One More Resource Against Osteoporosis!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Your Bones Were Made For Moving Too!
We know that to look after bone health, resistance training is generally what’s indicated. Indeed, we mentioned it yesterday, and we’ve talked about it before:
Resistance Is Useful! (Especially As We Get Older)
We also know that if you have osteoporosis already, some exercises are a better or worse idea than others:
Osteoporosis & Exercises: Which To Do (And Which To Avoid)
However! New research suggests that also getting in your recommended 150 minutes per week of moderate exercise slows bone density loss.
The study by Dr. Tiina Savikangas et al. looked at 299 people in their 70s (just over half being women) and found that, over the course of a year, bone mineral density loss was inversely correlated with moderate exercise as recorded by an accelerometer (as found in most fitness-tracking wearables and smartphones).
In other words: those who got more minutes of exercise, kept more bone mineral density.
As well as monitoring bone mineral density, the study also looked at cross-sectional area, but that remained stable throughout.
As for how much is needed:
❝Even short bursts of activity can be significant for the skeleton, so we also looked at movement in terms of the number and intensity of individual impacts. For example, walking and running cause impacts of different intensities.
We found that impacts that were comparable to at least brisk walking were associated with better preservation of bone mineral density.❞
Read more: Impacts during everyday physical activity can slow bone loss ← pop-science source, interviewing the lead researcher
On which note, we’ve a small bone to pick…
As a small correction, the pop-science source says that the subjects’ ages ranged from 70 to 85 years; the paper, meanwhile, clearly shows that the age-range was 74.4±3.9 years (shown in the “Results” table), rounded to 74.4 ± 4 years, in the abstract. So, certainly no participant was older than 78 years and four months.
Why this matters: the age range itself may be critical or it might not, but what is important is that this highlights how we shouldn’t just believe figures cited in pop-science articles, and it’s always good to click through to the source!
This paper is a particularly fascinating read if you have time, because—unlike a lot of studies—they really took great care to note what exactly can and cannot be inferred from the data, and how and why.
Especially noteworthy was the diligence with which they either controlled for, or recognized that they could not control for, far more variables than most studies even bother to mention.
This kind of transparency is critical for good science, and we’d love to see more of it!
Want to apply this to your life?
Tracking minutes-of-movement is one of the things that fitness trackers are best at, so connect your favourite app (one of these days we’ll do a fitness tracker comparison article) and get moving!
And as for the other things that fitness trackers do? As it turns out, they do have their strengths and weaknesses, which are good to bear in mind:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Head Over Hips
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about managing osteoarthritis (or ideally: avoiding it, but that’s not always an option on the table, of course), so here’s a primer/refresher before we get into the meat of today’s article:
Avoiding/Managing Osteoarthritis
When the head gets in the way
Research shows that the problem with recovery in cases of osteoarthritis of the hip is in fact often not the hip itself, but rather, the head:
❝In fact, the stronger your muscles are, the more protected your joint is, and the less pain you will experience.
Our research has shown that people with hip osteoarthritis were unable to activate their muscles as efficiently, irrespective of strength.
Basically, people with hip arthritis are unable to activate their muscles properly because the brain is actively putting on the brake to stop them from using the muscle.❞
This is a case of a short-term protective response being unhelpful in the long-term. If you injure yourself, your brain will try to inhibit you from exacerbating that injury, such as by (for example) disobliging you from putting weight on an injured joint.
This is great if you merely twisted an ankle and just need to sit back and relax while your body works its healing magic, but it’s counterproductive if it’s a chronic issue like osteoarthritis. In such (i.e. chronic) cases, avoidance of use of the joint will simply cause atrophy of the surrounding muscle and other tissues, leading to more of the very wear-and-tear that led to the osteoarthritis in the first place.
So… How to deal with that?
You probably can exercise
It’s easy to get caught between the dichotomy of “exercise and inflame your joints” vs “rest and your joints seize up”, which is not pleasant.
However, the trick lies in how you exercise, per joint type:
When Bad Joints Stop You From Exercising (5 Things To Change)
…which to be clear, isn’t a case of “avoid using the joint that’s bad”, but is rather “use it in this specific way, so that it gets stronger without doing it more damage in the process”.
Which is exactly what is needed!
Further resources
For those who like learning from short videos, here’s a trio of helpers (along with our own text-based overview for each):
- The Most Underrated Hip Mobility Exercise (Not Stretching)
- Overcome Front-Of-Hip Pain
- 10 Tips To Reduce Morning Pain & Stiffness With Arthritis
And for those who prefer just reading, here’s a book we reviewed on the topic:
11 Minutes to Pain-Free Hips – by Melinda Wright
Take care!
Share This Post
-
Eggcellent News Against Dementia?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s that time of the week again… We hope all our readers have had a great and healthy week! Here are some selections from health news from around the world:
Moderation remains key
Eggs have come under the spotlight for their protective potential against dementia, largely due to their content of omega-3 fatty acids, choline, and other nutrients.
Nevertheless, the study had some limitations (including not measuring the quantity of eggs consumed, just the frequency), and while eating eggs daily showed the lowest rates of dementia, not eating them at all did not significantly alter the risk.
Eating more than 2 eggs per day is still not recommended, however, for reasons of increasing the risk of other health issues, such as heart disease.
Read in full: Could eating eggs prevent dementia?
Related: Eggs: Nutritional Powerhouse or Heart-Health Timebomb?
More than suitable
It’s common for a lot of things to come with the warning “not suitable for those who are pregnant or nursing”, with such frequency that it can be hard to know what one can safely do/take while pregnant or nursing.
In the case of COVID vaccines, though, nearly 90% of babies who had to be hospitalized with COVID-19 had mothers who didn’t get the vaccine while they were pregnant.
And as for how common that is: babies too young to be vaccinated (so, under 6 months) had the highest covid hospitalization rate of any age group except people over 75.
Read in full: Here’s why getting a covid shot during pregnancy is important
Related: The Truth About Vaccines
Positive dieting
Adding things into one’s diet is a lot more fun than taking things out, is generally easier to sustain, and (as a general rule of thumb; there are exceptions of course) give the greatest differences in health outcomes.
This is perhaps most true of beans and pulses, which add many valuable vitamins, minerals, protein, and perhaps most importantly of all (single biggest factor in reducing heart disease risk), fiber.
Read in full: Adding beans and pulses can lead to improved shortfall nutrient intakes and a higher diet quality in American adults
Related: Intuitive Eating Might Not Be What You Think
Clearing out disordered thinking
Hoarding is largely driven by fear of loss, and this radical therapy tackles that at the root, by such means as rehearsing alternative outcomes of discarding through imagery rescripting, and examining the barriers to throwing things away—to break down those barriers one at a time.
Read in full: Hoarding disorder: sensory CBT treatment strategy shows promise
Related: When You Know What You “Should” Do (But Knowing Isn’t The Problem)
Superfluous
Fluoridated water may not be as helpful for the teeth as it used to be prior to about 1975. Not because it became any less effective per se, but because of the modern prevalence of fluoride-containing toothpastes, mouthwashes, etc rendering it redundant in more recent decades.
Read in full: Dental health benefits of fluoride in water may have declined, study finds
Related: Water Fluoridation, Atheroma, & More
Off-label?
With rising costs of living including rising healthcare costs, and increasing barriers to accessing in-person healthcare, it’s little wonder that many are turning to the gray market online to get their medications.
These websites typically use legal loopholes to sell prescription drugs to the public, by employing morally flexible doctors who are content to expediently rubber-stamp prescriptions upon request, on the basis of the patient having filled out a web form and checked boxes for their symptoms (and of course also having waived all rights of complaint or legal recourse).
However, some less scrupulous sorts are exploiting this market, to sell outright fake medications, using a setup that looks like a “legitimate” gray market website. Caveat emptor indeed.
Read in full: CDC warns of fake drug dangers from online pharmacies
Related: Are You Taking PIMs? Getting Off The Overmedication Train
A rising threat
In 2021 (we promise the paper was published only a few days ago!), the leading causes of death were:
- COVID-19
- Heart disease
- Stroke
…which latter represented a rising threat, likely in part due to the increase in the aging population.
Read in full: Stroke remains a leading cause of death globally, with increased risk linked to lifestyle factors
Related: 6 Signs Of Stroke (One Month In Advance)
Take care!
Share This Post
-
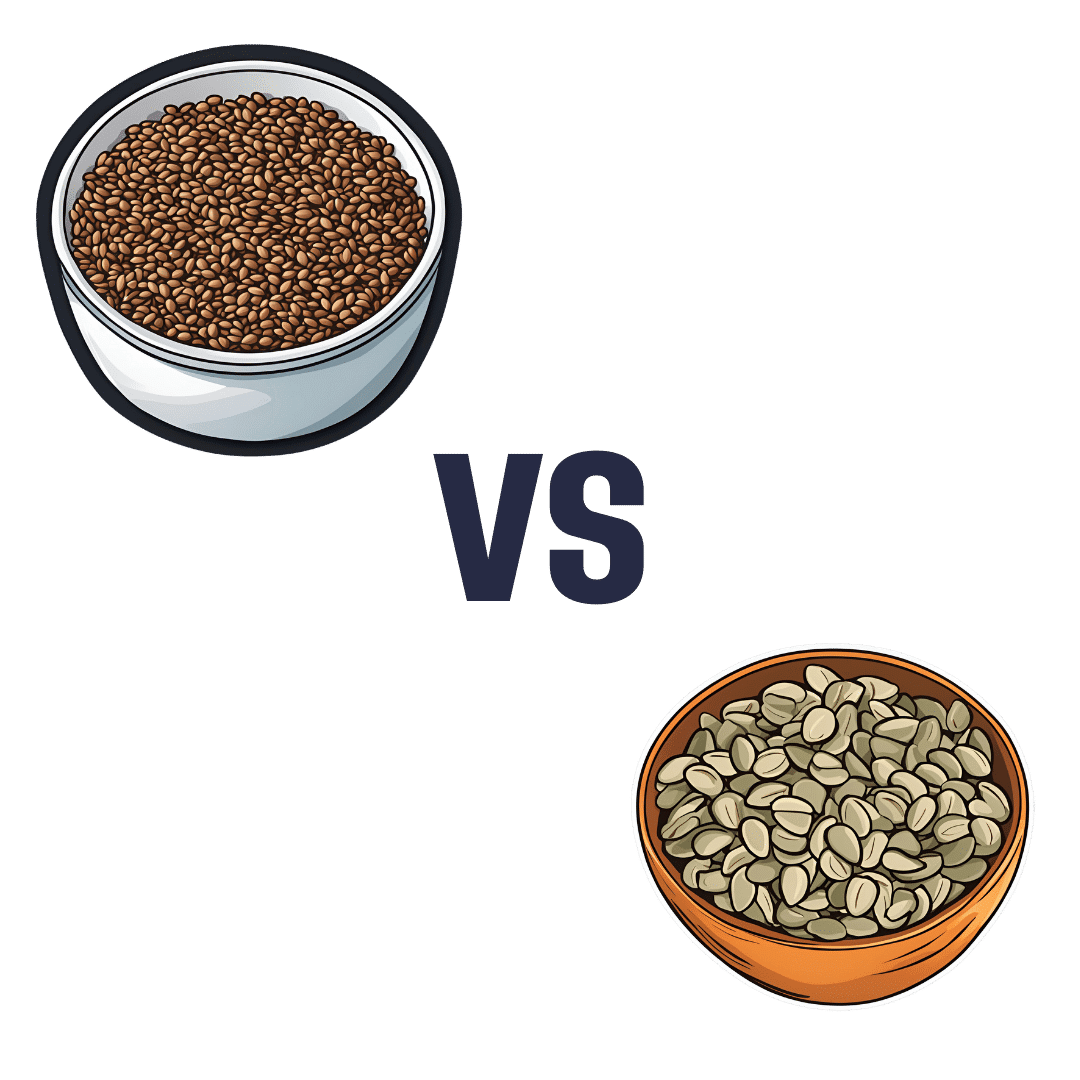
Flax Seeds vs Pumpkin Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing flax seeds to pumpkin seeds, we picked the flax.
Why?
Looking at the macros first, they are equal on protein, and flax seeds have a lot more fiber while pumpkin seeds have a lot more carbs. We’re going to prioritise fiber over carbs and call this a win for flax.
In terms of vitamins, flax seeds have a lot more of vitamins B1, B2, B3, B5, B6, B7, B9, C, E, K, and choline, while pumpkin seeds have a tiny bit more vitamin A. An easy win for flax here.
When it comes to minerals, flax has multiples more calcium, copper, iron, magnesium, manganese, phosphorus, and selenium, while pumpkin seeds have more zinc. Another win for flax.
Adding up the sections makes for a clear overall win for flax, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score? ← seeds count as plants!
Enjoy!
Share This Post
Related Posts
-
How worried should I be about cryptosporidiosis? Am I safe at the pool?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You might have heard of something called “cryptosporidiosis” recently, closely followed by warnings to stay away from your local swimming pool if you’ve had diarrhoea.
More than 700 cases of this gastrointestinal disease were reported in Queensland in January, which is 13 times more than in January last year. Just under 500 cases have been recorded in New South Wales this year to-date, while other states have similarly reported an increase in the number of cryptosporidiosis infections in recent months.
Cryptosporidiosis has been listed as a national notifiable disease in Australia since 2001.
But what exactly is it, and should we be worried?What causes cryptosporidiosis, and who is affected?
Cryptosporidiosis is the disease caused by the parasite Cryptosporidium, of which there are two types that can make us sick. Cryptosporidum hominis only affects humans and is the major cause of recent outbreaks in Australia, while Cryptosporidium parvum can also affect animals.
The infection is spread by spores called oocysts in the stools of humans and animals. When ingested, these oocysts migrate and mature in the small bowel. They damage the small bowel lining and can lead to diarrhoea, nausea, vomiting, fever and abdominal discomfort.
Most people develop symptoms anywhere from one to 12 days after becoming infected. Usually these symptoms resolve within two weeks, but the illness may last longer and can be severe in those with a weakened immune system.
Children and the elderly tend to be the most commonly affected. Cryptosporidiosis is more prevalent in young children, particularly those under five, but the disease can affect people of any age.
A number of public pools have been closed lately due to cryptosporidiosis outbreaks.
LBeddoe/ShutterstockSo how do we catch it?
Most major outbreaks of cryptosporidiosis have been due to people drinking contaminated water. The largest recorded outbreak occurred in Milwaukee in 1993 where 403,000 people were believed to have been infected.
Cryptosporidium oocysts are very small in size and in Milwaukee they passed through the filtration system of one of the water treatment plants undetected, infecting the city’s water supply. As few as ten oocysts can cause infection, making it possible for contaminated drinking water to affect a very large number of people.
Four days after infection a person with cryptosporidiosis can shed up to ten billion oocysts into their stool a day, with the shedding persisting for about two weeks. This is why one infected person in a swimming pool can infect the entire pool in a single visit.
Cryptosporidium oocysts excreted in the faeces of infected humans and animals can also reach natural bodies of water such as beaches, rivers and lakes directly through sewer pipes or indirectly such as in manure transported with surface runoff after heavy rain.
One study which modelled Cryptosporidium concentrations in rivers around the world estimated there are anywhere from 100 to one million oocysts in a litre of river water.
In Australia, cryptosporidiosis outbreaks tend to occur during the late spring and early summer periods when there’s an increase in recreational water activities such as swimming in natural water holes, water catchments and public pools. We don’t know exactly why cases have seen such a surge this summer compared to other years, but we know Cryptosporidium is very infectious.
Oocysts have been found in foods such as fresh vegetables and seafood but these are not common sources of infection in Australia.
What about chlorine?
Contrary to popular belief, chlorine doesn’t kill off all infectious microbes in a swimming pool. Cryptosporidium oocysts are hardy, thick-walled and resistant to chlorine and acid. They are not destroyed by chlorine at the normal concentrations found in swimming pools.
We also know oocysts can be significantly protected from the effects of chlorine in swimming pools by faecal material, so the presence of even small amounts of faecal matter contaminated with Cryptosporidium in a swimming pool would necessitate closure and a thorough decontamination.
Young children and in particular children in nappies are known to increase the potential for disease transmission in recreational water. Proper nappy changing, frequent bathroom breaks and showering before swimming to remove faecal residue are helpful ways to reduce the risk.
Cryptosporidium can spread in other bodies of water, not just swimming pools.
Yulia Simonova/ShutterstockSome sensible precautions
Other measures you can take to reduce yours and others’ risk of cryptosporidiosis include:
- avoid swimming in natural waters such as rivers and creeks during and for at least three days after heavy rain
- avoid swimming in beaches for at least one day after heavy rain
- avoid drinking untreated water such as water from rivers or springs. If you need to drink untreated water, boiling it first will kill the Cryptosporidium
- avoid swallowing water when swimming if you can
- if you’ve had diarrhoea, avoid swimming for at least two weeks after it has resolved
- avoid sharing towels or linen for at least two weeks after diarrhoea has resolved
- avoid sharing, touching or preparing food that other people may eat for at least 48 hours after diarrhoea has resolved
- wash your hands with soap and water after going to the bathroom or before preparing food (Cryptosporidium is not killed by alcohol gels and sanitisers).
Not all cases of diarrhoea are due to cryptosporidiosis. There are many other causes of infectious gastroenteritis and because the vast majority of the time recovery is uneventful you don’t need to see a doctor unless very unwell. If you do suspect you may have cryptosporidiosis you can ask your doctor to refer you for a stool test.
Vincent Ho, Associate Professor and clinical academic gastroenterologist, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
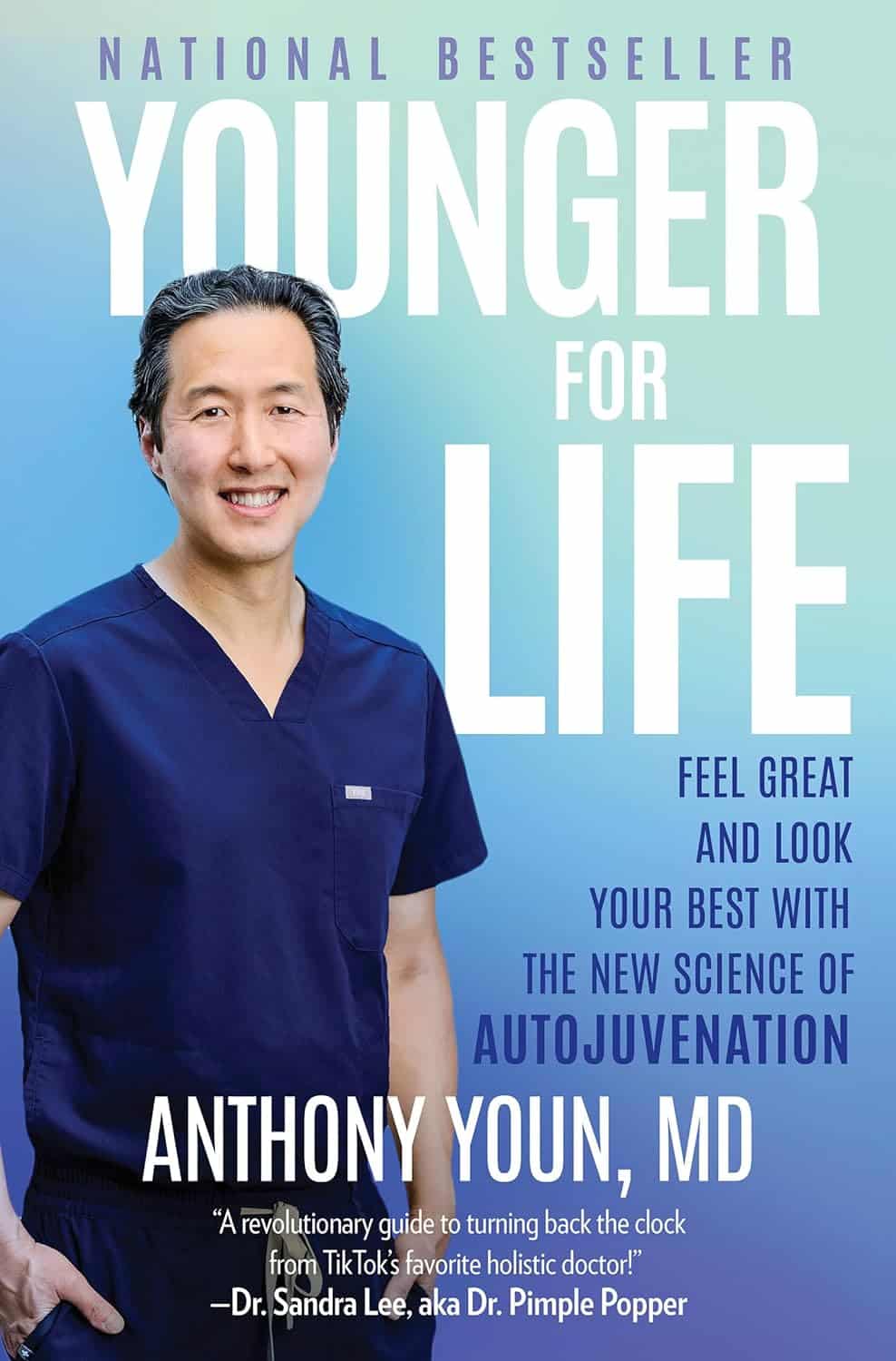
Younger For Life – by Dr. Anthony Youn
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed anti-aging books before, so what makes this one different? Mostly, it’s the very practical focus.
Which is not to say there’s not also good science in here; there is. But the focus is on what everything means for the reader, not what happened with a certain cohort of lab mice. Instead, he looks at the causes of aging, the process of aging, and what interventions to implement to address those, and reverse many of them.
Some parts are more general lifestyle interventions that 10almonds readers will know well already, but other parts are very specific advices, protocols, and regimes; in particular his skincare section is well worth reading. As for nutrition, there’s even a respectable recipes section, so this book does have it all!
The final section of the book is dedicated to plastic surgeries (the author is a plastic surgeon who believes that most people should not need those, and would do well to stick to the advices in the rest of the book). We suspect this last part of the book will be of least interest to 10almonds readers.
Bottom line: if you’re of the view that getting older should come with as little as possible physical deterioration along the way, then this book can help a lot with that.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Yes, adults can develop food allergies. Here are 4 types you need to know about
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you didn’t have food allergies as a child, is it possible to develop them as an adult? The short answer is yes. But the reasons why are much more complicated.
Preschoolers are about four times more likely to have a food allergy than adults and are more likely to grow out of it as they get older.
It’s hard to get accurate figures on adult food allergy prevalence. The Australian National Allergy Council reports one in 50 adults have food allergies. But a US survey suggested as many as one in ten adults were allergic to at least one food, with some developing allergies in adulthood.
What is a food allergy
Food allergies are immune reactions involving immunoglobulin E (IgE) – an antibody that’s central to triggering allergic responses. These are known as “IgE-mediated food allergies”.
Food allergy symptoms that are not mediated by IgE are usually delayed reactions and called food intolerances or hypersensitivity.
Food allergy symptoms can include hives, swelling, difficulty swallowing, vomiting, throat or chest tightening, trouble breathing, chest pain, rapid heart rate, dizziness, low blood pressure or anaphylaxis.
Symptoms include hives. wisely/Shutterstock IgE-mediated food allergies can be life threatening, so all adults need an action management plan developed in consultation with their medical team.
Here are four IgE-mediated food allergies that can occur in adults – from relatively common ones to rare allergies you’ve probably never heard of.
1. Single food allergies
The most common IgE-mediated food allergies in adults in a US survey were to:
- shellfish (2.9%)
- cow’s milk (1.9%)
- peanut (1.8%)
- tree nuts (1.2%)
- fin fish (0.9%) like barramundi, snapper, salmon, cod and perch.
In these adults, about 45% reported reacting to multiple foods.
This compares to most common childhood food allergies: cow’s milk, egg, peanut and soy.
Overall, adult food allergy prevalence appears to be increasing. Compared to older surveys published in 2003 and 2004, peanut allergy prevalence has increased about three-fold (from 0.6%), while tree nuts and fin fish roughly doubled (from 0.5% each), with shellfish similar (2.5%).
While new adult-onset food allergies are increasing, childhood-onset food allergies are also more likely to be retained into adulthood. Possible reasons for both include low vitamin D status, lack of immune system challenges due to being overly “clean”, heightened sensitisation due to allergen avoidance, and more frequent antibiotic use.
Some adults develop allergies to cow’s milk, while others retain their allergy from childhood. Sarah Swinton/Unsplash 2. Tick-meat allergy
Tick-meat allergy, also called α-Gal syndrome or mammalian meat allergy, is an allergic reaction to galactose-alpha-1,3-galactose, or α-Gal for short.
Australian immunologists first reported links between α-Gal syndrome and tick bites in 2009, with cases also reported in the United States, Japan, Europe and South Africa. The US Centers for Disease Control estimates about 450,000 Americans could be affected.
The α-Gal contains a carbohydrate molecule that is bound to a protein molecule in mammals.
The IgE-mediated allergy is triggered after repeated bites from ticks or chigger mites that have bitten those mammals. When tick saliva crosses into your body through the bite, antibodies to α-Gal are produced.
When you subsequently eat foods that contain α-Gal, the allergy is triggered. These triggering foods include meat (lamb, beef, pork, rabbit, kangaroo), dairy products (yoghurt, cheese, ice-cream, cream), animal-origin gelatin added to gummy foods (jelly, lollies, marshmallow), prescription medications and over-the counter supplements containing gelatin (some antibiotics, vitamins and other supplements).
Tick-meat allergy reactions can be hard to recognise because they’re usually delayed, and they can be severe and include anaphylaxis. Allergy organisations produce management guidelines, so always discuss management with your doctor.
3. Fruit-pollen allergy
Fruit-pollen allergy, called pollen food allergy syndrome, is an IgE-mediated allergic reaction.
In susceptible adults, pollen in the air provokes the production of IgE antibodies to antigens in the pollen, but these antigens are similar to ones found in some fruits, vegetables and herbs. The problem is that eating those plants triggers an allergic reaction.
The most allergenic tree pollens are from birch, cypress, Japanese cedar, latex, grass, and ragweed. Their pollen can cross-react with fruit and vegetables, including kiwi, banana, mango, avocado, grapes, celery, carrot and potato, and some herbs such as caraway, coriander, fennel, pepper and paprika.
Fruit-pollen allergy is not common. Prevalence estimates are between 0.03% and 8% depending on the country, but it can be life-threatening. Reactions range from itching or tingling of lips, mouth, tongue and throat, called oral allergy syndrome, to mild hives, to anaphylaxis.
4. Food-dependent, exercise-induced food allergy
During heavy exercise, the stomach produces less acid than usual and gut permeability increases, meaning that small molecules in your gut are more likely to escape across the membrane into your blood. These include food molecules that trigger an IgE reaction.
If the person already has IgE antibodies to the foods eaten before exercise, then the risk of triggering food allergy reactions is increased. This allergy is called food-dependent exercise-induced allergy, with symptoms ranging from hives and swelling, to difficulty breathing and anaphylaxis.
This type of allergy is extremely rare. Ben O’Sullivan/Unsplash Common trigger foods include wheat, seafood, meat, poultry, egg, milk, nuts, grapes, celery and other foods, which could have been eaten many hours before exercising.
To complicate things even further, allergic reactions can occur at lower levels of trigger-food exposure, and be more severe if the person is simultaneously taking non-steroidal inflammatory medications like aspirin, drinking alcohol or is sleep-deprived.
Food-dependent exercise-induced allergy is extremely rare. Surveys have estimated prevalence as between one to 17 cases per 1,000 people worldwide with the highest prevalence between the teenage years to age 35. Those affected often have other allergic conditions such as hay fever, asthma, allergic conjunctivitis and dermatitis.
Allergies are a growing burden
The burden on physical health, psychological health and health costs due to food allergy is increasing. In the US, this financial burden was estimated as $24 billion per year.
Adult food allergy needs to be taken seriously and those with severe symptoms should wear a medical information bracelet or chain and carry an adrenaline auto-injector pen. Concerningly, surveys suggest only about one in four adults with food allergy have an adrenaline pen.
If you have an IgE-mediated food allergy, discuss your management plan with your doctor. You can also find more information at Allergy and Anaphylaxis Australia.
Clare Collins, Laureate Professor in Nutrition and Dietetics, University of Newcastle
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: