Increase in online ADHD diagnoses for kids poses ethical questions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In 2020, in the midst of a pandemic, clinical protocols were altered for Ontario health clinics, allowing them to perform more types of care virtually. This included ADHD assessments and ADHD prescriptions for children – services that previously had been restricted to in-person appointments. But while other restrictions on virtual care are back, clinics are still allowed to virtually assess children for ADHD.
This shift has allowed for more and quicker diagnoses – though not covered by provincial insurance (OHIP) – via a host of newly emerging private, for-profit clinics. However, it also has raised significant ethical questions.
It solves an equity issue in terms of rural access to timely assessments, but does it also create new equity issues as a privatized service?
Is it even feasible to diagnose a child for a condition like ADHD without meeting that child in person?
And as rates of ADHD diagnosis continue to rise, should health regulators re-examine the virtual care approach?
Ontario: More prescriptions, less regulation
There are numerous for-profit clinics offering virtual diagnoses and prescriptions for childhood ADHD in Ontario. These include KixCare, which does not offer the option of an in-person assessment. Another clinic, Springboard, makes virtual appointments available within days, charging around $2,600 for assessments, which take three to four hours. The clinic offers coaching and therapy at an additional cost, also not covered by OHIP. Families can choose to continue to visit the clinic virtually during a trial stage with medications, prescribed by a doctor in the clinic who then sends prescribing information back to the child’s primary care provider.
For-profit clinics like these are departing from Canada’s traditional single-payer health care model. By charging patients out-of-pocket fees for services, the clinics are able to generate more revenue because they are working outside of the billing standards for OHIP, standards that set limits on the maximum amount doctors can earn for providing specific services. Instead many services are provided by non-physician providers, who are not limited by OHIP in the same way.
Need for safeguards
ADHD prescriptions rose during the pandemic in Ontario, with women, people of higher income and those aged 20 to 24 receiving the most new diagnoses, according to research published in January 2024 by a team including researchers from the Centre for Addictions and Mental Health and Holland Bloorview Children’s Hospital. There may be numerous reasons for this increase but could the move to virtual care have been a factor?
Ontario psychiatrist Javeed Sukhera, who treats both children and adults in Canada and the U.S., says virtual assessments can work for youth with ADHD, who may receive treatment quicker if they live in remote areas. However, he is concerned that as health care becomes more privatized, it will lead to exploitation and over-diagnosis of certain conditions.
“There have been a lot of profiteers who have tried to capitalize on people’s needs and I think this is very dangerous,” he said. “In some settings, profiteering companies have set up systems to offer ADHD assessments that are almost always substandard. This is different from not-for-profit setups that adhere to quality standards and regulatory mechanisms.”
Sukhera’s concerns recall the case of Cerebral Inc., a New York state-based virtual care company founded in 2020 that marketed on social media platforms including Instagram and TikTok. Cerebral offered online prescriptions for ADHD drugs among other services and boasted more than 200,000 patients. But as Dani Blum reported in the New York Times, Cerebral was accused in 2023 of pressuring doctors on staff to prescribe stimulants and faced an investigation by state prosecutors into whether it violated the U.S. Controlled Substances Act.
“At the start of the pandemic, regulators relaxed rules around medical prescription of controlled substances,” wrote Blum. “Those changes opened the door for companies to prescribe and market drugs without the protocols that can accompany an in-person visit.”
Access increased – but is it equitable?
Virtual care has been a necessity in rural areas in Ontario since well before the pandemic, although ADHD assessments for children were restricted to in-person appointments prior to 2020.
But ADHD assessment clinics that charge families out-of-pocket for services are only accessible to people with higher incomes. Rural families, many of whom are low income, are unable to afford thousands for private assessments, let alone the other services upsold by providers. If the private clinic/virtual care trend continues to grow unchecked, it may also attract doctors away from the public model of care since they can bill more for services. This could further aggravate the gap in care that lower income people already experience.
This could further aggravate the gap in care that lower income people already experience.
Sukhera says some risks could be addressed by instituting OHIP coverage for services at private clinics (similar to private surgical facilities that offer mixed private/public coverage), but also with safeguards to ensure that profits are reinvested back into the health-care system.
“This would be especially useful for folks who do not have the income, the means to pay out of pocket,” he said.
Concerns of misdiagnosis and over-prescription
Some for-profit companies also benefit financially from diagnosing and issuing prescriptions, as has been suggested in the Cerebral case. If it is cheaper for a clinic to do shorter, virtual appointments and they are also motivated to diagnose and prescribe more, then controls need to be put in place to prevent misdiagnosis.
The problem of misdiagnosis may also be related to the nature of ADHD assessments themselves. University of Strathclyde professor Matthew Smith, author of Hyperactive: The Controversial History of ADHD, notes that since the publication of Diagnostic and Statistical Manual of Mental Disorders in 1980, assessment has typically involved a few hours of parents and patients providing their subjective perspectives on how they experience time, tasks and the world around them.
“It’s often a box-ticking exercise, rather than really learning about the context in which these behaviours exist,” Smith said. “The tendency has been to use a list of yes/no questions which – if enough are answered in the affirmative – lead to a diagnosis. When this is done online or via Zoom, there is even less opportunity to understand the context surrounding behaviour.”
Smith cited a 2023 BBC investigation in which reporter Rory Carson booked an in-person ADHD assessment at a clinic and was found not to have the condition, then had a private online assessment – from a provider on her couch in a tracksuit – and was diagnosed with ADHD after just 45 minutes, for a fee of £685.
What do patients want?
If Canadian regulators can effectively tackle the issue of privatization and the risk of misdiagnosis, there is still another hurdle: not every youth is willing to take part in virtual care.
Jennifer Reesman, a therapist and Training Director for Neuropsychology at the Chesapeake Center for ADHD, Learning & Behavioural Health in Maryland, echoed Sukhera’s concerns about substandard care, cautioning that virtual care is not suitable for some of her young clients who had poor experiences with online education and resist online health care. It can be an emotional issue for pediatric patients who are managing their feelings about the pandemic experience.
“We need to respect what their needs are, not just the needs of the provider,” says Reesman.
In 2020, Ontario opted for virtual care based on the capacity of our health system in a pandemic. Today, with a shortage of doctors, we are still in a crisis of capacity. The success of virtual care may rest on how engaged regulators are with equity issues, such as waitlists and access to care for rural dwellers, and how they resolve ethical problems around standards of care.
Children and youth are a distinct category, which is why we had restrictions on virtual ADHD diagnosis prior to the pandemic. A question remains, then: If we could snap our fingers and have the capacity to provide in-person ADHD care for all children, would we? If the answer to that question is yes, then how can we begin to build our capacity?
This article is republished from healthydebate under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Continuous Glucose Monitors Without Diabetes: Pros & Cons
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The “Glucose Goddess”, biochemist Jessie Inchauspé, gives us the low-down:
Knowledge is power (but watch out)
A continuous glucose monitor (CGM) is a device that continually monitors glucose levels, without the need to stab one’s finger every few hours to test blood.
It was designed for diabetics, especially for those with Type 1 Diabetes, where around-the-clock monitoring is necessary for appropriate insulin dosing.
For non-diabetics, they can be a good way of learning what our body’s response to various foods and activities is like, the better to be able to tweak our habits to avoid undue glucose spikes (which are harmful for our pancreas, liver, heart, brain, kidneys, and more).
How it works: there’s a sensor that sits on the arm (or elsewhere, but the arm is a popular placement) with a little probe that goes under the skin. It’s applied using a device that inserts it automatically using a needle (you only need to press a button, you don’t need to guide the needle yourself); the needle then retracts, leaving the soft, flexible probe in place. Having been attached, that sensor can now stay in place for 2 weeks (usually; depends on brand, but for example FreeStyle Libre, the most popular brand, the sensors last 2 weeks), and yes, it’s fine to bathe/shower/etc with it. When you want an update from your CGM, you scan it with your phone (or you can buy a dedicated reader, but that is more expensive and unnecessary), and it uploads the data since your last scan.
Pros: it’s convenient and gives a lot of data, so even if you only use it for a short period of time (for example, a month) you can get a very good idea of what affects your blood sugar levels and how. Also, because of the constant nature of the monitoring, it helps avoid accidental sample bias of the kind that can occur with manual testing, by testing a little too soon or too late, and missing a spike/dip.
Cons: it can be expensive, depending on where you live and what options are available for you locally, so you might not want to do it long-term (since that would require buying two sensors per month). It’s also, for all its wealth of data, slightly less accurate than fingerprick testing—that’s because it takes an interstitial reading instead of directly from the blood. For this reason, if you test both ways, you may find a discrepancy of about 3mg/dL. Given that the healthy range is about 70–140mg/dL, a discrepancy of 3mg/dL is probably not going to be important, but it is a thing to mention can (and probably will) happen.
Patterns to bear in mind (with any kind of blood sugar monitoring):
- Dawn phenomenon: a natural glucose rise upon waking.
- Exercise-induced spikes (normal due to energy demands).
- Fat in meals slowing glucose absorption.
- Different foods can sometimes cause a double-wave after dinner (because glucose from different foods is absorbed differently, and/or different foods affect insulin response independent of glucose)
- Steep, rapid spikes that are more harmful than gradual, sustained increases.
- Vitamin C spikes: temporary chemical interference with the sensor, not actual glucose rises.
- Nighttime glucose dips (often false readings caused by sleeping position).
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
10 Ways To Balance Blood Sugars
Take care!
Share This Post
-
8 Signs Of High Cortisol & How To Reverse “Cortisol Face”
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Shereene Idriss has insights about the facial features that might indicate chronically elevated cortisol levels, and what to do about same:
At face value
Dr. Idriss notes that for most people, this should not be cause for undue concern, although hypercortisolism can also be associated with genetic disorders such as Cushing’s syndrome, as well as prolonged use of certain medication, or the presence of certain tumors. As well as facial swelling, hypercortisolism can also result in other physical changes like acne, weight gain, skin thinning, stretch marks, infections, and hair loss.
As for what to do about it, she recommends addressing lifestyle factors like poor sleep, unhealthy diet, alcohol consumption, and lack of hydration to reduce facial puffiness related to stress. Diet suggestions include incorporating foods rich in magnesium, vitamin C, and omega-3s, such as leafy greens, fatty fish, nuts and seeds, and berries.
She also suggests some supplements to consider, such as ashwagandha, magnesium, omega-3s, and/or l-theanine, but you might want to speak to your doctor/pharmacist to check in case of contraindications per any other conditions you may have, or medications you may be on.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Lower Your Cortisol! (Here’s Why & How)
- Ashwagandha: The Root of All Even-Mindedness?
- L-Theanine: What’s The Tea?
Take care!
Share This Post
-
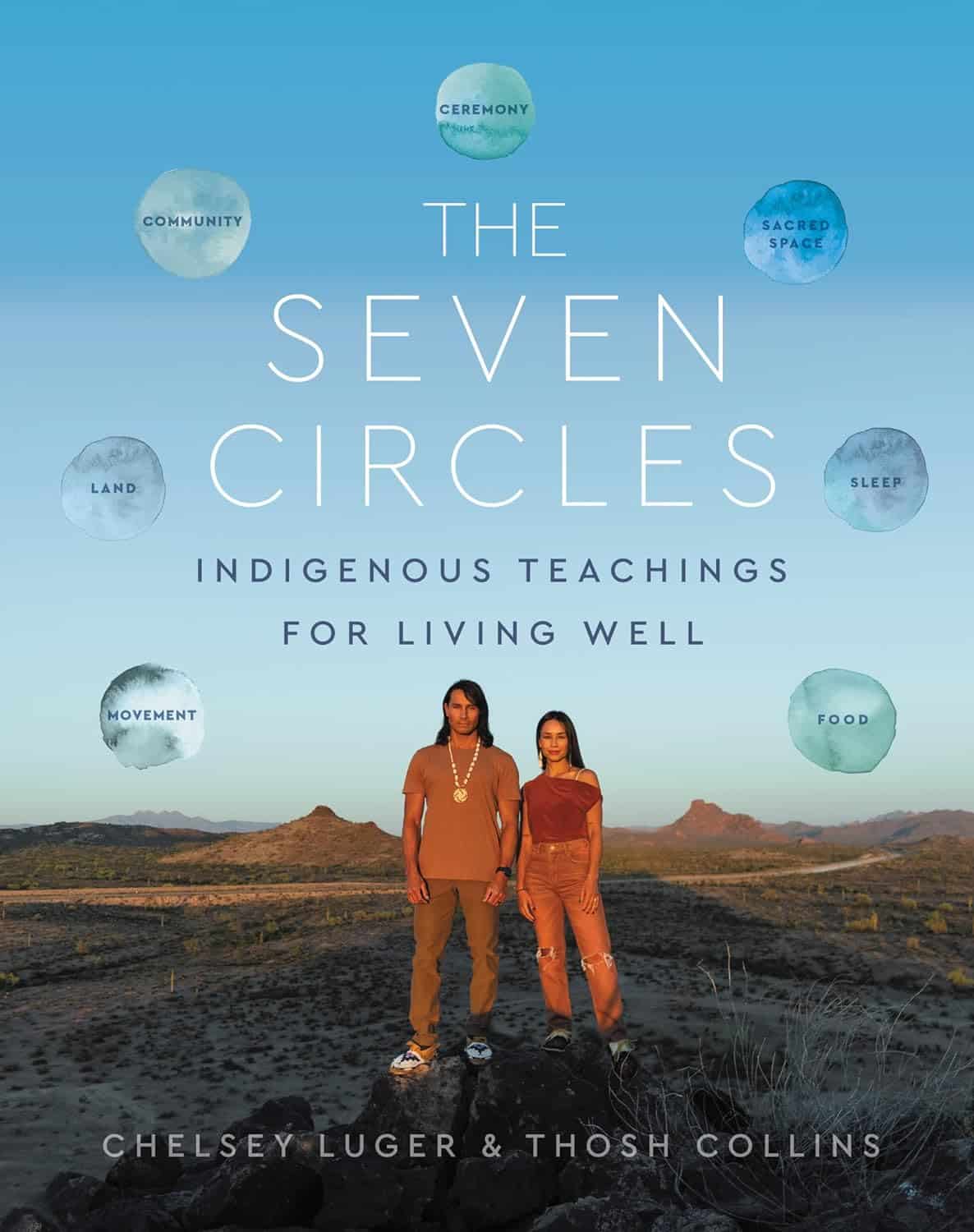
The Seven Circles – by Chelsey Luger & Thosh Collins
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At first glance, this can seem like an unscientific book—you won’t find links to studies in this one, for sure! However, if we take a look at the seven circles in question, they are:
- Food
- Movement
- Sleep
- Ceremony
- Sacred Space
- Land
- Community
Regular 10almonds readers may notice that these seven items contain five of the things strongly associated with the “supercentenarian Blue Zones”. (If you are wondering why Native American reservations are not Blue Zones, the answer there lies less in health science and more in history and sociology, and what things have been done to a given people).
The authors—who are Native American, yes—present in one place a wealth of knowledge and know-how. Not even just from their own knowledge and their own respective tribes, but gathered from other tribes too.
Perhaps the strongest value of this book to the reader is in the explanation of noting the size of each of those circles, how they connect with each other, and providing a whole well-explained system for how we can grow each of them in harmony with each other.
Or to say the same thing in sciencey terms: how to mindfully improve integrated lifestyle factors synergistically for greater efficacy and improved health-adjusted quality-of-life years.
Bottom line: if you’re not averse to something that mostly doesn’t use sciencey terms of have citations to peer-reviewed studies peppered through the text, then this book has wisdom that’s a) older than the pyramids of Giza, yet also b) highly consistent with our current best science of Blue Zone healthy longevity.
Share This Post
Related Posts
-
Beetroot Juice & Caffeine Work Better Than Either Alone
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Beetroot has many beneficial properties, which we’ve written about before:
Beetroot For More Than Just Your Blood Pressure
…and as for caffeine, it’s a mixed bag but for most people, the benefits of moderate caffeine use outweigh the risks:
Caffeine: Cognitive Enhancer Or Brain-Wrecker?
Now, caffeine’s less desirable effects can be mitigated somewhat by pairing it with l-theanine, as we’ve also discussed before:
L-Theanine: What’s The Tea? ← l-theanine also has many wonderful properties of its own, aside from its complementary effects when taken alongside caffeine
So, what’s the deal with caffeine and beetroot juice?
A performance-enhancing balancing act
Caffeine raises blood pressure, while beetroot lowers it, but there’s a lot more to it than that.
Researchers looked into the effects of caffeine and beetroot juice, together or separately, on athletic performance (in a 1000m run) in non-athletes.
They found:
- Caffeine alone enhanced second-run performance but not the first.
- Beetroot juice alone improved first-run performance but led to a performance decline after recovery.
- The caffeine + BJ combo resulted in the best initial and repeated 1000m run performances.
Specifically, they also noted:
- Caffeine alone caused higher blood lactate levels post-exercise.
- Beetroot juice increased muscle oxygenation by 25% during runs.
- The caffeine + BJ combo led to the highest post-exercise heart rate improvements.
You can read the paper in full here:
Caffeine and Beetroot Juice Optimize 1,000-m Performance: Shapley Additive Explanations Analysis
Now, maybe you don’t have a 1000m run to do, let alone multiple ones back-to-back, but most of us could sometimes do with an energy boost during the day, and this seems like an excellent way to get it.
That said, caffeine timing can be important too; midday is generally the best time for it, because:
- of course it should not be too late in the day, because the elimination half-life of caffeine (4–8 hours to eliminate just half of the caffeine, depending on genes, call it 6 hours as an average though honestly for most people it will either be 4 or 8, not 6) is such that it can easily interfere with sleep for most people
- because caffeine is an adenosine blocker, not an adenosine inhibitor, taking caffeine in the morning means either there’s no adenosine to block, or it’ll just “save” that adenosine for later, i.e. when the caffeine is eliminated, then the adenosine will kick in, meaning that your morning sleepiness has now been deferred to the afternoon, rather than eliminated.
Another reminder that caffeine is the “payday loan” of energy. So, midday it is. No morning sleepiness to defer, and yet also not so late as to interfere with sleep.
See also: Calculate (And Enjoy) The Perfect Night’s Sleep
Want to learn more?
Check out:
The Best Form Of Sugar For Energy During Exercise
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cashew Nuts vs Macadamia Nuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cashews to macadamias, we picked the cashews.
Why?
In terms of macros, cashews have more than 2x the protein, while macadamias have nearly 2x the fat. The fats are mostly monounsaturated, so it’s still healthy in moderation, but still, we’re going to prize the protein over it and call this category a nominal win for cashews.
When it comes to vitamins, things are fairly even; cashews have more of vitamins B5, B6, B9, and E, while macadamias have more of vitamins B1, B2, B3, and C.
In the category of minerals, cashews take the clear lead; cashews have more copper, iron, magnesium, phosphorus, potassium, selenium, and zinc, while macadamias have more calcium and manganese.
In short, enjoy both (as macadamias have their benefits too), but cashews win in total nutrient density.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Stop Self-Sabotage – by Dr. Judy Ho
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of books of this genre identify one particular kind of self-sabotage, for example, they might pick one out of:
- Bad habits
- Limiting self-beliefs
- Poor goal-setting
- Procrastination
…etc, slap a quick fix on whatever they chose to focus on, and call it a day. Not so with Dr. Ho!
Here we have a much more comprehensive approach to tackling the problem of unintentional self-sabotage. With a multi-vector method, of which all angles can be improved simultaneously, it becomes much less like “whack-a-mole”… And much more like everything actually getting into order and staying that way.
The main approach here is CBT, but far beyond what most pop-psychology CBT books go for, with more techniques and resources.
On which note…
There are many great exercises that Dr. Ho recommends we do while reading… So you might want to get a nice notebook alongside this book if you don’t already have one! And what is more inspiring of optimism than a new notebook?
Bottom line: this is a great, well-organized guide to pruning the “why am I still doing this to myself?” aspects out of your life for a much more intentional, purposeful, effective way of living.
Click here to check it out on Amazon today, and stop sabotaging yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: