He Thinks His Wife Died in an Understaffed Hospital. Now He’s Trying to Change the Industry.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For the past year, police Detective Tim Lillard has spent most of his waking hours unofficially investigating his wife’s death.
The question has never been exactly how Ann Picha-Lillard died on Nov. 19, 2022: She succumbed to respiratory failure after an infection put too much strain on her weakened lungs. She was 65.
For Tim Lillard, the question has been why.
Lillard had been in the hospital with his wife every day for a month. Nurses in the intensive care unit had told him they were short-staffed, and were constantly rushing from one patient to the next.
Lillard tried to pitch in where he could: brushing Ann’s shoulder-length blonde hair or flagging down help when her tracheostomy tube gurgled — a sign of possible respiratory distress.
So the day he walked into the ICU and saw staff members huddled in Ann’s room, he knew it was serious. He called the couple’s adult children: “It’s Mom,” he told them. “Come now.”
All he could do then was sit on Ann’s bed and hold her hand, watching as staff members performed chest compressions, desperately trying to save her life.
A minute ticked by. Then another. Lillard’s not sure how long the CPR continued — long enough for the couple’s son to arrive and take a seat on the other side of Ann’s bed, holding her other hand.
Finally, the intensive care doctor called it and the team stopped CPR. Time of death: 12:37 p.m.
Lillard didn’t know what to do in a world without Ann. They had been married almost 25 years. “We were best friends,” he said.
Just days before her death, nurses had told Lillard that Ann could be discharged to a rehabilitation center as soon as the end of the week. Then, suddenly, she was gone. Lillard didn’t understand what had happened.
Lillard said he now believes that overwhelmed, understaffed nurses hadn’t been able to respond in time as Ann’s condition deteriorated. And he has made it his mission to fight for change, joining some nursing unions in a push for mandatory ratios that would limit the number of patients in a nurse’s care. “I without a doubt believe 100% Ann would still be here today if they had staffing levels, mandatory staffing levels, especially in ICU,” Lillard said.
Last year, Oregon became the second state after California to pass hospital-wide nurse ratios that limit the number of patients in a nurse’s care. Michigan, Maine, and Pennsylvania are now weighing similar legislation.
But supporters of mandatory ratios are going up against a powerful hospital industry spending millions of dollars to kill those efforts. And hospitals and health systems say any staffing ratio regulations, however well-intentioned, would only put patients in greater danger.
Putting Patients at Risk
By next year, the United States could have as many as 450,000 fewer nurses than it needs, according to one estimate. The hospital industry blames covid-19 burnout, an aging workforce, a large patient population, and an insufficient pipeline of new nurses entering the field.
But nursing unions say that’s not the full story. There are now 4.7 million registered nurses in the country, more than ever before.
The problem, the unions say, is a hospital industry that’s been intentionally understaffing their units for years in order to cut costs and bolster profits. The unions say there isn’t a shortage of nurses but a shortage of nurses willing to work in those conditions.
The nurse staffing crisis is now affecting patient care. The number of Michigan nurses who say they know of a patient who has died because of understaffing has nearly doubled in recent years, according to a Michigan Nurses Association survey last year.
Just months before Ann Picha-Lillard’s death, nurses and doctors at the health system where she died had asked the Michigan attorney general to investigate staffing cuts they believed were leading to dangerous conditions, including patient deaths, according to The Detroit News.
But Lillard didn’t know any of that when he drove his wife to the hospital in October 2022. She had been feeling short of breath for a few weeks after she and Lillard had mild covid infections. They were both vaccinated, but Ann was immunocompromised. She suffered from rheumatoid arthritis, a condition that had also caused scarring in her lungs.
To be safe, doctors at DMC Huron Valley-Sinai Hospital wanted to keep Ann for observation. After a few days in the facility, she developed pneumonia. Doctors told the couple that Ann needed to be intubated. Ann was terrified but Lillard begged her to listen to the doctors. Tearfully, she agreed.
With Ann on a ventilator in the ICU, it seemed clear to Lillard that nurses were understaffed and overwhelmed. One nurse told him they had been especially short-staffed lately, Lillard said.
“The alarms would go off for the medications, they’d come into the room, shut off the alarm when they get low, run to the medication room, come back, set them down, go to the next room, shut off alarms,” Lillard recalled. “And that was going on all the time.”
Lillard felt bad for the nurses, he said. “But obviously, also for my wife. That’s why I tried doing as much as I could when I was there. I would comb her hair, clean her, just keep an eye on things. But I had no idea what was really going on.”
Finally, Ann’s health seemed to be stabilizing. A nurse told Lillard they’d be able to discharge Ann, possibly by the end of that week.
By Nov. 17, Ann was no longer sedated and she cried when she saw Lillard and her daughter. Still unable to speak, she tried to mouth words to her husband “but we couldn’t understand what she was saying,” Lillard said.
The next day, Lillard went home feeling hopeful, counting down the days until Ann could leave the hospital.
Less than 24 hours later, Ann died.
Lillard couldn’t wrap his head around how things went downhill so fast. Ann’s underlying lung condition, the infection, and her weakened state could have proved fatal in the best of circumstances. But Lillard wanted to understand how Ann had gone from nearly discharged to dying, seemingly overnight.
He turned his dining room table into a makeshift office and started with what he knew. The day Ann died, he remembered her medical team telling him that her heart rate had spiked and she had developed another infection the night before. Lillard said he interviewed two DMC Huron Valley-Sinai nurse administrators, and had his own doctor look through Ann’s charts and test results from the hospital. “Everybody kept telling me: sepsis, sepsis, sepsis,” he said.
Sepsis is when an infection triggers an extreme reaction in the body that can cause rapid organ failure. It’s one of the leading causes of death in U.S. hospitals. Some experts say up to 80% of sepsis deaths are preventable, while others say the percentage is far lower.
Lives can be saved when sepsis is caught and treated fast, which requires careful attention to small changes in vital signs. One study found that for every additional patient a nurse had to care for, the mortality rate from sepsis increased by 12%.
Lillard became convinced that had there been more nurses working in the ICU, someone could have caught what was happening to Ann.
“They just didn’t have the time,” he said.
DMC Huron Valley-Sinai’s director of communications and media relations, Brian Taylor, declined a request for comment about the 2022 staffing complaint to the Michigan attorney general.
Following the Money
When Lillard asked the hospital for copies of Ann’s medical records, DMC Huron Valley-Sinai told him he’d have to request them from its parent company in Texas.
Like so many hospitals in recent years, the Lillards’ local health system had been absorbed by a series of other corporations. In 2011, the Detroit Medical Center health system was bought for $1.5 billion by Vanguard Health Systems, which was backed by the private equity company Blackstone Group.
Two years after that, in 2013, Vanguard itself was acquired by Tenet Healthcare, a for-profit company based in Dallas that, according to its website, operates 480 ambulatory surgery centers and surgical hospitals, 52 hospitals, and approximately 160 additional outpatient centers.
As health care executives face increasing pressure from investors, nursing unions say hospitals have been intentionally understaffing nurses to reduce labor costs and increase revenue. Also, insurance reimbursements incentivize keeping nurse staffing levels low. “Hospitals are not directly reimbursed for nursing services in the same way that a physician bills for their services,” said Karen Lasater, an associate professor of nursing in the Center for Health Outcomes and Policy Research at the University of Pennsylvania. “And because hospitals don’t perceive nursing as a service line, but rather a cost center, they think about nursing as: How can we reduce this to the lowest denominator possible?” she said.
Lasater is a proponent of mandatory nurse ratios. “The nursing shortage is not a pipeline problem, but a leaky bucket problem,” she said. “And the solutions to this crisis need to address the root cause of the issue, which is why nurses are saying they’re leaving employment. And it’s rooted in unsafe staffing. It’s not safe for the patients, but it’s also not safe for nurses.”
A Battle Between Hospitals and Unions
In November, almost one year after Ann’s death, Lillard told a room of lawmakers at the Michigan State Capitol that he believes the Safe Patient Care Act could save lives. The health policy committee in the Michigan House was holding a hearing on the proposed act, which would limit the amount of mandatory overtime a nurse can be forced to work, and require hospitals to make their staffing levels available to the public.
Most significantly, the bills would require hospitals to have mandatory, minimum nurse-to-patient ratios. For example: one nurse for every patient in the ICU; one for every three patients in the emergency room; a nurse for triage; and one nurse for every four postpartum birthing patients and well-baby care.
Efforts to pass mandatory ratio laws failed in Washington and Minnesota last year after facing opposition from the hospital industry. In Minnesota, the Minnesota Nurses Association accused the Mayo Clinic of using “blackmail tactics”: Mayo had told lawmakers it would pull billions of dollars in investment from the state if mandatory ratio legislation passed. Soon afterward, lawmakers removed nurse ratios from the legislation.
While Lillard waited for his turn to speak to Michigan lawmakers about the Safe Patient Care Act in November, members of the Michigan Nurses Association, which says it represents some 13,000 nurses, told lawmakers that its units were dangerously understaffed. They said critical care nurses were sometimes caring for up to 11 patients at a time.
“Last year I coded someone in an ICU for 10 minutes, all alone, because there was no one to help me,” said the nurses association president and registered nurse Jamie Brown, reading from another nurse’s letter.
“I have been left as the only specially trained nurse to take care of eight babies on the unit: eight fragile newborns,” said Carolyn Clemens, a registered nurse from the Grand Blanc area of Michigan.
Nikia Parker said she has left full-time emergency room nursing, a job she believes is her calling. After her friend died in the hospital where she worked, she was left wondering whether understaffing may have contributed to his death.
“If the Safe Patient Care Act passed, and we have ratios, I’m one of those nurses who would return to the bedside full time,” Parker told lawmakers. “And so many of my co-workers who have left would join me.”
But not all nurses agree that mandatory ratios are a good idea.
While the American Nurses Association supports enforceable ratios as an “essential approach,” that organization’s Michigan chapter does not, saying there may not be enough nurses in the state to satisfy the requirements of the Safe Patient Care Act.
For some lawmakers, the risk of collateral damage seems too high. State Rep. Graham Filler said he worries that mandating ratios could backfire.
“We’re going to severely hamper health care in the state of Michigan. I’m talking closed wards because you can’t meet the ratio in a bill. The inability for a hospital to treat an emergent patient. So it feels kind of to me like a gamble we’re taking,” said Filler, a Republican.
Michigan hospitals are already struggling to fill some 8,400 open positions, according to the Michigan Health & Hospital Association. That association says that complying with the Safe Patient Care Act would require hiring 13,000 nurses.
Every major health system in the state signed a letter opposing mandatory ratios, saying it would force them to close as many as 5,100 beds.
Lillard watched the debate play out in the hearing. “That’s a scare tactic, in my opinion, where the hospitals say we’re going to have to start closing stuff down,” he said.
He doesn’t think legislation on mandatory ratios — which are still awaiting a vote in the Michigan House’s health policy committee — are a “magic bullet” for such a complex, national problem. But he believes they could help.
“The only way these hospitals and the administrations are gonna make any changes, and even start moving towards making it better, is if they’re forced to,” Lillard said.
Seated in the center of the hearing room in Lansing, next to a framed photo of Ann, Lillard’s hands shook as he recounted those final minutes in the ICU.
“Please take action so that no other person or other family endures this loss,” he said. “You can make a difference in saving lives.”
Grief is one thing, Lillard said, but it’s another thing to be haunted by doubts, to worry that your loved one’s care was compromised before they ever walked through the hospital doors. What he wants most, he said, is to prevent any other family from having to wonder, “What if?”
This article is from a partnership that includes Michigan Public, NPR, and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fixing Fascia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fascia: Why (And How) You Should Take Care Of Yours
Fascia is the web-like layer of connective tissue that divides your muscles and organs from each other. It simultaneously holds some stuff in place, and allows other parts to glide over each other with minimal friction.
At least, that’s what it’s supposed to do.
Like any body part, it can go wrong. More on this later. But first…
A quick note on terms
It may seem like sometimes people say “myofascial” because it sounds fancier, but it does actually have a specific meaning too:
- “Fascia” is what we just described above
- “Myofascial” means “of or relating to muscles and fascia”
For example, “myofascial release” means “stopping the fascia from sticking to the muscle where it shouldn’t” and “myofascial pain” means “pain that has to do with the muscles and fascia”. See also:
Myofascial vs Fascia: When To Use Each One? What To Consider
Why fascia is so ignored
For millennia, it was mostly disregarded as a “neither this nor that” tissue that just happens to be in the body. We didn’t pay attention to it, just like we mostly don’t pay attention to the air around us.
But, much like the air around us, we sure pay attention when something goes wrong with it!
However, even in more recent years, we’ve been held back until quite new developments like musculoskeletal ultrasound that could show us problems with the fascia.
What can go wrong
It’s supposed to be strong, thin, supple, and slippery. It holds on in the necessary places like a spiderweb, but for the most part, it is evolved for minimum friction.
Some things can cause it to thicken and become sticky in the wrong places. Things such as:
- Physical trauma, e.g. an injury or surgery—but we repeat ourselves, because a surgery is an injury! It’s a (usually) necessary injury, but an injury nonetheless.
- Compensation for pain. If a body part hurts for some reason, and your posture changes to accommodate that, doing so can mess up your fascia, and cause you different problems somewhere else entirely.
- This is not witchcraft; think of how, when using a corded vacuum cleaner, sometimes the cord can get snagged on something in the next room and we nearly break something because we expected it to just come with us and it didn’t? It’s like that.
- Repetitive movements (repetitive strain injury is partly a myofascial issue)
- Not enough movement: when it comes to range of motion, it’s “use it or lose it”.
- The human body tries its best to be as efficient as possible for us! So eventually it will go “Hey, I notice you never move more than 30º in this direction, so I’m going to stop making fascia that allows you to go past that point, and I’ll just dump the materials here instead”
“I’ll just dump the materials here instead” is also part of the problem—it creates what we colloquially call “knots”, which are not so much part of the muscle as the fascia that covers it. That’s an actual physical sticky lumpy bit.
What to do about it
Firstly, avoid the above things! But, if for whatever reason something has gone wrong and you now have sticky lumpy fascia that doesn’t let you move the way you’d like (if you have any mobility/flexibility issues that aren’t for another known reason, then this is usually it), there are things can be done:
- Heat—is definitely not a cure-all, but it’s a good first step before doing the other things. A heating pad or a warm bath are great.
- Here’s an example of a neck+back+shoulders heating pad; you can get them for different body parts, or just use an electric blanket!
- Massage—ideally, by someone else who knows what they are doing. Self-massage is possible, as is teaching oneself (there are plenty of video tutorials available), but skilled professional therapeutic myofascial release massage is the gold standard.
- Foam rollers are a great no-skill way to get going with self-massage, whether because that’s what’s available to you, or because you just want something you can do between sessions. Here’s an example of the kind we mean.
- Acupuncture—triggering localized muscular relaxation, an important part of myofascial release, is something acupuncture is good at.
- See also: Pinpointing The Usefulness Of Acupuncture ← noteworthily, the strongest criticism of acupuncture for pain relief is that it performs only slightly better than sham acupuncture, but taken in practical terms, all that really means is “sticking little needles in does work, even if not necessarily by the mechanism acupuncturists believe”
- Calisthenics—Pilates, yoga, and other forms of body movement training can help gradually get one’s fascia to where and how it’s supposed to be.
- This is that “use it or lose it” bodily efficiency we talked about!
Remember, the body is always rebuilding itself. It never stops, until you die. So on any given day, you get to choose whether it rebuilds itself a little bit worse or a little bit better.
Take care!
Share This Post
-
Can We Drink To Good Health?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Can we drink to good health?
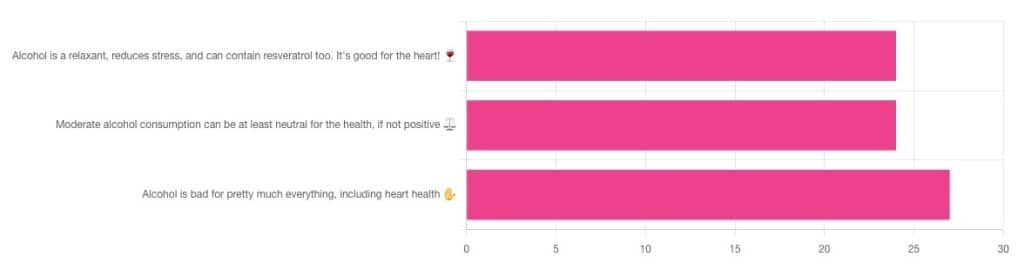
We asked you for your thoughts on alcohol and heart health, and we got quite an even spread of results!
If perchance that’s too tiny to read, the figures were:
- 32% voted for “Alcohol is a relaxant, reduces stress, and can contain resveratrol too. It’s good for the heart!”
- 32% voted for: “Moderate alcohol consumption can be at least neutral for the health, if not positive ⚖️”
- 36% voted for: “Alcohol is bad for pretty much everything, including heart health ✋”
One subscriber who voted for “Alcohol is a relaxant, reduces stress, and can contain resveratrol too. It’s good for the heart!” added the following thoughts:
❝While it isn’t necessary to consume alcohol, moderate amounts can be beneficial and contribute to well-being through social activity, celebrations, etc.❞
That’s an interesting point, and definitely many people do see alcohol that way! Of course, that does not mean that one will find no social activities, celebrations, etc, in parts of the world where alcohol consumption is uncommon. Indeed, in India, wedding parties where no alcohol is consumed can go on for days!
But, “we live in a society” and all that, and while we’re a health newsletter not a social issues newsletter, it’d be remiss of us to not acknowledge the importance of socialization for good mental health—and thus the rest of our health too.
So, if indeed all our friends and family drink alcohol, it can certainly make abstaining more of a challenge.
On that note, let’s take a moment to consider “The French Paradox” (an observation of a low prevalence of ischemic heart disease despite high intakes of saturated fat, a phenomenon accredited to the consumption of red wine).
As it happens, a comprehensive review in “Circulation”, a cardiovascular health journal, has suggested the French Paradox may not be so paradoxical after all.
Research suggests it has more to do with other lifestyle factors (and historic under-reporting of cardiovascular disease by French doctors), which would explain why Japan has lower rates of heart disease, despite drinking little wine, and more beer and spirits.
So, our subscriber’s note may not be completely without reason! It’s just about the party, not the alcohol.
One subscriber who voted for “Moderate alcohol consumption can be at least neutral for the health, if not positive ⚖️” wrote:
❝Keeping in mind, moderate means one glass of wine for women a day and two for men. Hard alcohol doesn’t have the same heart benefits as wine❞
That is indeed the guideline according to some health bodies!
In other places with different guiding advisory bodies, that’s been dropped down to one a day for everyone (the science may be universal, but how government institutions interpret that is not).
About that wine… Specifically, red wine, for its resveratrol content:
While there are polyphenols such as resveratrol in red wine that could boost heart health, there’s so little per glass that you may need 100–1000 glasses to get the dosage that provides benefits in mouse studies. If you’re not a mouse, you might even need more.
To this end, many people prefer resveratrol supplementation. ← link is to an example product, but there are plenty more so feel free to shop around
A subscriber who voted for “Alcohol is bad for pretty much everything, including heart health ✋” says:
❝New guidelines suggest 1 to 2 drinks a week are okay but the less the better.❞
If you haven’t heard these new guidelines, we’ll mention again: every government has its own official bodies and guidelines so perhaps your local guidelines differ, but for example here’s what that World Health Organization has to say (as of January this year):
WHO: No level of alcohol consumption is safe for our health
So, whom to believe? The governments who hopefully consider the welfare of their citizenry more important than the tax dollars from alcohol sales, or the World Health Organization?
It’s a tough one, but we’ll always err on the side of the science.
Share This Post
-
Ear Today, Gone Tomorrow
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Have just had microsuction to remove wax from my ears. A not unpleasant experience but would appreciate your guidance on how best to discourage the buildup of wax in the first place.❞
Well, certainly do not prod or poke it, and that includes with cotton buds (Q-Tips, for the Americans amongst us). That pushes more down than that it extracts, and creates a denser base of wax.
There is no evidence that ear candles help, and they can cause harm.
Further reading: Experts update best practices for diagnosis and treatment of earwax (cerumen impaction)
Ear drops can help, and if you want a home-remedy edition, olive oil or almond oil can be used; these oils dissolve the wax quite quickly (in fancier words: they are cerumenolytic agents); washing with water (e.g. in the shower or bath) is then all that’s needed. However, to avoid infection, ensure you are using a high-purity oil, and get one to use just for that; don’t just grab a bottle from the kitchen.
For your convenience, here is an example of medical grade almond oil (with dropper!) on Amazon
❝Every article had relevance to me. I ❤️ whole fruit, it’s my go to treat. I use ice packs to ease my arthritic knee pain, works well. I’ve read and loved Dr Gawande’s books. Great handful of almonds today❞
While this wasn’t a question, and we don’t usually publish feedback here, I (your writer here, hi) misread that as “ice picks” in the first instance, an implement we’ve probably all wanted to use to relieve pain at some point, but certainly not recommendable! Anyway, the momentary confusion made me smile, so I thought I’d share the silly thought. Smiling is infectious, and all that… And it’s certainly good for the health!
More seriously, glad you enjoyed!
Share This Post
Related Posts
-
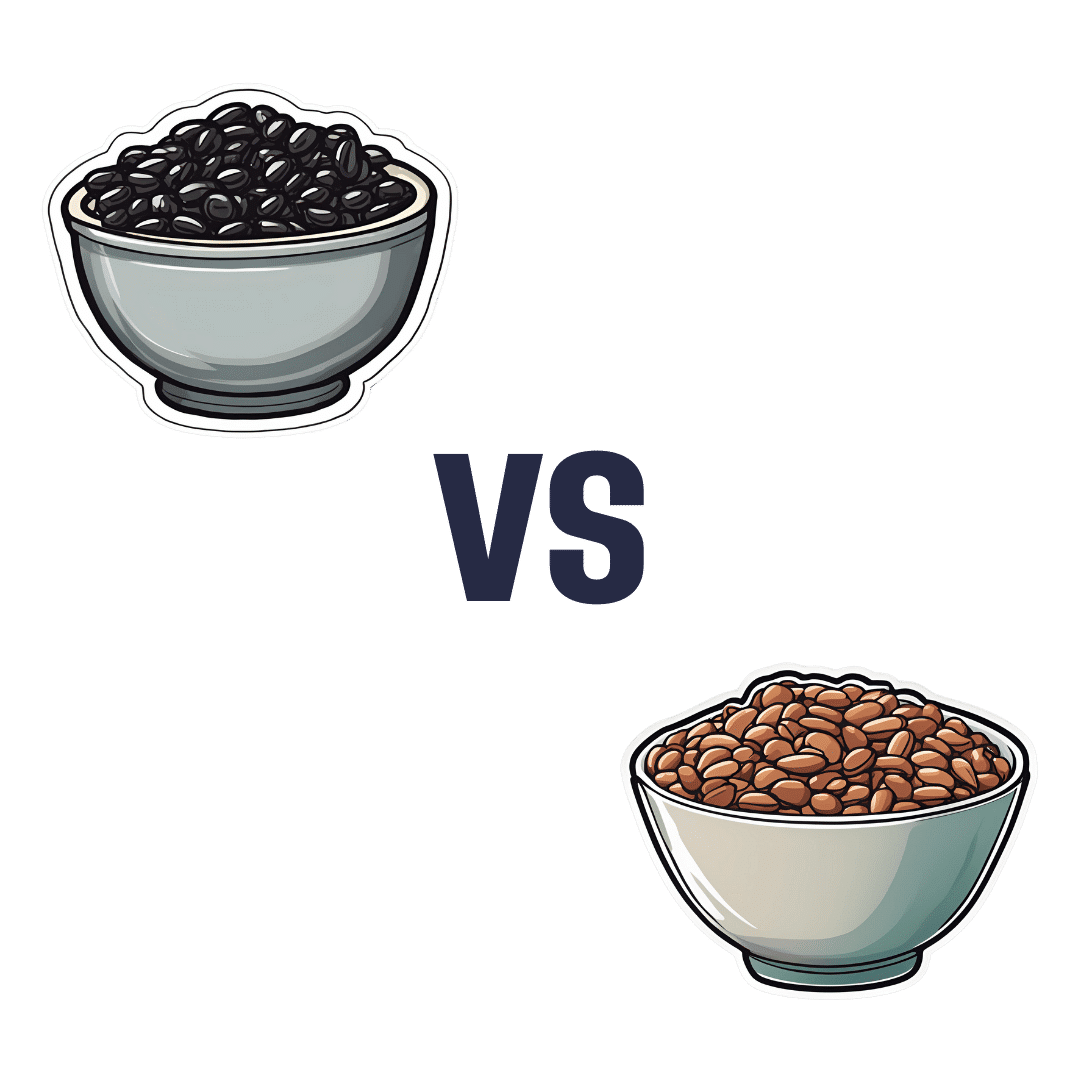
Black Beans vs Pinto Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing black beans to pinto beans, we picked the pinto beans.
Why?
Both of these beans have won all their previous comparisons, so it’s no surprise that this one was very close. Despite their different appearance, taste, and texture, their nutritional profiles are almost identical:
In terms of macros, pinto beans have a tiny bit more protein, carbs, and fiber. So, a nominal win for pinto beans, but again, the difference is very slight.
When it comes to vitamins, black beans have more of vitamins A, B1, B3, and B5, while pinto beans have more of vitamins B2, B6, B9, C, E, K and choline. Superficially, again this is nominally a win for pinto beans, but in most cases the differences are so slight as to be potentially the product of decimal place rounding.
In the category of minerals, black beans have more calcium, copper, iron, and phosphorus, while pinto beans have more magnesium, manganese, selenium, and zinc. That’s a 4:4 tie, but the only one with a meaningful margin of difference is selenium (of which pinto beans have 4x more), so we’re calling this one a very modest win for pinto beans.
All in all, adding these up makes for a “if we really are pressed to choose” win for pinto beans, but honestly, enjoy either in accordance with your preference (this writer prefers black beans!), or better yet, both.
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Not to Age – by Dr. Michael Greger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First things first: it’s a great book, and it’s this reviewer’s favorite of Dr. Greger’s so far (for posterity: it’s just been published and this reviewer has just finished reading the copy she got on pre-order)
Unlike many popular physician authors, Dr. Greger doesn’t rehash a lot of old material, and instead favours prioritizing new material in each work. Where appropriate, he’ll send the reader to other books for more specific information (e.g: you want to know how to avoid premature death? Go read How Not To Die. You want to know how to lose weight? How Not To Diet. Etc).
In the category of new information, he has a lot to offer here. And with over 8,000 references, it’s information, not conjecture. On which note, we recommend the e-book version if that’s possible for you, for three reasons:
- It’s possible to just click the references and be taken straight to the cited paper itself online
- To try to keep the book’s size down, Dr. Greger has linked to other external resources too
- The only negative reviews on Amazon, so far, are people complaining that the print copy’s text is smaller than they’d like
For all its information-density (those 8,000+ references are packed into 600ish pages), the book is very readable even to a lay reader; the author is a very skilled writer.
As for the content, we can’t fit more than a few sentences here so forgive the brevity, but we’ll mention that he covers:
- Slowing 11 pathways of aging
- The optimal anti-aging regimen according to current best science
- Preserving function (specific individual aspects of aging, e.g. hearing, sight, cognitive function, sexual function, hair, bones, etc)
- “Dr. Greger’s Anti-Aging Eight”
In terms of “flavor” of anti-aging science, his approach can be summed up as: diet and lifestyle as foundation; specific supplements and interventions as cornerstones.
Bottom line: this is now the anti-aging book.
Click here to check out How Not To Age, and look after yourself with the best modern science!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Stand Up For Your Health (Or Don’t)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may have heard the phrase “sitting is the new smoking”, and while the jury’s out on whether that’s accurate or not in terms of exactly how damaging it is, one thing that is universally agreed-upon is that sitting is indeed very bad.
It’s especially bad for your spine (because of being folded in ways it shouldn’t be), your muscles and associated nerves of the lower back and hip area, your abdominal organs (because of being compressed in ways they shouldn’t be), and your heart (because of arteries and veins being squashed up in ways they shouldn’t be), and if you remember how “what’s good for your heart is good for your brain”, the inverse is true, and what’s bad for your heart is also bad for your brain, which won’t get nourished with oxygen and nutrients and which won’t have its detritus removed as efficiently as it should; that’ll be left to build up in the brain instead.
First, elephant in the room: not everybody can stand, and of those who can, not everybody can stand for long. So obviously, work within what’s attainable for you.
Also note that while sitting is the disease-bringer/worsener, standing isn’t the only solution, for example:
- Walking is better than standing. You may be wondering: “who can’t stand but can walk?” and the answer is, a lot of people with certain kinds of chronic pain, for whom walking is less chronic-pain-exacerbating than standing, because the human body is built for movement and inactivity can worsen things even more than movement.
- See also: Managing Chronic Pain (Realistically)
- Lying down is better than sitting. One of the major problems with sitting is that your organs are all bunched up in ways they shouldn’t be. Lying down is, in this regard, closer to standing than sitting, because your body has a nice straight line to it.
- Sitting can be made less bad! For example:
- Sitting in a recliner chair in the reclined position is… Not great, if you’re then tilting your skull forwards to compensate, but if you’re just sitting back and relaxing, this is a lot better than sitting in the usual seated position, because again, it’s closer to lying down, which is closer to standing.
- Sitting in seiza (the traditional Japanese kneeling position) is, provided you do it correctly and with good posture, better than sitting in the traditional Western manner. The reason for this is simple: instead of having your torso and legs at 90°, they are at 120°ish, give or take the size of your thighs and butt (bigger being better in this regard), and even that angle can be made even better if you use a meditation bench like this one ← we’re eyeballing it and didn’t get out a protractor, but if you look at the model’s torso and thighs, that’s about 135° difference, which is huge improvement over the 90° you get while sitting Western-style.
For most of us a lot of the time though, we can stand to sit less. Think about the places you most often sit, and what can be done to reasonably minimize those, for example:
- Car: minimize driving (or being a passenger in a car); walk where reasonably possible. Public transport, if available, may have standing options.
- Office: a standing desk is, of course, the way to go. You can even use a standing desk converter, like this one. Just make sure to set it at the correct height, both in terms of where the keyboard and mouse go (the same height as your elbows are when your arms are dropped to your sides), and where the monitor goes (center of the monitor should be at eye-level).
- Note: laptops will never be right for this, unless the natural resting distance between your elbows and your eyes is about 4½ inches, which will only be the case if your total height is approximately 1 foot and 2 inches. For anyone taller than that, laptops are still great to have when on the move and as a backup, but not great for ergonomics.
- Workaround: if for some reason you must use a laptop for your day-to-day work, consider using a bluetooth keyboard so that you can still set them the appropriate height-distance apart and thus not have to hunch over them.
- Dining room: sitting to eat a main meal is reasonable, but consider standing options for lighter bites; a standing-height “brunch bar” is great if you can arrange one.
- Lounge: let it live up to its name, and actually lounge: if you’re not going to stand, then horizontal lounging is an improvement over sitting—as is sitting on the floor, and changing your position frequently. Who knew, kids had it right in that regard!
- Note: if, like this writer, you do a lot of reading, the same applies regardless of which room you’re doing it in.
- Bedroom: a culprit for many will be sitting while doing a beauty routine and/or possibly make-up. Easily avoided if you set a well-lit mirror at the correct height to use while standing.
- Note: at the correct height though! While hunching up over a wall-mounted mirror is an improvement over hunching up at a seated vanity, it’s not a great improvement. You want to be able to stand with good posture and do it comfortably.
- Bathroom: leave your phone outside—which is also a good approach for avoiding hemorrhoids! See also: Half Of Americans Over 50 Have Hemorrhoids, But They Can Be Prevented!
Want to know more?
We reviewed this book recently, which goes into all of the above in much more detail than we have room for here, plus also discusses a lot of social reframes that can be used (since a lot of sitting is a matter of social expectations, not actual need). It’s a very useful read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Walking is better than standing. You may be wondering: “who can’t stand but can walk?” and the answer is, a lot of people with certain kinds of chronic pain, for whom walking is less chronic-pain-exacerbating than standing, because the human body is built for movement and inactivity can worsen things even more than movement.