The Science Of New Year’s Pre-Resolutions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Science Of New Year’s Pre-Resolutions
There’s a military dictum that “prior preparation and planning prevents piss-poor performance”.
Would it surprise you to know that soldiers going on the attack are not focused on the goal? Rather, they are focused on the process.
With drills and mnemonics, everything that can be controlled for in advance is; every action, every reaction, everything that can go wrong, and all the “if x then y” decisions in between pre-battle PREWAR and PAWPERSO and post-battle PACESDO (all mnemonic acronyms; the content is not important here but the principle is).
In short: take Murphy’s Law into account now, and plan accordingly!
The same goes for making your plans the winning kind
If you want your resolutions to work, you may need to make pre-resolutions now, so that you’re properly prepared:
- Do you want to make an exercise habit? Make sure now that you have the right clothes/shoes/etc, make sure that they fit you correctly, make sure you have enough of them that you can exercise when one set’s in the wash, etc.
- What grace will you allow yourself if tired, unwell, busy? What’s your back-up plan so that you still do what you can at those times when “what you can” is legitimately a bit less?
- If it’s an outdoors plan, what’s your plan for when it’s rainy? Snowy? Dangerously hot?
- What are the parameters for what counts? Make it measurable. How many exercise sessions per week, what duration?
- Do you want to make a diet habit? Make sure that you have in the healthy foods that you want to eat; know where you can and will get things. We’re often creatures of habit when it comes to shopping, so planning will be critical here!
- Do you want to cut some food/drink/substance out? Make sure you have a plan to run down or otherwise dispose of your current stock first. And make sure you have alternatives set up, and if it was something you were leaning on as a coping strategy of some kind (e.g. alcohol, cannabis, comfort-eating, etc), make sure you have an alternative coping strategy, too!
See also: How To Reduce Or Quit Alcohol
We promised science, so here it comes
Approach-oriented resolutions work better than avoidance-oriented ones.
This means: positively-framed resolutions work better than negatively-framed ones.
On a simple level, this means that, for example, resolving to exercise three times per week is going to work better than resolving to not consume alcohol.
But what if you really want to quit something? Just frame it positively. There’s a reason that Alcoholics Anonymous (and similar Thing Anonymous groups) measure days sober, not relapses.
So it’s not “I will not consume alcohol” but “I will get through each day alcohol-free”.
Semantics? Maybe, but it’s also science:
Why January the 1st? It’s a fresh start
Resolutions started on the 1st of January enjoy a psychological boost of a feeling of a fresh start, a new page, a new chapter.
Similar benefits can be found from starting on the 1st of a month in general, or on a Monday, or on some date that is auspicious to the person in question (religious fasts tied to calendar dates are a fine example of this).
Again, this is borne-out by science:
The Fresh Start Effect: Temporal Landmarks Motivate Aspirational Behavior
Make it a habit
Here be science:
How do people adhere to goals when willpower is low? The profits (and pitfalls) of strong habits
As for how to do that?
How To Really Pick Up (And Keep!) Those Habits
Trim the middle
No, we’re not talking about your waistline. Rather, what Dr. Ayelet Fischbach refers to as “the middle problem”:
❝We’re highly motivated at the beginning. Over time, our motivation declines as we lose steam. To the extent that our goal has a clear end point, our motivation picks up again toward the end.
Therefore, people are more likely to adhere to their standards at the beginning and end of goal pursuit—and slack in the middle. We demonstrate this pattern of judgment and behavior in adherence to ethical standards (e.g., cheating), religious traditions (e.g., skipping religious rituals), and performance standards (e.g., “cutting corners” on a task).
We also show that the motivation to adhere to standards by using proper means is independent and follows a different pattern from the motivation to reach the end state of goal pursuit❞
Read: The end justifies the means, but only in the middle
How to fix this, then?
Give yourself consistent, recurring, short-term goals, with frequent review points. That way, it’s never “the middle” for long:
The fresh start effect: temporal landmarks motivate aspirational behavior
See also:
How do people protect their long-term goals from the influence of short-term motives or temptations?
Finally…
You might like this previous main feature of ours that was specifically about getting oneself through those “middle” parts:
How To Keep On Keeping On… Long Term!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Beetroot vs Pumpkin – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing beetroot to pumpkin, we picked the beetroot.
Why?
It was close! And an argument could be made for either.
In terms of macros, beetroot has about 3x more protein and about 3x more fiber, as well as about 2x more carbs, making it the “more food per food” option. While both have a low glycemic index, we picked the beetroot here for its better numbers overall.
In the category of vitamins, beetroot has more of vitamins B6 and B9, while pumpkin has more of vitamins A, B2, B3, B5, E, and K. So, a fair win for pumpkin this time.
When it comes to minerals, though, beetroot has more calcium, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while pumpkin has a tiny bit more copper. An easy win for beetroot here.
In short, both are great, and although pumpkin shines in the vitamin category, beetroot wins on overall nutritional density.
Want to learn more?
You might like to read:
No, beetroot isn’t vegetable Viagra. But here’s what it can do
Take care!
Share This Post
-
Goji Berries: Which Benefits Do They Really Have?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Are Goji Berries Really A Superfood?
Goji berries are popularly considered a superfood, and sold for everything from anti-aging effects, to exciting benefits* that would get this email directed to your spam folder if we described them.
*We searched so you don’t have to: there doesn’t seem to be much research to back [that claim that we can’t mention], but we did find one paper on its “invigorating” benefits for elderly male rats. We prefer to stick to human studies where we can!
So how does the science stack up for the more mainstream claims?
Antioxidant effects
First and most obvious for this fruit that’s full of helpful polysaccharides, carotenoids, phenolic acids, and flavonoids, yes, they really do have strong antioxidant properties:
Immune benefits
Things that are antioxidant are generally also anti-inflammatory, and often have knock-on benefits for the immune system. That appears to be the case here.
For example, in this small-but-statistically-significant study (n=60) in healthy adults (aged 55–72 years)
❝The GoChi group showed a statistically significant increase in the number of lymphocytes and levels of interleukin-2 and immunoglobulin G compared to pre-intervention and the placebo group, whereas the number of CD4, CD8, and natural killer cells or levels of interleukin-4 and immunoglobulin A were not significantly altered. The placebo group showed no significant changes in any immune measures.
Whereas the GoChi group showed a significant increase in general feelings of well-being, such as fatigue and sleep, and showed a tendency for increased short-term memory and focus between pre- and post-intervention, the placebo group showed no significant positive changes in these measures.❞
“GoChi” here is a brand name for goji berries, and it’s not clear from the abstract whether the company funded the study:
Here’s another study, this time n=150, and ages 65–70 years old. This time it’s with a different brand (“Lacto-Wolfberry”, a milk-with-goji supplement drink) and it’s also unclear whether the company funded the study. However, taking the data at face value:
❝In conclusion, long-term dietary supplementation with Lacto-Wolfberry in elderly subjects enhances their capacity to respond to antigenic challenge without overaffecting their immune system, supporting a contribution to reinforcing immune defense in this population. ❞
In other words: it allowed those who took it to get measurably more benefit from the flu vaccinations that they received, without any ill effects.
Anticancer potential
This one’s less contentious (the immune benefits seemed very credible; we’d just like to see more transparent research to say for sure), so in the more clearly-evidenced case against cancer we’ll just drop a few quick studies, clipped for brevity:
- Goji berry (Lycium barbarum) inhibits the proliferation, adhesion, and migration of oral cancer cells
- A closer look at immunomodulatory properties of goji berries extract in human colon cancer cells
- Lycium barbarum polysaccharides induce apoptosis in human prostate cancer cells and inhibits prostate cancer growth
- Identification of goji berry cyclic peptides and anticervical carcinoma activity
- Antiproliferative effects of Lycium barbarum’s (goji berry) fractions on breast cancer Cell Lines
You get the idea: it helps!
Bonus benefit for the eyes
Goji berries also help against age-related macular degeneration. The research for this is in large part secondary, i.e. goji berries contain things x, y, and z, and then separate studies say that those things help against age-related macular degeneration.
We did find some goji-specific studies though! One of them was for our old friends the “Lacto-Wolfberry” people and again, wasn’t very transparent, so we’ll not take up extra time/space with that one here.
Instead, here’s a much clearer, transparent, and well-referenced study with no conflicts of interest, that found:
❝Overall, daily supplementation with Goji berry for 90d improves MPOD by increasing serum Z levels rather than serum L levels in early AMD patients. Goji berry may be an effective therapeutic intervention for preventing the progression of early AMD.❞
- MPOD = Macular Pigment Optical Density, a standard diagnostic tool for age-related macular degeneration
- AMD = Age-related Macular Degeneration
(that whole paper is very compelling reading, if you have time)
If you want a quicker read, we offer:
How To Avoid Age-Related Macular Degeneration
and also…
Where to get goji berries?
You can probably find them at your local health food store, if not the supermarket. However, if you’d like to buy them online, here’s an example product on Amazon for your convenience
Enjoy!
Share This Post
-
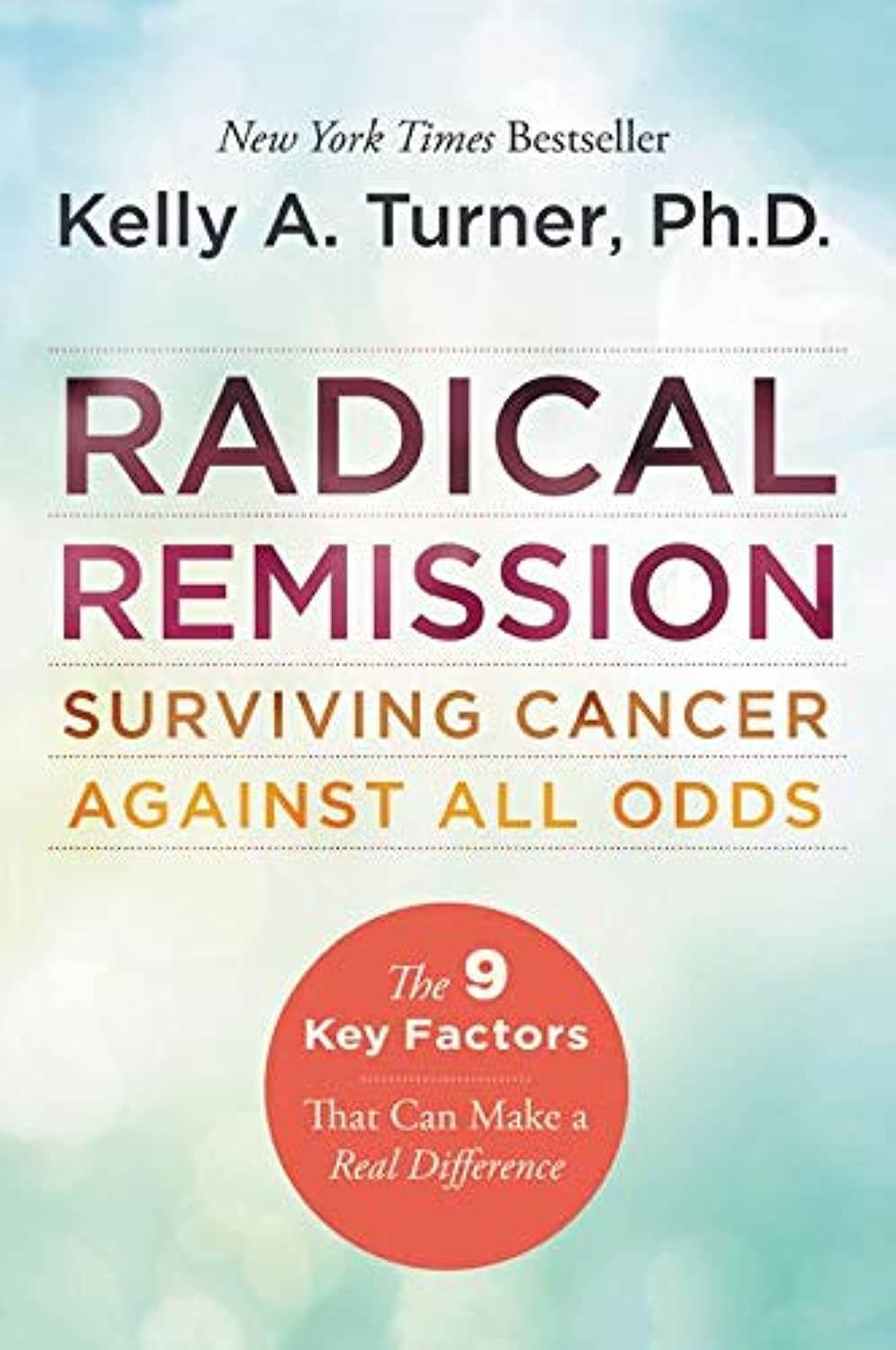
Radical Remission – by Dr. Kelly Turner
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this is not:an autobiographical account of the “I beat cancer and you can too” pep-talk style.
What it is: a very readable pop-science book based on the author’s own PhD research into radical remission.
She knew that a very small percentage of people experience spontaneous radical remission (or quasi-spontaneous, if the remission is attributed to lifestyle changes, and/or some alternative therapy), but a small percentage of people means a large number worldwide, so she travelled the world studying over 1,000 cases of people with late-stage cancer who had either not gone for conventional anticancer drugs, or had and then stopped, and lived to tell the tale.
While she doesn’t advocate for any particular alternative therapy, she does report on what things came to her attention. She does advocate for some lifestyle changes.
Perhaps the biggest value this book offers is in its promised “9 key factors that can make a real difference”, which are essentially her conclusions from her PhD dissertation.
There isn’t room to talk about them here in a way that wouldn’t be misleading/unhelpful for a paucity of space, so perhaps we’ll do a main feature one of these days.
Bottom line: if you have (or a loved one has) cancer, this is an incredibly sensible book to read. If you don’t, then it’s an interesting and thought-provoking book to read.
Click here to check out Radical Remission, and learn about the factors at hand!
Share This Post
Related Posts
-
What’s the difference between a food allergy and an intolerance?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At one time or another, you’ve probably come across someone who is lactose intolerant and might experience some unpleasant gut symptoms if they have dairy. Maybe it’s you – food intolerances are estimated to affect up to 25% of Australians.
Meanwhile, cow’s milk allergy is one of the most common food allergies in infants and young children, affecting around one in 100 infants.
But what’s the difference between food allergies and food intolerances? While they might seem alike, there are some fundamental differences between the two.
Feel good studio/Shutterstock What is an allergy?
Australia has one of the highest rates of food allergies in the world. Food allergies can develop at any age but are more common in children, affecting more than 10% of one-year-olds and 6% of children at age ten.
A food allergy happens when the body’s immune system mistakenly reacts to certain foods as if they were dangerous. The most common foods that trigger allergies include eggs, peanuts and other nuts, milk, shellfish, fish, soy and wheat.
Mild to moderate signs of food allergy include a swollen face, lips or eyes; hives or welts on your skin; or vomiting. A severe allergic reaction (called anaphylaxis) can cause trouble breathing, persistent dizziness or collapse.
What is an intolerance?
Food intolerances (sometimes called non-allergic reactions) are also reactions to food, but they don’t involve your immune system.
For example, lactose intolerance is a metabolic condition that happens when the body doesn’t produce enough lactase. This enzyme is needed to break down the lactose (a type of sugar) in dairy products.
Food intolerances can also include reactions to natural chemicals in foods (such as salicylates, found in some fruits, vegetables, herbs and spices) and problems with artificial preservatives or flavour enhancers.
Lactose intolerance is caused by a problem with breaking down lactose in milk. Pormezz/Shutterstock Symptoms of food intolerances can include an upset stomach, headaches and fatigue, among others.
Food intolerances don’t cause life-threatening reactions (anaphylaxis) so are less dangerous than allergies in the short term, although they can cause problems in the longer term such as malnutrition.
We don’t know a lot about how common food intolerances are, but they appear to be more commonly reported than allergies. They can develop at any age.
It can be confusing
Some foods, such as peanuts and tree nuts, are more often associated with allergy. Other foods or ingredients, such as caffeine, are more often associated with intolerance.
Meanwhile, certain foods, such as cow’s milk and wheat or gluten (a protein found in wheat, rye and barley), can cause both allergic and non-allergic reactions in different people. But these reactions, even when they’re caused by the same foods, are quite different.
For example, children with a cow’s milk allergy can react to very small amounts of milk, and serious reactions (such as throat swelling or difficulty breathing) can happen within minutes. Conversely, many people with lactose intolerance can tolerate small amounts of lactose without symptoms.
There are other differences too. Cow’s milk allergy is more common in children, though many infants will grow out of this allergy during childhood.
Lactose intolerance is more common in adults, but can also sometimes be temporary. One type of lactose intolerance, secondary lactase deficiency, can be caused by damage to the gut after infection or with medication use (such as antibiotics or cancer treatment). This can go away by itself when the underlying condition resolves or the person stops using the relevant medication.
Whether an allergy or intolerance is likely to be lifelong depends on the food and the reason that the child or adult is reacting to it.
Allergies to some foods, such as milk, egg, wheat and soy, often resolve during childhood, whereas allergies to nuts, fish or shellfish, often (but not always) persist into adulthood. We don’t know much about how likely children are to grow out of different types of food intolerances.
How do you find out what’s wrong?
If you think you may have a food allergy or intolerance, see a doctor.
Allergy tests help doctors find out which foods might be causing your allergic reactions (but can’t diagnose food intolerances). There are two common types: skin prick tests and blood tests.
In a skin prick test, doctors put tiny amounts of allergens (the things that can cause allergies) on your skin and make small pricks to see if your body reacts.
A blood test checks for allergen-specific immunoglobulin E (IgE) antibodies in your blood that show if you might be allergic to a particular food.
Blood tests can help diagnose allergies. RossHelen/Shutterstock Food intolerances can be tricky to figure out because the symptoms depend on what foods you eat and how much. To diagnose them, doctors look at your health history, and may do some tests (such as a breath test). They may ask you to keep a record of foods you eat and timing of symptoms.
A temporary elimination diet, where you stop eating certain foods, can also help to work out which foods you might be intolerant to. But this should only be done with the help of a doctor or dietitian, because eliminating particular foods can lead to nutritional deficiencies, especially in children.
Is there a cure?
There’s currently no cure for food allergies or intolerances. For allergies in particular, it’s important to strictly avoid allergens. This means reading food labels carefully and being vigilant when eating out.
However, researchers are studying a treatment called oral immunotherapy, which may help some people with food allergies become less sensitive to certain foods.
Whether you have a food allergy or intolerance, your doctor or dietitian can help you to make sure you’re eating the right foods.
Victoria Gibson, a Higher Degree by Research student and Research Officer at the School of Nursing, Midwifery and Social Work at the University of Queensland, and Rani Scott-Farmer, a Senior Research Assistant at the University of Queensland, contributed to this article.
Jennifer Koplin, Group Leader, Childhood Allergy & Epidemiology, The University of Queensland and Desalegn Markos Shifti, Postdoctoral Research Fellow, Child Health Research Centre, Faculty of Medicine, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Redcurrants vs Cranberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing redcurrants to cranberries, we picked the redcurrants.
Why?
First know: here we’re comparing raw redcurrants to raw cranberries, with no additives in either case. If you buy jelly made from either, or if you buy dried fruits but the ingredients list has a lot of added sugar and often some vegetable oil, then that’s going to be very different. But for now… Let’s look at just the fruits:
In terms of macros, redcurrants are higher in carbs, but also higher in fiber, and have the lower glycemic index as cranberries have nearly 2x the GI.
When it comes to vitamins, redcurrants have more of vitamins B1, B2, B6, B9, C, K, and choline, while cranberries have more of vitamins A, B5, and E. In other words, a clear win for redcurrants.
In the category of minerals, redcurrants sweep even more convincingly with a lot more calcium, copper, iron, magnesium, phosphorus, potassium, selenium, and zinc. On the other hand, cranberries boast a little more manganese; they also have about 2x the sodium.
Both berries have generous amounts of assorted phytochemicals (flavonoids and others), and/but nothing to set one ahead of the other.
As per any berries that aren’t poisonous, both of these are fine choices for most people most of the time, but redcurrants win with room to spare in most categories.
Want to learn more?
You might like to read:
Health Benefits Of Cranberries (But: You’d Better Watch Out)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Understanding Cellulitis: Skin And Soft Tissue Infections
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference between a minor passing skin complaint, and a skin condition that’s indicative of something more serious? Dr. Thomas Watchman explains:
More than skin-deep
Cellulitis sounds benign enough, like having a little cellulite perhaps, but in fact it means an infection of the skin and—critically—the underlying soft tissues.
Normally, the skin acts as a barrier against infections, but this barrier can be breached by physical trauma (i.e. an injury that broke the skin), eczema, fungal nail infections, skin ulcers, and other similar things that disrupt the skin’s ability to protect us.
Things to watch out for: Dr. Watchman advises we keep an eye out for warm, reddened skin, swelling, and blisters. Specifically, a golden-yellow crust to these likely indicates a Staphylococcus aureus infection (hence the name).
There’s a scale of degrees of severity:
- Class 1: No systemic toxicity or comorbidities
- Class 2: Systemic toxicity or comorbidities present
- Class 3: Significant systemic toxicity or comorbidities with risk of significant deterioration
- Class 4: Sepsis or life-threatening infection
…with antibiotics being recommended in the latter two cases there, or in other cases for frail, young, old, or immunocompromised patients. Given the rather “scorched earth” results of antibiotics (they cause a lot of collateral iatrogenic damage), this can be taken as a sign of how seriously such infections should be taken.
For more about all this, including visual guides, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Of Brains & Breakouts: The Brain-Skin Doctor
- Beyond Supplements: The Real Immune-Boosters!
- Antibiotics? You Might Want To Think Thrice
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: