Why You Probably Need More Sleep
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sleep: yes, you really do still need it!
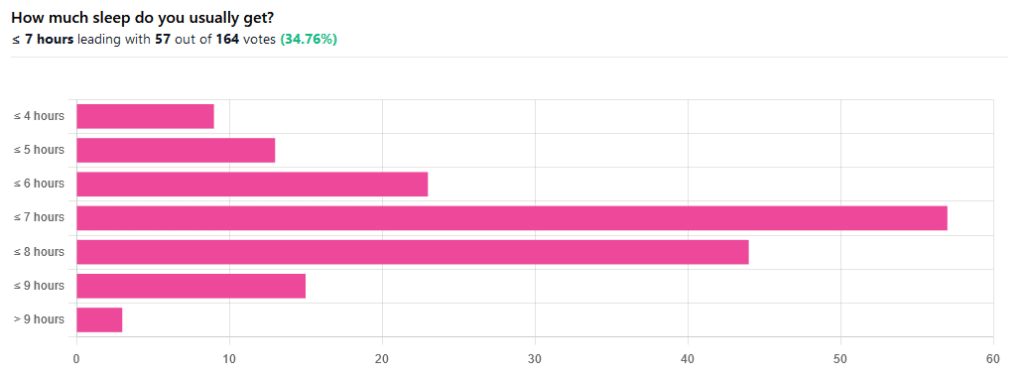
We asked you how much sleep you usually get, and got the above-pictured, below-described set of responses:
- A little of a third of all respondents selected the option “< 7 hours”
- However, because respondents also selected options such as < 6 hours, < 5 hours, and < 4 hours, so if we include those in the tally, the actual total percentage of respondents who reported getting under 7 hours, is actually more like 62%, or just under two thirds of all respondents.
- Nine respondents, which was about 5% of the total, reported usually getting under 4 hours sleep
- A little over quarter of respondents reported usually getting between 7 and 8 hours sleep
- Fifteen respondents, which was a little under 10% of the total, reported usually getting between 8 and 9 hours of sleep
- Three respondents, which was a little under 2% of the total, reported getting over 9 hours of sleep
- In terms of the classic “you should get 7–9 hours sleep”, approximately a third of respondents reported getting this amount.
You need to get 7–9 hours sleep: True or False?
True! Unless you have a (rare!) mutated ADRB1 gene, which reduces that.
The way to know whether you have this, without genomic testing to know for sure, is: do you regularly get under 6.5 hours sleep, and yet continue to go through life bright-eyed and bushy-tailed? If so, you probably have that gene. If you experience daytime fatigue, brain fog, and restlessness, you probably don’t.
About that mutated ADRB1 gene:
NIH | Gene identified in people who need little sleep
Quality of sleep matters as much as duration, and a lot of studies use the “RU-Sated” framework, which assesses six key dimensions of sleep that have been consistently associated with better health outcomes. These are:
- regularity / usual hours
- satisfaction with sleep
- alertness during waking hours
- timing of sleep
- efficiency of sleep
- duration of sleep
But, that doesn’t mean that you can skimp on the last one if the others are in order. In fact, getting a good 7 hours sleep can reduce your risk of getting a cold by three or four times (compared with six or fewer hours):
Behaviorally Assessed Sleep and Susceptibility to the Common Cold
^This study was about the common cold, but you may be aware there are more serious respiratory viruses freely available, and you don’t want those, either.
Napping is good for the health: True or False?
True or False, depending on how you’re doing it!
If you’re trying to do it to sleep less in total (per polyphasic sleep scheduling), then no, this will not work in any sustainable fashion and will be ruinous to the health. We did a Mythbusting Friday special on specifically this, a while back:
Could Just Two Hours Sleep Per Day Be Enough?
PS: you might remember Betteridge’s Law of Headlines
If you’re doing it as a energy-boosting supplement to a reasonable night’s sleep, napping can indeed be beneficial to the health, and can give benefits such as:
- Increased alertness
- Helps with learning
- Improved memory
- Boost to immunity
- Enhance athletic performance
However! There is still a right and a wrong way to go about it, and we wrote about this previously, for a Saturday Life Hacks edition of 10almonds:
How To Nap Like A Pro (No More “Sleep Hangovers”!)
As we get older, we need less sleep: True or False
False, with one small caveat.
The small caveat: children and adolescents need 9–12 hours sleep because, uncredited as it goes, they are doing some seriously impressive bodybuilding, and that is exhausting to the body. So, an adult (with a normal lifestyle, who is not a bodybuilder) will tend to need less sleep than a child/adolescent.
But, the statement “As we get older, we need less sleep” is generally taken to mean “People in the 65+ age bracket need less sleep than younger adults”, and this popular myth is based on anecdotal observational evidence: older people tend to sleep less (as our survey above shows! For any who aren’t aware, our readership is heavily weighted towards the 60+ demographic), and still continue functioning, after all.
Just because we survive something with a degree of resilience doesn’t mean it’s good for us.
In fact, there can be serious health risks from not getting enough sleep in later years, for example:
Sleep deficiency promotes Alzheimer’s disease development and progression
Want to get better sleep?
What gets measured, gets done. Sleep tracking apps can be a really good tool for getting one’s sleep on a healthier track. We compared and contrasted some popular ones:
The Head-To-Head Of Google and Apple’s Top Apps For Getting Your Head Down
Take good care of yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
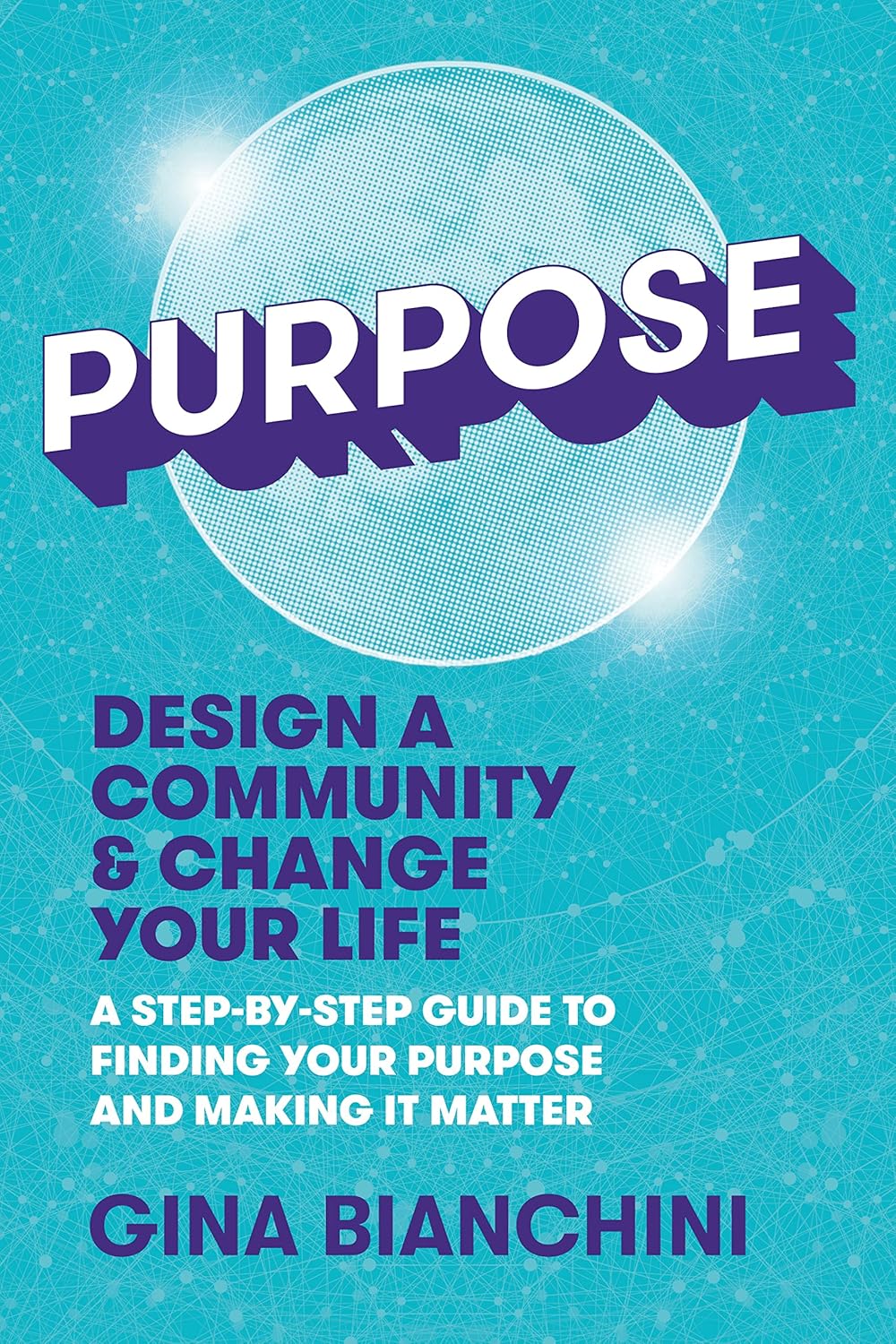
Purpose – by Gina Bianchini
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
To address the elephant in the room, this is not a rehash of Rick Warren’s best-selling “The Purpose-Driven Life”. Instead, this book is (in this reviewer’s opinion) a lot better. It’s a lot more comprehensive, and it doesn’t assume that what’s most important to the author will be what’s most important to you.
What’s it about, then? It’s about giving your passion (whatever it may be) the tools to have an enduring impact on the world. It recommends doing this by leveraging a technology that would once have been considered magic: social media.
Far from “grow your brand” business books, this one looks at what really matters the most to you. Nobody will look back on your life and say “what a profitable second quarter that was in such-a-year”. But if you do your thing well, people will look back and say:
- “he was a pillar of the community”
- “she raised that community around her”
- “they did so much for us”
- “finding my place in that community changed my life”
- …and so forth. Isn’t that something worth doing?
Bianchini takes the position of both “idealistic dreamer” and “realistic worker”.
Further, she blends the two beautifully, to give practical step-by-step instructions on how to give life to the community that you build.
Share This Post
-
I want to eat healthily. So why do I crave sugar, salt and carbs?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We all want to eat healthily, especially as we reset our health goals at the start of a new year. But sometimes these plans are sabotaged by powerful cravings for sweet, salty or carb-heavy foods.
So why do you crave these foods when you’re trying to improve your diet or lose weight? And what can you do about it?
There are many reasons for craving specific foods, but let’s focus on four common ones:
1. Blood sugar crashes
Sugar is a key energy source for all animals, and its taste is one of the most basic sensory experiences. Even without specific sweet taste receptors on the tongue, a strong preference for sugar can develop, indicating a mechanism beyond taste alone.
Neurons responding to sugar are activated when sugar is delivered to the gut. This can increase appetite and make you want to consume more. Giving into cravings also drives an appetite for more sugar.
In the long term, research suggests a high-sugar diet can affect mood, digestion and inflammation in the gut.
While there’s a lot of variation between individuals, regularly eating sugary and high-carb foods can lead to rapid spikes and crashes in blood sugar levels. When your blood sugar drops, your body can respond by craving quick sources of energy, often in the form of sugar and carbs because these deliver the fastest, most easily accessible form of energy.
2. Drops in dopamine and serotonin
Certain neurotransmitters, such as dopamine, are involved in the reward and pleasure centres of the brain. Eating sugary and carb-rich foods can trigger the release of dopamine, creating a pleasurable experience and reinforcing the craving.
Serotonin, the feel-good hormone, suppresses appetite. Natural changes in serotonin can influence daily fluctuations in mood, energy levels and attention. It’s also associated with eating more carb-rich snacks in the afternoon.
Do you get 3pm sugar cravings? Serotonin could play a role.
Marcus Aurelius/PexelsLow carb diets may reduce serotonin and lower mood. However, a recent systematic review suggests little association between these diets and risk for anxiety and depression.
Compared to men, women tend to crave more carb rich foods. Feeling irritable, tired, depressed or experiencing carb cravings are part of premenstrual symptoms and could be linked to reduced serotonin levels.
3. Loss of fluids and drops in blood sugar and salt
Sometimes our bodies crave the things they’re missing, such as hydration or even salt. A low-carb diet, for example, depletes insulin levels, decreasing sodium and water retention.
Very low-carb diets, like ketogenic diets, induce “ketosis”, a metabolic state where the body switches to using fat as its primary energy source, moving away from the usual dependence on carbohydrates.
Ketosis is often associated with increased urine production, further contributing to potential fluid loss, electrolyte imbalances and salt cravings.
4. High levels of stress or emotional turmoil
Stress, boredom and emotional turmoil can lead to cravings for comfort foods. This is because stress-related hormones can impact our appetite, satiety (feeling full) and food preferences.
The stress hormone cortisol, in particular, can drive cravings for sweet comfort foods.
A 2001 study of 59 premenopausal women subjected to stress revealed that the stress led to higher calorie consumption.
A more recent study found chronic stress, when paired with high-calorie diet, increases food intake and a preference for sweet foods. This shows the importance of a healthy diet during stress to prevent weight gain.
What can you do about cravings?
Here are four tips to curb cravings:
1) don’t cut out whole food groups. Aim for a well-balanced diet and make sure you include:
- sufficient protein in your meals to help you feel full and reduce the urge to snack on sugary and carb-rich foods. Older adults should aim for 20–40g protein per meal with a particular focus on breakfast and lunch and an overall daily protein intake of at least 0.8g per kg of body weight for muscle health
- fibre-rich foods, such as vegetables and whole grains. These make you feel full and stabilise your blood sugar levels. Examples include broccoli, quinoa, brown rice, oats, beans, lentils and bran cereals. Substitute refined carbs high in sugar like processed snack bars, soft drink or baked goods for more complex ones like whole grain bread or wholewheat muffins, or nut and seed bars or energy bites made with chia seeds and oats
2) manage your stress levels. Practise stress-reduction techniques like meditation, deep breathing, or yoga to manage emotional triggers for cravings. Practising mindful eating, by eating slowly and tuning into bodily sensations, can also reduce daily calorie intake and curb cravings and stress-driven eating
3) get enough sleep. Aim for seven to eight hours of quality sleep per night, with a minimum of seven hours. Lack of sleep can disrupt hormones that regulate hunger and cravings
4) control your portions. If you decide to indulge in a treat, control your portion size to avoid overindulging.
Overcoming cravings for sugar, salt and carbs when trying to eat healthily or lose weight is undoubtedly a formidable challenge. Remember, it’s a journey, and setbacks may occur. Be patient with yourself – your success is not defined by occasional cravings but by your ability to manage and overcome them.
Hayley O’Neill, Assistant Professor, Faculty of Health Sciences and Medicine, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
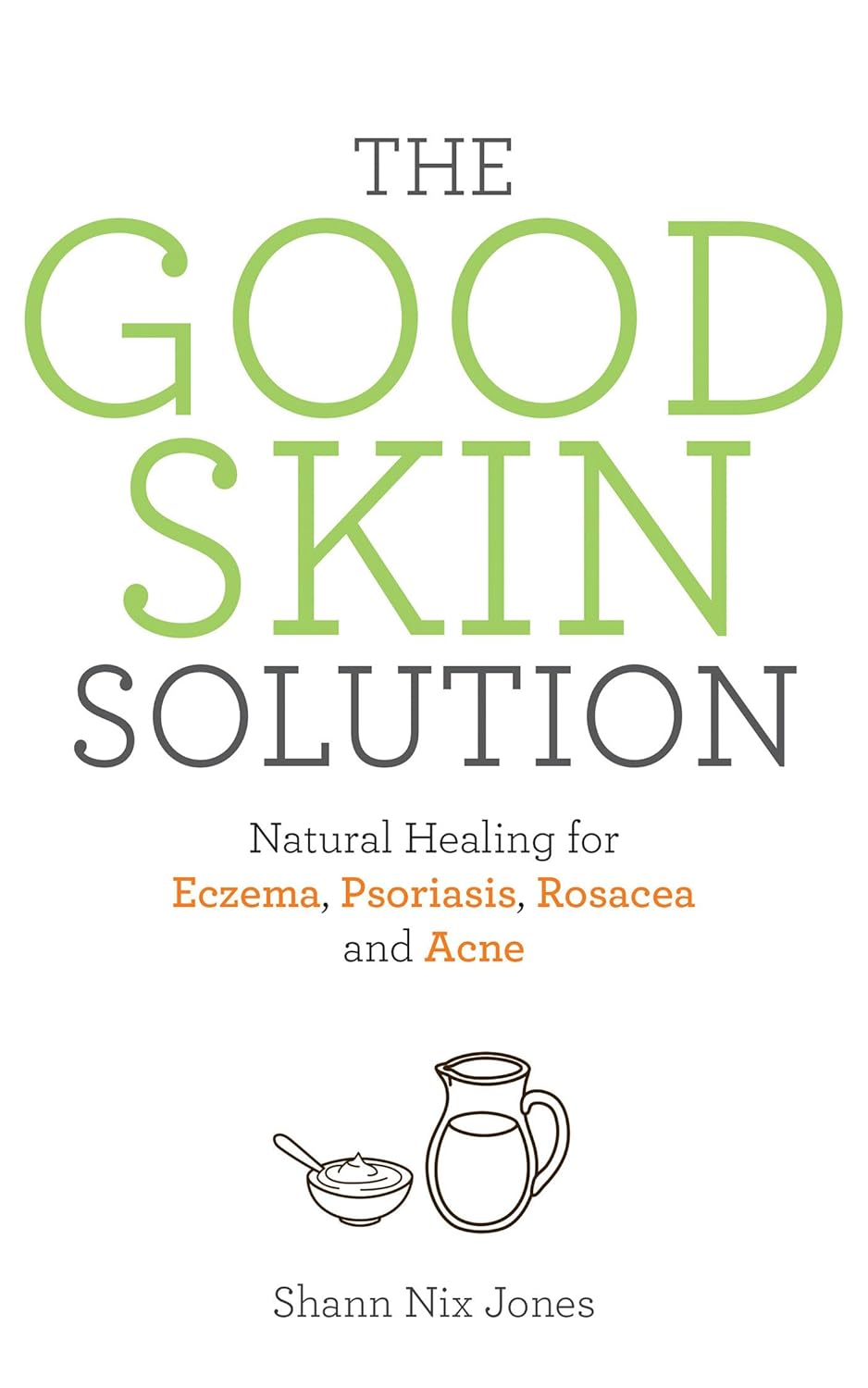
The Good Skin Solution – by Shann Jones
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not everyone knows that eczema is not just a skin condition; it’s an autoimmune condition. And thus to heal one’s skin, the gut is a good place to start.
This is not your average gut health book though, because it is focused on optimizing things for one’s skin… Although the author herself learned about this while helping her husband to battle an MRSA infection. In other words, a multi-fronted battle for sure.
The advices in this book are good for, as the subtitle promises, an assortment of other skin conditions too, including psoriasis, rosacea, and acne. She covers the usual bases, and recommends probiotics, of which she’s particularly keen to praise kefir, while advising against the use of antibiotics unless absolutely necessary—something we’ve talked about from time to time at 10almonds, too.
Not content to merely cover those things, she also talks allergies, and walking the fine line between avoiding triggers and developing hypersensitivity by treating to live in a perfectly clean bubble.
Ultimately, she offers “7 daily habits”, 3 of which involve goat’s milk kefir, that’s how keen on it she is. So if you’re vegan, probably this book isn’t as good value, however much it discusses the health woes that can be caused and/or exacerbated by drinking cow’s milk.
The style is very light and personable, which makes for easy reading, more like one friend talking to another, than a scientific textbook.
Bottom line: if you’d like healthier skin, are interested in dietary tweaks and homemade soaps, and have no aversion to goat’s milk and/or kefir, then this book is full of fascinating pointers.
Click here to check out The Good Skin Solution, and who knows, maybe you’ll find it’s the G.O.A.T!
Share This Post
Related Posts
-
Fruit Is Healthy; Juice Isn’t (Here’s Why)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Biochemist and “Glucose Goddess” Jessie Inchauspé wants us to understand the difference:
Stripped!
A glass of orange juice contains 22 grams of sugar (about six sugar cubes), nearly as much as a can of soda (27 grams).
Orange juice is widely perceived as healthy due to vitamin content—but if you add vitamins to soda, it won’t make it healthy, because the main health effect is still the sugar, leading to glucose spikes and many resultant health risks. The positive image of fruit juice is mainly from industry marketing.
In reality, Inchauspé advises, fruit juice should be treated like a dessert—consumed for pleasure, not health benefits.
But why, then, is fruit healthy if fruit juice is unhealthy? Isn’t the sugar there too?
Whole fruit contains plenty of fiber, which slows sugar absorption and prevents glucose spikes. Juicing strips it of its fiber, leaving water and sugar.
The American Heart Association suggests a sugar limit: 25g/day for women, 36g/day for men. One glass of orange juice nearly meets the daily limit for women. If that’s how you want to “spend” your daily sugar allowance, go for it, but do so consciously, by choice, knowing that the allowance is now “spent”.
In contrast, if you eat whole fruit, that basically “doesn’t count” for sugar purposes. The sugar is there, but the fiber more than offsets it, making whole fruit very good for blood sugars.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Biohack Your Way to Healthy Skin – by Jennifer Sun
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, an aesthetician with a biotech background, explains about the overlap of skin health and skin beauty, making it better from the inside first (diet and other lifestyle factors), and then tweaking things as desired from the outside.
We previous reviewed another book of hers, “Unleashing Your Best Skin”, and this time the focus is on things you can do at home—not requiring expensive salon treatments (the other book covers both approaches; this one simply skips the clinic work and instead has a lot more detail in the at-home category).
As for what she covers, it comes in categories:
- Gadgets to consider investing in, how to pick good ones, and what gadgets to avoid
- Basic skincare knowledge and practice; here we’re talking cleaners, tonics, moisturizers, and so forth
- Best topical and oral ingredients for the skin (and in contrast, ingredients to be wary of)
- Nutrition for skincare; not just “your skin needs these ingredients”, but also…
- Gut health for skincare, which gets a whole chapter just for that
- Biohacking hormones for skincare, including in the cases of various common hormone imbalances (e.g. menopause, PCOS, etc) and other complications not generally thought of in terms of skincare, such as diabetes and hypo-/hyperthyroidism.
- Circulatory health for skincare (blood and lymph)
- Mental health techniques for skincare (including improving sleep, managing stress, supplements to consider, etc).
As with her other book that we reviewed, the book is broadly aimed at women, and the section on sex-hormonal considerations is completely aimed at women, but as for the rest of the book, there’s no pressing reason why this book couldn’t benefit men too. It also addresses considerations when it comes to darker skintones, something that a lot of similar books overlook.
The style is directly instructional, albeit light and conversational in tone, and still with 20+ pages of scientific references to show that she does indeed know her stuff.
Bottom line: if you’d like to improve your skin health, and/but aren’t a fan of going to the salon, then this book will be an invaluable resource.
Click here to check out Biohack Your Way To Healthy Skin, and biohack your way to healthy skin!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Eat To Lose Belly Fat (3 Stages)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Belly fat is easier to gain than it is to lose, and it’s absolutely something that needs more attention in the kitchen than in the gym. Here’s one way of doing it:
By the numbers
First note: this video is by a man, and judging by the numbers mentioned, assumes that the viewer is also a man. An end goal of 10% body fat is a little on the low side for men, and would be dangerous for women. The magic 15% mark that he mentions as being a point where various metabolic things change, is more like 20% for women. All assuming normal hormones, of course, since it is hormones that direct this.
Healthy body fat percentages are (assuming normal hormones) in the range of 20–25% for women and 15–20% for men.
With that in mind…
The idea of this approach is to lose enough weight that your body gets rid of even the most awkward bits (e.g: visceral belly fat, which will often be the last to get used) before, if desired, then maintaining at a slightly higher body fat percentage.
- Stage 1: count calories (we don’t usually recommend this at 10almonds, but he does, so we’re reporting it here) and use your weight in pounds multiplied by 12 to give your daily calorie target. Make the majority of your diet foods that have a large volume:calorie ratio, such as fruits and vegetables, in order to feel full without overloading your metabolism. He has an interesting method of calculating a protein target; instead of the usual “1g/kg of body weight”, he says 1g per cm of height. Doing this consistently should get you to 15% body fat (so, 20%, for women).
- Stage 2: start counting fat intake too, and aim for 20–25% of your daily calories as fat. Continue, aside from that, with what you were doing in Stage 1. Doing this consistently should get you to 12% body fat (so, about 17%, for women). Being under the usual healthy level for a while should allow your body to start getting rid of visceral fat.
- Stage 3: track everything, levelling up your precision (no more “this little thing doesn’t count”), and planning ahead when it comes to social events etc. Doing this consistently should yet you to 10% body fat (so, about 15%, for women). This stage has a good chance of making most people miserable, so if that happens, consider the benefits of going back to the healthier 15% body fat (men) or 20% (women).
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Visceral Belly Fat & How To Lose It ← without calorie-counting! We prefer this 😉
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: