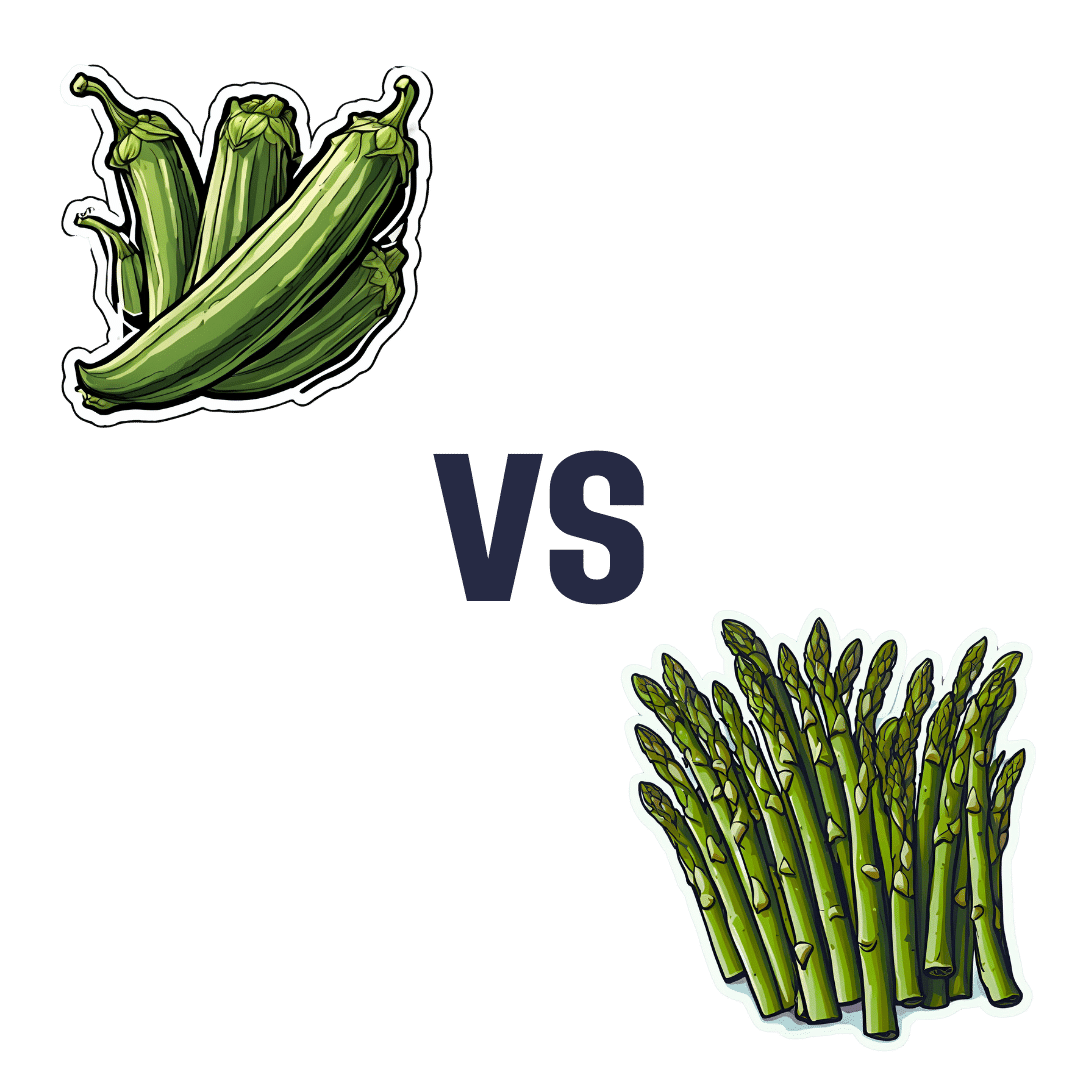
Okra vs Asparagus – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing okra to asparagus, we picked the okra.
Why?
Both are great! But…
In terms of macros, okra has more fiber and carbs, making it the more nutrient dense option, for a similar glycemic index.
In the category of vitamins, okra has more of vitamins B1, B3, B6, B9, and C, while asparagus has more of vitamins B2, B5, E, K, and choline, making for a 5:5 tie, with similar margins of difference too. Thus, definitely a tie on vitamins.
When it comes to minerals, okra has more calcium, magnesium, manganese, phosphorus, potassium, and zinc, while asparagus has more copper, iron, and selenium. An easy 6:3 win for okra.
Both of these on-the-cusp-of-being-pungent vegetables have beneficial antioxidant polyphenols (especially various forms of quercetin), but okra has more.
Adding up the sections makes for an overall win for okra, but by all means enjoy either both; diversity is good!
Want to learn more?
You might like to read:
Enjoy Bitter/Astringent/Pungent Foods For Your Heart & Brain
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Olfactory Training, Better
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Anosmia, by any other name…
The loss of the sense of smell (anosmia) is these days well-associated with COVID and Long-COVID, but also can simply come with age:
National Institute of Aging | How Smell & Taste Change With Age
…although it can also be something else entirely:
❝Another possibility is a problem with part of the nervous system responsible for smell.
Some studies have suggested that loss of smell could be an early sign of a neurodegenerative disease, such as Alzheimer’s or Parkinson’s disease.
However, a recent study of 1,430 people (average age about 80) showed that 76% of people with anosmia had normal cognitive function at the study’s end.❞
Read more: Harvard Health | Is it normal to lose my sense of smell as I age?
We’d love to look at and cite the paper that they cite, but they didn’t actually provide a source. We did find some others, though:
❝Olfactory capacity declines with aging, but increasing evidence shows that smell dysfunction is one of the early signs of prodromal neurodegenerative diseases such as Alzheimer’s and Parkinson’s disease.
The loss of smell is considered a clinical sign of early-stage disease and a marker of the disease’s progression and cognitive impairment.❞
Read more: Neurons, Nose, and Neurodegenerative Diseases: Olfactory Function and Cognitive Impairment
What’s clear is the association; what’s not clear is whether one worsens the other, and what causal role each might play. However, the researchers conclude that both ways are possible, including when there is another, third, underlying potential causal factor:
❝Ongoing studies on COVID-19 anosmia could reveal new molecular aspects unexplored in olfactory impairments due to neurodegenerative diseases, shedding a light on the validity of smell test predictivity of cognitive dementia.
The neuroepithelium might become a new translational research target (Neurons, Nose, and Neurodegenerative diseases) to investigate alternative approaches for intranasal therapy and the treatment of brain disorders. ❞
~ Ibid.
Another study explored the possible mechanisms of action, and found…
❝Olfactory impairment was significantly associated with increased likelihoods of MCI, amnestic MCI, and non-amnestic MCI.
In the subsamples, anosmia was significantly associated with higher plasma total tau and NfL concentrations, smaller hippocampal and entorhinal cortex volumes, and greater WMH volume, and marginally with lower AD-signature cortical thickness.
These results suggest that cerebral neurodegenerative and microvascular lesions are common neuropathologies linking anosmia with MCI in older adults❞
- MCI = Mild Cognitive Impairment
- NfL = Neurofilament Light [Chain]
- WMH = White Matter Hyperintensity
- AD =Alzheimer’s Disease
Read more: Anosmia, mild cognitive impairment, and biomarkers of brain aging in older adults
How to act on this information
You may be wondering, “this is fascinating and maybe even a little bit frightening, but how is this Saturday’s Life Hacks?”
We wanted to set up the “why” before getting to the “how”, because with a big enough “why”, it’s much easier to find the motivation to act on the “how”.
Test yourself
Or more conveniently, you and a partner/friend/relative can test each other.
Simply do like a “blind taste testing”, but for smell. Ideally these will be a range of simple and complex odors, and commercially available smell test kits will provide these, if you don’t want to make do with random items from your kitchen.
If you’d like to use a clinical diagnostic tool, you can check out:
Clinical assessment of patients with smell and taste disorders
…and especially, this really handy diagnostic flowchart:
Algorithm of evaluation of a patient who has olfactory loss
Train yourself
“Olfactory training” has been the got-to for helping people to regain their sense of smell after losing it due to COVID.
In simple terms, this means simply trying to smell things that “should” have a distinctive odor, and gradually working up one’s repertoire of what one can smell.
You can get some great tips here:
AbScent | Useful Insights Into Smell Training
Hack your training
An extra trick was researched deeply in a recent study which found that multisensory integration helped a) initially regain the ability to smell things and b) maintain that ability later without the cross-sensory input.
What that means: you will more likely be able to smell lemon while viewing the color yellow, and most likely of all to be able to smell lemon while actually holding and looking at a slice of lemon. Having done this, you’re more likely to be able to smell (and distinguish) the odor of lemon later in a blind smell test.
In other words: with this method, you may be able to cut out many months of frustration of trying and failing to smell something, and skip straight to the “re-adding specific smells to my brain’s olfactory database” bit.
Read the study: Olfactory training: effects of multisensory integration, attention towards odors and physical activity
Or if you prefer, here’s a pop-science article based on that:
One in twenty people has no sense of smell—here’s how they might get it back
Take care!
Share This Post
-
Protein: How Much Do We Need, Really?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mythbusting Protein!
Yesterday, we asked you for your policy on protein consumption. The distribution of responses was as follows:
- A marginal majority (about 55%) voted for “Protein is very important, but we can eat too much of it”
- A large minority (about 35%) voted for “We need lots of protein; the more, the better!”
- A handful (about 4%) voted for “We should go as light on protein as possible”
- A handful (6%) voted for “If we don’t eat protein, our body will create it from other foods”
So, what does the science say?
If we don’t eat protein, our body will create it from other foods: True or False?
Contingently True on an absurd technicality, but for all practical purposes False.
Our body requires 20 amino acids (the building blocks of protein), 9 of which it can’t synthesize and absolutely must get from food. Normally, we get those amino acids from protein in our diet, and we can also supplement them by buying amino acid supplements.
Specifically, we require (per kg of bodyweight) a daily average of:
- Histidine: 10 mg
- Isoleucine: 20 mg
- Leucine: 39 mg
- Lysine: 30 mg
- Methionine: 10.4 mg
- Phenylalanine*: 25 mg
- Threonine: 15 mg
- Tryptophan: 4 mg
- Valine: 26 mg
*combined with the non-essential amino acid tyrosine
Source: Protein and Amino Acid Requirements In Human Nutrition: WHO Technical Report
However, to get the requisite amino acid amounts, without consuming actual protein, would require gargantuan amounts of supplementation (bearing in mind bioavailability will never be 100%, so you’ll always need to take more than it seems), using supplements that will have been made by breaking down proteins anyway.
So unless you live in a laboratory and have access to endless amounts of all of the required amino acids (you can’t miss even one; you will die), and are willing to do that for the sake of proving a point, then you do really need to eat protein.
Your body cannot, for example, simply break down sugar and use it to make the protein you need.
On another technical note… Do bear in mind that many foods that we don’t necessarily think of as being sources of protein, are sources of protein.
Grains and grain products, for example, all contain protein; we just don’t think of them as that because their macronutritional profile is heavily weighted towards carbohydrates.
For that matter, even celery contains protein. How much, you may ask? Almost none! But if something has DNA, it has protein. Which means all plants and animals (at least in their unrefined forms).
So again, to even try to live without protein would very much require living in a laboratory.
We can eat too much protein: True or False?
True. First on an easy technicality; anything in excess is toxic. Even water, or oxygen. But also, in practical terms, there is such a thing as too much protein. The bar is quite high, though:
❝Based on short-term nitrogen balance studies, the Recommended Dietary Allowance of protein for a healthy adult with minimal physical activity is currently 0.8 g protein per kg bodyweight per day❞
❝To meet the functional needs such as promoting skeletal-muscle protein accretion and physical strength, dietary intake of 1.0, 1.3, and 1.6 g protein per kg bodyweight per day is recommended for individuals with minimal, moderate, and intense physical activity, respectively❞
❝Long-term consumption of protein at 2 g per kg bodyweight per day is safe for healthy adults, and the tolerable upper limit is 3.5 g per kg bodyweight per day for well-adapted subjects❞
❝Chronic high protein intake (>2 g per kg bodyweight per day for adults) may result in digestive, renal, and vascular abnormalities and should be avoided❞
Source: Dietary protein intake and human health
To put this into perspective, if you weigh about 160lbs (about 72kg), this would mean eating more than 144g protein per day, which grabbing a calculator means about 560g of lean beef, or 20oz, or 1¼lb.
If you’re eating quarter-pounder burgers though, that’s not usually so lean, so you’d need to eat more than nine quarter-pounder burgers per day to get too much protein.
High protein intake damages the kidneys: True or False?
True if you have kidney damage already; False if you are healthy. See for example:
- Effects of dietary protein restriction on the progression of advanced renal disease in the modification of diet in renal disease study
- A high protein diet has no harmful effects: a one-year crossover study in healthy male athletes
High protein intake increases cancer risk: True or False?
True or False depending on the source of the protein, so functionally false:
- Eating protein from red meat sources has been associated with higher risk for many cancers
- Eating protein from other sources has been associated with lower risk for many cancers
Source: Red Meat Consumption and Mortality Results From 2 Prospective Cohort Studies
High protein intake increase risk of heart disease: True or False?
True or False depending on the source of the protein, so, functionally false:
- Eating protein from red meat sources has been associated with higher risk of heart disease
- Eating protein from other sources has been associated with lower risk of heart disease
Source: Major Dietary Protein Sources and Risk of Coronary Heart Disease in Women
In summary…
Getting a good amount of good quality protein is important to health.
One can get too much, but one would have to go to extremes to do so.
The source of protein matters:
- Red meat is associated with many health risks, but that’s not necessarily the protein’s fault.
- Getting plenty of protein from (ideally: unprocessed) sources such as poultry, fish, and/or plants, is critical to good health.
- Consuming “whole proteins” (that contain all 9 amino acids that we can’t synthesize) are best.
Learn more: Complete proteins vs. incomplete proteins (explanation and examples)
Share This Post
-
What Harm Can One Sleepless Night Do?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ll not bury the lede: a study found that just one night of 24-hour sleep deprivation can alter immune cell profiles in young, lean, healthy people to resemble those of people with obesity and chronic inflammation.
Chronic inflammation, in turn, causes very many other chronic diseases, and worsens most of the ones it doesn’t outright cause.
The reason this happens is because in principle, inflammation is supposed to be good for us—it’s our body’s defenses coming to the rescue. However, if we imagine our immune cells as firefighters, then compare:
- A team of firefighters who are in great shape and ready to deploy at a moment’s notice, are mostly allowed to rest, sometimes get training, and get called out to a fire from time time, just enough to keep them on their toes. Today, something in your house caught fire, and they showed up in 5 minutes and put it out safely.
- A team of firefighters who have been pulling 24-hour shifts every day for the past 20 years, getting called out constantly for lost cats, burned toast, wrong numbers, the neighbor’s music, a broken fridge, and even the occasional fire. Today, your printer got jammed so they broke down your door and also your windows just for good measure, and blasted your general desk area with a fire hose, which did not resolve the problem but now your computer itself is broken.
Which team would you rather have?
The former team is a healthy immune system; the latter is the immune system of someone with chronic inflammation.
But if it’s one night, it’s not chronic, right?
Contingently true. However, the problem is that because the immune profile was made to be like the bad team we described (imagine that chaos in your house, now remember that for this metaphor, it’s your body that that’s happening to), the immediate strong negative health impact will already have knock-on effects, which in turn make it more likely that you’ll struggle to get your sleep back on track quickly.
For example, the next night you may oversleep “to compensate”, but then the following day your sleep schedule is now slid back considerably; one thing leads to another, and a month later you’re thinking “I really must sort my sleep out”.
See also: How Regularity Of Sleep Can Be Even More Important Than Duration ← A recent, large (n=72,269) 8-year prospective* observational study of adults aged 40-79 found a strong association between irregular sleep and major cardiovascular events, to such an extent that it was worse than undersleeping.
*this means they started the study at a given point, and measured what happened for the next eight years—as opposed to a retrospective study, which would look at what had happened during the previous 8 years.
What about sleep fragmentation?
In other words: getting sleep, but heavily disrupted sleep.
The answer is: basically the same deal as with missed sleep.
Specifically, elevated proinflammatory cytokines (in this context, that’s bad) and an increase in nonclassical monocytes—as are typically seen in people with obesity and chronic inflammation.
Remember: these were young, lean, healthy participants going into the study, who signed up for a controlled sleep deprivation experiment.
This is important, because the unhealthy inflammatory profile means that people with such are a lot more likely to develop diabetes, heart disease, Alzheimer’s, and many more things besides. And, famously, most people in the industrialized world are not sleeping that well.
Even amongst 10almonds readers, a health-conscious demographic by nature, 62% of 10almonds readers do not regularly get the prescribed 7–9 hours sleep (i.e. they get under 7 hours).
You can see the data on this one, here: Why You Probably Need More Sleep ← yes, including if you are in the older age range; we bust that myth in the article too!*
*Unless you have a (rare!) mutated ADRB1 gene, which reduces that. But we also cover that in the article, and how to know whether you have it.
With regard to “most people in the industrialized world are not sleeping that well”, this means that most people in the industrialized world are subject to an unseen epidemic of sleep-deprivation-induced inflammation that is creating vulnerability to many other diseases. In short, the lifestyle of the industrialized world (especially: having to work certain hours) is making most of the working population sick.
Dr. Fatema Al-Rashed, lead researcher, concluded:
❝In the long term, we aim for this research to drive policies and strategies that recognize the critical role of sleep in public health.
We envision workplace reforms and educational campaigns promoting better sleep practices, particularly for populations at risk of sleep disruption due to technological and occupational demands.
Ultimately, this could help mitigate the burden of inflammatory diseases like obesity, diabetes, and cardiovascular diseases.❞
You can read the paper in full here: Impact of sleep deprivation on monocyte subclasses and function
What can we do about it?
With regard to sleep, we’ve written so much about this, but here are three key articles that contain a lot of valuable information:
- Get Better Sleep: Beyond The Basics
- Calculate (And Enjoy) The Perfect Night’s Sleep
- Safe Effective Sleep Aids For Seniors
…and with regard to inflammation, a good concise overview of how to dial it down is:
How To Prevent Or Reduce Inflammation
Take care!
Share This Post
Related Posts
-
9 Reasons To Avoid Mobility Training
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Why might someone not want to do mobility training? Here are some important reasons:
Make an informed choice
Here’s Liv’s hit-list of reasons to skip mobility training:
- Poor Circulation: Avoid mobility training if you don’t want to improve or maintain good blood circulation, which aids muscle recovery and reduces soreness.
- Low Energy Levels: Mobility training increases oxygen flow to the brain and muscles, boosting energy. Skip it if you prefer feeling sluggish!
- Digestive Health: Stretches that rotate the torso aid digestion and relieve bloating. Definitely best to avoid it if you’re uninterested in improving digestive health.
- Joint Health: Mobility work stimulates synovial fluid production, reducing joint friction and promoting longevity. You can skip it if you don’t care about comfortable movement.
- Sleep Quality: Gentle stretching triggers relaxation, aiding restful sleep. Avoid it if you enjoy restless nights!
- Pain Tolerance: Stretching trains the nervous system to handle discomfort better. Skip it if you prefer suffering 🙂
- Headache Reduction: Mobility work relieves tension in the neck and shoulders, reducing the occurrence and severity of headaches. No need to do it if you’re fine with frequent headaches.
- Immune System Support: Mobility training boosts lymphatic circulation, aiding the immune system. Avoid it if you prefer your immune system to get exciting in a bad way.
- Stress Reduction: Mobility exercises release endorphins and lower cortisol levels, reducing stress. So, it is certainly best to skip it if you prefer feeling stressed and enjoy the many harmful symptoms of high cortisol levels!
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Mobility As Though A Sporting Pursuit: Train For The Event Of Your Life!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Alpha, beta, theta: what are brain states and brain waves? And can we control them?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s no shortage of apps and technology that claim to shift the brain into a “theta” state – said to help with relaxation, inward focus and sleep.
But what exactly does it mean to change one’s “mental state”? And is that even possible? For now, the evidence remains murky. But our understanding of the brain is growing exponentially as our methods of investigation improve.
Brain-measuring tech is evolving
Currently, no single approach to imaging or measuring brain activity gives us the whole picture. What we “see” in the brain depends on which tool we use to “look”. There are myriad ways to do this, but each one comes with trade-offs.
We learnt a lot about brain activity in the 1980s thanks to the advent of magnetic resonance imaging (MRI).
Eventually we invented “functional MRI”, which allows us to link brain activity with certain functions or behaviours in real time by measuring the brain’s use of oxygenated blood during a task.
We can also measure electrical activity using EEG (electroencephalography). This can accurately measure the timing of brain waves as they occur, but isn’t very accurate at identifying which specific areas of the brain they occur in.
Alternatively, we can measure the brain’s response to magnetic stimulation. This is very accurate in terms of area and timing, but only as long as it’s close to the surface.
What are brain states?
All of our simple and complex behaviours, as well as our cognition (thoughts) have a foundation in brain activity, or “neural activity”. Neurons – the brain’s nerve cells – communicate by a sequence of electrical impulses and chemical signals called “neurotransmitters”.
Neurons are very greedy for fuel from the blood and require a lot of support from companion cells. Hence, a lot of measurement of the site, amount and timing of brain activity is done via measuring electrical activity, neurotransmitter levels or blood flow.
We can consider this activity at three levels. The first is a single-cell level, wherein individual neurons communicate. But measurement at this level is difficult (laboratory-based) and provides a limited picture.
As such, we rely more on measurements done on a network level, where a series of neurons or networks are activated. Or, we measure whole-of-brain activity patterns which can incorporate one or more so-called “brain states”.
According to a recent definition, brain states are “recurring activity patterns distributed across the brain that emerge from physiological or cognitive processes”. These states are functionally relevant, which means they are related to behaviour.
Brain states involve the synchronisation of different brain regions, something that’s been most readily observed in animal models, usually rodents. Only now are we starting to see some evidence in human studies.
Various kinds of states
The most commonly-studied brain states in both rodents and humans are states of “arousal” and “resting”. You can picture these as various levels of alertness.
Studies show environmental factors and activity influence our brain states. Activities or environments with high cognitive demands drive “attentional” brain states (so-called task-induced brain states) with increased connectivity. Examples of task-induced brain states include complex behaviours such as reward anticipation, mood, hunger and so on.
In contrast, a brain state such as “mind-wandering” seems to be divorced from one’s environment and tasks. Dropping into daydreaming is, by definition, without connection to the real world.
We can’t currently disentangle multiple “states” that exist in the brain at any given time and place. As mentioned earlier, this is because of the trade-offs that come with recording spatial (brain region) versus temporal (timing) brain activity.
Brain states vs brain waves
Brain state work can be couched in terms such as alpha, delta and so forth. However, this is actually referring to brain waves which specifically come from measuring brain activity using EEG.
EEG picks up on changing electrical activity in the brain, which can be sorted into different frequencies (based on wavelength). Classically, these frequencies have had specific associations:
- gamma is linked with states or tasks that require more focused concentration
- beta is linked with higher anxiety and more active states, with attention often directed externally
- alpha is linked with being very relaxed, and passive attention (such as listening quietly but not engaging)
- theta is linked with deep relaxation and inward focus
- and delta is linked with deep sleep.
Brain wave patterns are used a lot to monitor sleep stages. When we fall asleep we go from drowsy, light attention that’s easily roused (alpha), to being relaxed and no longer alert (theta), to being deeply asleep (delta).
Can we control our brain states?
The question on many people’s minds is: can we judiciously and intentionally influence our brain states?
For now, it’s likely too simplistic to suggest we can do this, as the actual mechanisms that influence brain states remain hard to detangle. Nonetheless, researchers are investigating everything from the use of drugs, to environmental cues, to practising mindfulness, meditation and sensory manipulation.
Controversially, brain wave patterns are used in something called “neurofeedback” therapy. In these treatments, people are given feedback (such as visual or auditory) based on their brain wave activity and are then tasked with trying to maintain or change it. To stay in a required state they may be encouraged to control their thoughts, relax, or breathe in certain ways.
The applications of this work are predominantly around mental health, including for individuals who have experienced trauma, or who have difficulty self-regulating – which may manifest as poor attention or emotional turbulence.
However, although these techniques have intuitive appeal, they don’t account for the issue of multiple brain states being present at any given time. Overall, clinical studies have been largely inconclusive, and proponents of neurofeedback therapy remain frustrated by a lack of orthodox support.
Other forms of neurofeedback are delivered by MRI-generated data. Participants engaging in mental tasks are given signals based on their neural activity, which they use to try and “up-regulate” (activate) regions of the brain involved in positive emotions. This could, for instance, be useful for helping people with depression.
Another potential method claimed to purportedly change brain states involves different sensory inputs. Binaural beats are perhaps the most popular example, wherein two different wavelengths of sound are played in each ear. But the evidence for such techniques is similarly mixed.
Treatments such as neurofeedback therapy are often very costly, and their success likely relies as much on the therapeutic relationship than the actual therapy.
On the bright side, there’s no evidence these treatment do any harm – other than potentially delaying treatments which have been proven to be beneficial.
Susan Hillier, Professor: Neuroscience and Rehabilitation, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Myth of Normal – by Dr. Gabor Maté and Daniel Maté
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of popular beliefs (and books!) start with the assumption that everyone is, broadly speaking, “normal”. That major diversions from “normal” happen only to other people… And that minor diversions from “normal” are just something to suck up and get over—magically effecting a return to “normalcy”.
Dr. Maté, however, will have none of these unhelpful brush-offs, and observes that in fact most if not all of us have been battered by the fates one way or another. We just:
- note that we have more similarities than differences, and
- tend to hide our own differences (to be accepted) or overlook other people’s (to make them more acceptable).
How is this more helpful? Well, the above approach isn’t always, but Mate has an improvement to offer:
We must see flawed humans (including ourselves) as the product of our environments… and/but see this a reason to look at improving those environments!
Beyond that…
The final nine chapters of the books he devotes to “pathways to wholeness” and, in a nutshell, recovery. Recovery from whatever it was for you. And if you’ve had a life free from anything that needs recovering from, then congratulations! You doubtlessly have at least one loved one who wasn’t so lucky, though, so this book still makes for excellent reading.
Dr. Maté was awarded the Order of Canada for his medical work and writing. His work has mostly been about addiction, trauma, stress, and childhood development. He co-wrote this book with his son, Daniel.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: