Pear vs Prickly Pear – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pear to prickly pear, we picked the prickly.
Why?
Both of these fruits are fine and worthy choices, but the prickly pear wins out in nutritional density.
Looking at the macros to start with, the prickly pear is higher in fiber and lower in carbs, resulting in a much lower glycemic index. However, non-prickly pears are already low GI, so this is not a huge matter. Whether it’s pear’s GI of 38 or prickly pear’s GI of 7, you’re unlikely to experience a glucose spike.
In the category of vitamins, pear has a little more of vitamins B5, B9, E, K, and choline, but the margins are tiny. On the other hand, prickly pear has more of vitamins A, B1, B2, B3, B6, and C, with much larger margins of difference (except vitamin B1; that’s still quite close). Even before taking margins of difference into account, this is a slight win for prickly pear.
When it comes to minerals, things are more pronounced; pear has more manganese, while prickly pear has more calcium, iron, magnesium, phosphorus, potassium, selenium, and zinc.
In short, both pears are great (so do enjoy the pair), but prickly pear is the clear winner where one must be declared.
Want to learn more?
You might like to read:
Apple vs Pear – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Could not getting enough sleep increase your risk of type 2 diabetes?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not getting enough sleep is a common affliction in the modern age. If you don’t always get as many hours of shut-eye as you’d like, perhaps you were concerned by news of a recent study that found people who sleep less than six hours a night are at higher risk of type 2 diabetes.
So what can we make of these findings? It turns out the relationship between sleep and diabetes is complex.
The study
Researchers analysed data from the UK Biobank, a large biomedical database which serves as a global resource for health and medical research. They looked at information from 247,867 adults, following their health outcomes for more than a decade.
The researchers wanted to understand the associations between sleep duration and type 2 diabetes, and whether a healthy diet reduced the effects of short sleep on diabetes risk.
As part of their involvement in the UK Biobank, participants had been asked roughly how much sleep they get in 24 hours. Seven to eight hours was the average and considered normal sleep. Short sleep duration was broken up into three categories: mild (six hours), moderate (five hours) and extreme (three to four hours). The researchers analysed sleep data alongside information about people’s diets.
Some 3.2% of participants were diagnosed with type 2 diabetes during the follow-up period. Although healthy eating habits were associated with a lower overall risk of diabetes, when people ate healthily but slept less than six hours a day, their risk of type 2 diabetes increased compared to people in the normal sleep category.
The researchers found sleep duration of five hours was linked with a 16% higher risk of developing type 2 diabetes, while the risk for people who slept three to four hours was 41% higher, compared to people who slept seven to eight hours.
One limitation is the study defined a healthy diet based on the number of servings of fruit, vegetables, red meat and fish a person consumed over a day or a week. In doing so, it didn’t consider how dietary patterns such as time-restricted eating or the Mediterranean diet may modify the risk of diabetes among those who slept less.
Also, information on participants’ sleep quantity and diet was only captured at recruitment and may have changed over the course of the study. The authors acknowledge these limitations.
Why might short sleep increase diabetes risk?
In people with type 2 diabetes, the body becomes resistant to the effects of a hormone called insulin, and slowly loses the capacity to produce enough of it in the pancreas. Insulin is important because it regulates glucose (sugar) in our blood that comes from the food we eat by helping move it to cells throughout the body.
We don’t know the precise reasons why people who sleep less may be at higher risk of type 2 diabetes. But previous research has shown sleep-deprived people often have increased inflammatory markers and free fatty acids in their blood, which impair insulin sensitivity, leading to insulin resistance. This means the body struggles to use insulin properly to regulate blood glucose levels, and therefore increases the risk of type 2 diabetes.
Further, people who don’t sleep enough, as well as people who sleep in irregular patterns (such as shift workers), experience disruptions to their body’s natural rhythm, known as the circadian rhythm.
This can interfere with the release of hormones like cortisol, glucagon and growth hormones. These hormones are released through the day to meet the body’s changing energy needs, and normally keep blood glucose levels nicely balanced. If they’re compromised, this may reduce the body’s ability to handle glucose as the day progresses.
These factors, and others, may contribute to the increased risk of type 2 diabetes seen among people sleeping less than six hours.
Millions of people around the world have diabetes. WESTOCK PRODUCTIONS/Shutterstock While this study primarily focused on people who sleep eight hours or less, it’s possible longer sleepers may also face an increased risk of type 2 diabetes.
Research has previously shown a U-shaped correlation between sleep duration and type 2 diabetes risk. A review of multiple studies found getting between seven to eight hours of sleep daily was associated with the lowest risk. When people got less than seven hours sleep, or more than eight hours, the risk began to increase.
The reason sleeping longer is associated with increased risk of type 2 diabetes may be linked to weight gain, which is also correlated with longer sleep. Likewise, people who don’t sleep enough are more likely to be overweight or obese.
Good sleep, healthy diet
Getting enough sleep is an important part of a healthy lifestyle and may reduce the risk of type 2 diabetes.
Based on this study and other evidence, it seems that when it comes to diabetes risk, seven to eight hours of sleep may be the sweet spot. However, other factors could influence the relationship between sleep duration and diabetes risk, such as individual differences in sleep quality and lifestyle.
While this study’s findings question whether a healthy diet can mitigate the effects of a lack of sleep on diabetes risk, a wide range of evidence points to the benefits of healthy eating for overall health.
The authors of the study acknowledge it’s not always possible to get enough sleep, and suggest doing high-intensity interval exercise during the day may offset some of the potential effects of short sleep on diabetes risk.
In fact, exercise at any intensity can improve blood glucose levels.
Giuliana Murfet, Casual Academic, Faculty of Health, University of Technology Sydney and ShanShan Lin, Senior Lecturer, School of Public Health, University of Technology Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
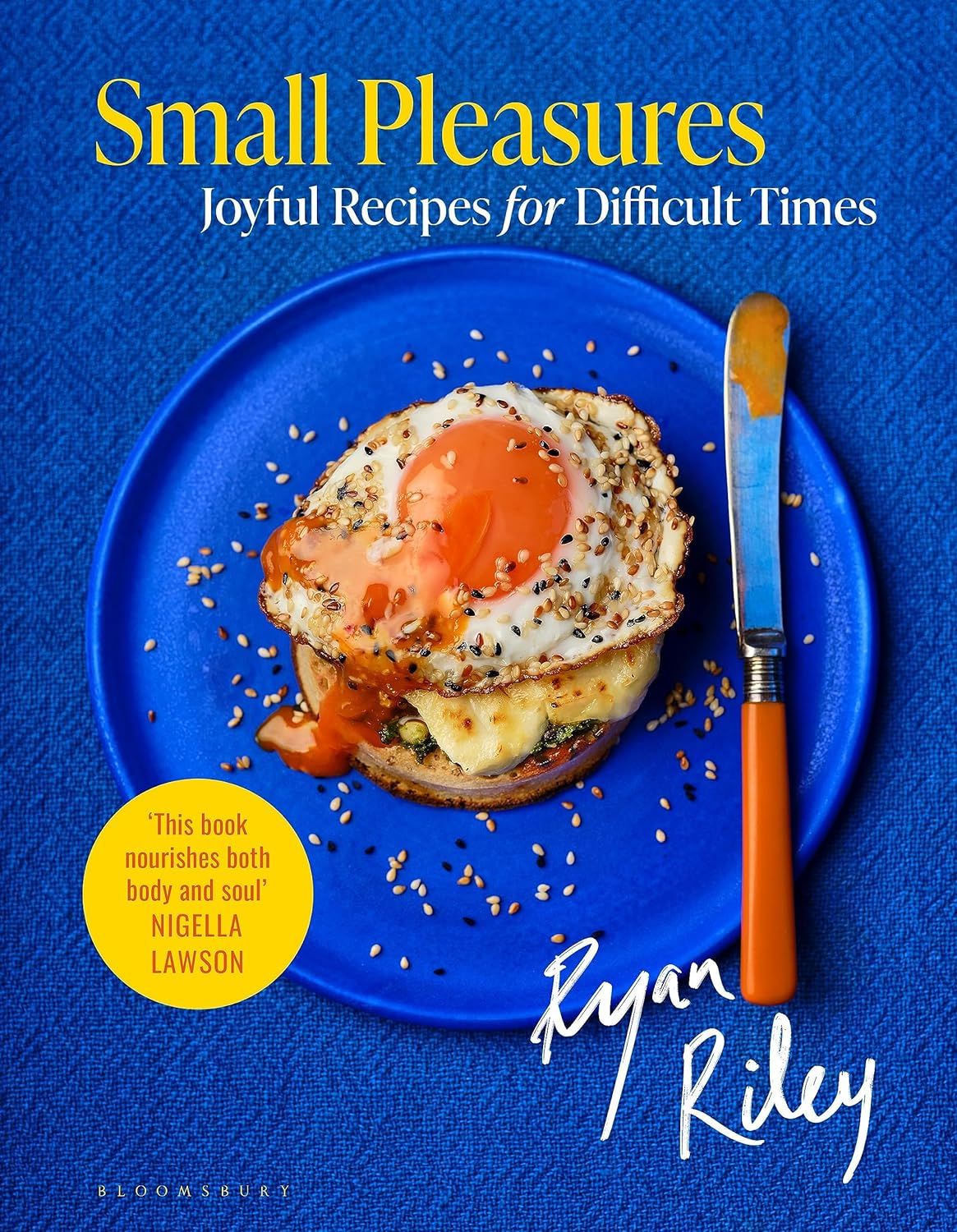
Small Pleasures – by Ryan Riley
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Hippocrates said “let food be thy medicine, and let medicine be thy food”, he may or may not have had this book in mind.
In terms of healthiness, this one’s not the very most nutritionist-approved recipe book we’ve ever reviewed. It’s not bad, to be clear!
But the physical health aspect is secondary to the mental health aspects, in this one, as you’ll see. And as we say, “mental health is also just health”.
The book is divided into three sections:
- Comfort—for when you feel at your worst, for when eating is a chore, for when something familiar and reassuring will bring you solace. Here we find flavor and simplicity; pastas, eggs, stews, potato dishes, and the like.
- Restoration—for when your energy needs reawakening. Here we find flavors fresh and tangy, enlivening and bright. Things to make you feel alive.
- Pleasure—while there’s little in the way of health-food here, the author describes the dishes in this section as “a love letter to yourself; they tell you that you’re special as you ready yourself to return to the world”.
And sometimes, just sometimes, we probably all need a little of that.
Bottom line: if you’d like to bring a little more joie de vivre to your cuisine, this book can do that.
Click here to check out Small Pleasures, and rekindle joy in your kitchen!
Share This Post
-
Cool As A Cucumber
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cucumber Extract Beats Glucosamine & Chondroitin… At 1/135th Of The Dose?!
Do you take glucosamine & chondroitin supplements for your bone-and-joint health?
Or perhaps, like many, you take them intermittently because they mean taking several large tablets a day. Or maybe you don’t take them at all because they generally contain ingredients derived from shellfish?
Cucumber extract has your back! (and your knees, and your hips, and…)
It’s plant-derived (being from botanical cucumbers, not sea cucumbers, the aquatic animal!) and requires only 1/135th of the dosage to produce twice the benefits!
Distilling the study to its absolute bare bones for your convenience:
- Cucumber extract (10mg) was pitted against glucosamine & chondroitin (1350mg)
- Cucumber extract performed around 50% better than G&C after 30 days
- Cucumber extract performed more than 200% better than G&C after 180 days
In conclusion, this study indicates that, in very lay terms:
Cucumber extract blows glucosamine & chondroitin out of the water as a treatment and preventative for joint pain
Share This Post
Related Posts
-
6 Signs Of Stroke (One Month In Advance)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most people can recognise the signs of a stroke when it’s just happened, but knowing the signs that appear a month beforehand would be very useful. That’s what this video’s about!
The Warning Signs
- Persistently elevated blood pressure: one more reason to have an at-home testing kit and use it regularly! Or a smartwatch or similar that’ll do it for you. The reason this is relevant is because high blood pressure can lead to damaging blood vessels, causing a stroke.
- Excessive fatigue: of course, this one can have many possible causes, but one of them is a “transient ischemic attack” (TIA), which is essentially a micro-stroke, and can be a precursor to a more severe stroke. So, we’re not doing the Google MD thing here of saying “if this, then that”, but we are saying: paying attention to the overall patterns can be very useful. Rather than fretting unduly about a symptom in isolation, see how it fits into the big picture.
- Vision problems: especially if sudden-onset with no obvious alternative cause can be a sign of neural damage, and may indicate a stroke on the way.
- Speech problems: if there’s not an obvious alternative explanation (e.g. you’ve just finished your third martini, or was this the fourth?), then speech problems (e.g. slurred speech, trouble forming sentences, etc) are a very worrying indicator and should be treated as a medical emergency.
- Neurological problems: a bit of a catch-all category, but memory issues, loss of balance, nausea without an obvious alternative cause, are all things that should get checked out immediately just in case.
- Numbness or weakness in the extremities: especially if on one side of the body only, is often caused by the TIA we mentioned earlier. If it’s both sides, then peripheral neuropathy may be the culprit, but having a neurologist take a look at it is a good idea either way.
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Two Things You Can Do To Improve Stroke Survival Chances
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Nobody’s Sleeping – by Dr. Bijoy John
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Firstly, let’s mention: yes, for the sake of being methodical and comprehensive this book does give the same baseline advice as every other sleep book out there. However, it gives something else, too:
It goes beyond that baseline, to a) give more personalized advice for various demographics (e.g. per age, sex, health conditions, etc) and b) give direction for further personalizing one’s own sleep improvement journey, by troubleshooting and fixing things that may pertain to you very specifically and not to most people.
This means, that if you’re doing “all the right things” but still having sleep-related problems, there is hope and there are more approaches to try.
The style in which this is delivered is very readable, which is good, because if one hasn’t been sleeping well, then chances are that an intellectual challenge would be about as welcome as a physical challenge—that is to say: not at all.
Bottom line: if sleep is not your strength and you would like it to be and all the usual things haven’t yet worked, this book may well help you to overcome the hurdles between you and a good night’s sleep each night.
Click here to check out Nobody’s Sleeping, and refute that title!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Even small diet tweaks can lead to sustainable weight loss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s a well-known fact that to lose weight, you either need to eat less or move more. But how many calories do you really need to cut out of your diet each day to lose weight? It may be less than you think.
To determine how much energy (calories) your body requires, you need to calculate your total daily energy expenditure (TDEE). This is comprised of your basal metabolic rate (BMR) – the energy needed to sustain your body’s metabolic processes at rest – and your physical activity level. Many online calculators can help determine your daily calorie needs.
If you reduce your energy intake (or increase the amount you burn through exercise) by 500-1,000 calories per day, you’ll see a weekly weight loss of around one pound (0.45kg).
But studies show that even small calorie deficits (of 100-200 calories daily) can lead to long-term, sustainable weight-loss success. And although you might not lose as much weight in the short-term by only decreasing calories slightly each day, these gradual reductions are more effective than drastic cuts as they tend to be easier to stick with.
Small diet changes can still lead to weight loss in the long run. Monkey Business Images/ Shutterstock Hormonal changes
When you decrease your calorie intake, the body’s BMR often decreases. This phenomenon is known as adaptive thermogenesis. This adaptation slows down weight loss so the body can conserve energy in response to what it perceives as starvation. This can lead to a weight-loss plateau – even when calorie intake remains reduced.
Caloric restriction can also lead to hormonal changes that influence metabolism and appetite. For instance, thyroid hormones, which regulate metabolism, can decrease – leading to a slower metabolic rate. Additionally, leptin levels drop, reducing satiety, increasing hunger and decreasing metabolic rate.
Ghrelin, known as the “hunger hormone”, also increases when caloric intake is reduced, signalling the brain to stimulate appetite and increase food intake. Higher ghrelin levels make it challenging to maintain a reduced calorie diet, as the body constantly feels hungrier.
Insulin, which helps regulate blood sugar levels and fat storage, can improve in sensitivity when we reduce calorie intake. But sometimes, insulin levels decrease instead, affecting metabolism and leading to a reduction in daily energy expenditure. Cortisol, the stress hormone, can also spike – especially when we’re in a significant caloric deficit. This may break down muscles and lead to fat retention, particularly in the stomach.
Lastly, hormones such as peptide YY and cholecystokinin, which make us feel full when we’ve eaten, can decrease when we lower calorie intake. This may make us feel hungrier.
Fortunately, there are many things we can do to address these metabolic adaptations so we can continue losing weight.
Weight loss strategies
Maintaining muscle mass (either through resistance training or eating plenty of protein) is essential to counteract the physiological adaptations that slow weight loss down. This is because muscle burns more calories at rest compared to fat tissue – which may help mitigate decreased metabolic rate.
Portion control is one way of decreasing your daily calorie intake. Fevziie/ Shutterstock Gradual caloric restriction (reducing daily calories by only around 200-300 a day), focusing on nutrient-dense foods (particularly those high in protein and fibre), and eating regular meals can all also help to mitigate these hormonal challenges.
But if you aren’t someone who wants to track calories each day, here are some easy strategies that can help you decrease daily calorie intake without thinking too much about it:
1. Portion control: reducing portion sizes is a straightforward way of reducing calorie intake. Use smaller plates or measure serving sizes to help reduce daily calorie intake.
2. Healthy swaps: substituting high-calorie foods with lower-calorie alternatives can help reduce overall caloric intake without feeling deprived. For example, replacing sugary snacks with fruits or swapping soda with water can make a substantial difference to your calorie intake. Fibre-rich foods can also reduce the calorie density of your meal.
3. Mindful eating: practising mindful eating involves paying attention to hunger and fullness cues, eating slowly, and avoiding distractions during meals. This approach helps prevent overeating and promotes better control over food intake.
4. Have some water: having a drink with your meal can increase satiety and reduce total food intake at a given meal. In addition, replacing sugary beverages with water has been shown to reduce calorie intake from sugars.
4. Intermittent fasting: restricting eating to specific windows can reduce your caloric intake and have positive effects on your metabolism. There are different types of intermittent fasting you can do, but one of the easiest types is restricting your mealtimes to a specific window of time (such as only eating between 12 noon and 8pm). This reduces night-time snacking, so is particularly helpful if you tend to get the snacks out late in the evening.
Long-term behavioural changes are crucial for maintaining weight loss. Successful strategies include regular physical activity, continued mindful eating, and periodically being diligent about your weight and food intake. Having a support system to help you stay on track can also play a big role in helping you maintain weight loss.
Modest weight loss of 5-10% body weight in people who are overweight or obese offers significant health benefits, including improved metabolic health and reduced risk of chronic diseases. But it can be hard to lose weight – especially given all the adaptations our body has to prevent it from happening.
Thankfully, small, sustainable changes that lead to gradual weight loss appear to be more effective in the long run, compared with more drastic lifestyle changes.
Alexandra Cremona, Lecturer, Human Nutrition and Dietetics, University of Limerick
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: