is that even possible? For now, the evidence remains murky. But our understanding of the brain is growing exponentially as our methods of investigation improve.
Brain-measuring tech is evolving
Currently, no single approach to imaging or measuring brain activity gives us the whole picture. What we “see” in the brain depends on which tool we use to “look”. There are myriad ways to do this, but each one comes with trade-offs.
We learnt a lot about brain activity in the 1980s thanks to the advent of magnetic resonance imaging (MRI).
Eventually we invented “functional MRI”, which allows us to link brain activity with certain functions or behaviours in real time by measuring the brain’s use of oxygenated blood during a task.
We can also measure electrical activity using EEG (electroencephalography). This can accurately measure the timing of brain waves as they occur, but isn’t very accurate at identifying which specific areas of the brain they occur in.
Alternatively, we can measure the brain’s response to magnetic stimulation. This is very accurate in terms of area and timing, but only as long as it’s close to the surface.
What are brain states?
All of our simple and complex behaviours, as well as our cognition (thoughts) have a foundation in brain activity, or “neural activity”. Neurons – the brain’s nerve cells – communicate by a sequence of electrical impulses and chemical signals called “neurotransmitters”.
Neurons are very greedy for fuel from the blood and require a lot of support from companion cells. Hence, a lot of measurement of the site, amount and timing of brain activity is done via measuring electrical activity, neurotransmitter levels or blood flow.
We can consider this activity at three levels. The first is a single-cell level, wherein individual neurons communicate. But measurement at this level is difficult (laboratory-based) and provides a limited picture.
As such, we rely more on measurements done on a network level, where a series of neurons or networks are activated. Or, we measure whole-of-brain activity patterns which can incorporate one or more so-called “brain states”.
According to a recent definition, brain states are “recurring activity patterns distributed across the brain that emerge from physiological or cognitive processes”. These states are functionally relevant, which means they are related to behaviour.
Brain states involve the synchronisation of different brain regions, something that’s been most readily observed in animal models, usually rodents. Only now are we starting to see some evidence in human studies.
Various kinds of states
The most commonly-studied brain states in both rodents and humans are states of “arousal” and “resting”. You can picture these as various levels of alertness.
Studies show environmental factors and activity influence our brain states. Activities or environments with high cognitive demands drive “attentional” brain states (so-called task-induced brain states) with increased connectivity. Examples of task-induced brain states include complex behaviours such as reward anticipation, mood, hunger and so on.
In contrast, a brain state such as “mind-wandering” seems to be divorced from one’s environment and tasks. Dropping into daydreaming is, by definition, without connection to the real world.
We can’t currently disentangle multiple “states” that exist in the brain at any given time and place. As mentioned earlier, this is because of the trade-offs that come with recording spatial (brain region) versus temporal (timing) brain activity.
Brain states vs brain waves
Brain state work can be couched in terms such as alpha, delta and so forth. However, this is actually referring to brain waves which specifically come from measuring brain activity using EEG.
EEG picks up on changing electrical activity in the brain, which can be sorted into different frequencies (based on wavelength). Classically, these frequencies have had specific associations:
- gamma is linked with states or tasks that require more focused concentration
- beta is linked with higher anxiety and more active states, with attention often directed externally
- alpha is linked with being very relaxed, and passive attention (such as listening quietly but not engaging)
- theta is linked with deep relaxation and inward focus
- and delta is linked with deep sleep.
Brain wave patterns are used a lot to monitor sleep stages. When we fall asleep we go from drowsy, light attention that’s easily roused (alpha), to being relaxed and no longer alert (theta), to being deeply asleep (delta).
Can we control our brain states?
The question on many people’s minds is: can we judiciously and intentionally influence our brain states?
For now, it’s likely too simplistic to suggest we can do this, as the actual mechanisms that influence brain states remain hard to detangle. Nonetheless, researchers are investigating everything from the use of drugs, to environmental cues, to practising mindfulness, meditation and sensory manipulation.
Controversially, brain wave patterns are used in something called “neurofeedback” therapy. In these treatments, people are given feedback (such as visual or auditory) based on their brain wave activity and are then tasked with trying to maintain or change it. To stay in a required state they may be encouraged to control their thoughts, relax, or breathe in certain ways.
The applications of this work are predominantly around mental health, including for individuals who have experienced trauma, or who have difficulty self-regulating – which may manifest as poor attention or emotional turbulence.
However, although these techniques have intuitive appeal, they don’t account for the issue of multiple brain states being present at any given time. Overall, clinical studies have been largely inconclusive, and proponents of neurofeedback therapy remain frustrated by a lack of orthodox support.
Other forms of neurofeedback are delivered by MRI-generated data. Participants engaging in mental tasks are given signals based on their neural activity, which they use to try and “up-regulate” (activate) regions of the brain involved in positive emotions. This could, for instance, be useful for helping people with depression.
Another potential method claimed to purportedly change brain states involves different sensory inputs. Binaural beats are perhaps the most popular example, wherein two different wavelengths of sound are played in each ear. But the evidence for such techniques is similarly mixed.
Treatments such as neurofeedback therapy are often very costly, and their success likely relies as much on the therapeutic relationship than the actual therapy.
On the bright side, there’s no evidence these treatment do any harm – other than potentially delaying treatments which have been proven to be beneficial.
Susan Hillier, Professor: Neuroscience and Rehabilitation, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Feel-Good Productivity – by Dr. Ali Abdaal
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Rise and grind” is not a sustainable way to live. Yet for most of us, there are things we do have to do every day that we don’t necessarily do for fun. So, how to be productive with those things, and not feel like we are constantly compromising and sacrificing our time on this earth for some intrinsically trivial but extrinsically required activity that’ll be forgotten tomorrow?
And most of us do also have dreams and ambitions (and if you don’t, then what were they before life snatched them away from you?), things to work towards. So there is “carrot” for us as well as “stick”. But how to break the cycle and get more carrot and less stick, while being more productive than before?
Dr. Abdaal frames this principally in terms of neurology first, psychology next.
That when we are bored, we simply do not have the neurochemicals required to work well anyway, so addressing that first needs to be a priority. He lays out many ways of doing this, gives lots of practical tips, and brings attention to the ways it’s easy to go wrong (and how to fix those too).
The writing style isdeceptively relaxed and casual, leading the reader smoothly into understanding of each topic before moving on.
Bottom line: if you want to get more done while feeling better about it (not a tired wreck), then this is the book for you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Toothpastes & Mouthwashes: Which Help And Which Harm?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Toothpastes and mouthwashes: which kinds help, and which kinds harm?
You almost certainly brush your teeth. You might use mouthwash. A lot of people floss for three weeks at a time, often in January.
There are a lot of options for oral hygiene; variations of the above, and many alternatives too. This is a big topic, so rather than try to squeeze it all in one, this will be a several-part series.
For today, let’s look at toothpastes and mouthwashes, to start!
Toothpaste options
Toothpastes may contain one, some, or all of the following, so here are some notes on those:
Fluoride
Most toothpastes contain fluoride; this is generally recognized as safe though is not without its controversies. The fluoride content is the reason it’s recommended not to swallow toothpaste, though.
The fluoride in toothpaste can cause some small problems if overused; if you see unusually white patches on your teeth (your teeth are supposed to be ivory-colored, not truly white), that is probably a case of localized overcalcification because of the fluoride, and yes, you can have too much of a good thing.
Overall, the benefits are considered to far outweigh the risks, though.
Baking soda
Whether by itself or as part of a toothpaste, baking soda is a safe and effective choice, not just for cosmetic purposes, but for boosting genuine oral hygiene too:
- Enhanced plaque removal to improve gingival health: 3-month randomized clinical study of the effects of baking soda toothpaste on plaque and gingivitis
- The effects of two baking-soda toothpastes in enhancing mechanical plaque removal and improving gingival health: A 6-month randomized clinical study
- The efficacy of baking soda dentifrice in controlling plaque and gingivitis: A systematic review
Activated charcoal
Activated charcoal is great at removing many chemicals from things it touches. That includes the kind you might see on your teeth in the form of stains.
A topical aside on safety: activated charcoal is a common ingredient in a lot of black-colored Halloween-themed foods and drinks around this time of year. Beware, if you ingest these, there’s a good chance of it also cleaning out any meds you are taking. Ask your pharmacist about your own personal meds, but meds that (ingested) activated charcoal will usually remove include:
- Oral HRT / contraceptives
- Antidepressants (many kinds)
- Heart medications (at least several major kinds)
Toothpaste, assuming you are spitting-not-swallowing, won’t remove your medications though. Nor, in case you were worrying, will it strip tooth enamel, even if you have extant tooth enamel erosion:
Source: Activated charcoal toothpastes do not increase erosive tooth wear
However, it’s of no special extra help when it comes to oral hygiene itself, just removing stains.
So, if you’d like to use it for cosmetic reasons, go right ahead. If not, no need.
Hydrogen peroxide
This is generally not a good idea, speaking for the health. For whitening, yes, it works. But for health, not so much:
To be clear, when they say “alter”, they mean “in a bad way”. It increases inflammation and tissue damage.
If buying commercially-available whitening toothpaste made with hydrogen peroxide, the academic answer is that it’s a lottery, because brands’ proprietorial compounding processes vary widely and constantly with little oversight and even less transparency:
Is whitening toothpaste safe for dental health?: RDA-PE method
Mouthwash options
In the case of fluoride and hydrogen peroxide, the same advice (for and against) goes as per toothpaste.
Alcohol
There has been some concern about the potential carcinogenic effect of alcohol-based mouthwashes. According to the best current science, this one’s not an easy yes-or-no, but rather:
- If there are no other cancer risk factors, it does not seem to increase cancer risk
- If there are other cancer risk factors, it does make the risk worse
Read more:
- Does the use of alcohol mouthwash increase the risk of developing oral cancer?
- Alcohol-based mouthwash as a risk factor of oral cancer: A systematic review
Non-Alcohol
Non-alcoholic mouthwashes are not without their concerns either. In this case, the potential problem is changing the oral microbiome (we are supposed to have one!), and specifically, that the spread of what it kills and what it doesn’t may result in an imbalance that causes a lowering of the pH of the mouth.
Put differently: it makes your saliva more acidic.
Needless to say, that can cause its own problems for teeth. The research on this is still emerging, with regard to whether the benefits outweigh the problems, but the fact that it has this effect seems to be a consensus. Here’s an example paper; there are others:
Effects of Chlorhexidine mouthwash on the oral microbiome
Flossing, scraping, and alternatives
These are important (and varied, and interesting) enough to merit their own main feature, rather than squeezing them in at the end.
So, watch this space for a main feature on these soon!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: