America’s Health System Isn’t Ready for the Surge of Seniors With Disabilities
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The number of older adults with disabilities — difficulty with walking, seeing, hearing, memory, cognition, or performing daily tasks such as bathing or using the bathroom — will soar in the decades ahead, as baby boomers enter their 70s, 80s, and 90s.
But the health care system isn’t ready to address their needs.
That became painfully obvious during the covid-19 pandemic, when older adults with disabilities had trouble getting treatments and hundreds of thousands died. Now, the Department of Health and Human Services and the National Institutes of Health are targeting some failures that led to those problems.
One initiative strengthens access to medical treatments, equipment, and web-based programs for people with disabilities. The other recognizes that people with disabilities, including older adults, are a separate population with special health concerns that need more research and attention.
Lisa Iezzoni, 69, a professor at Harvard Medical School who has lived with multiple sclerosis since her early 20s and is widely considered the godmother of research on disability, called the developments “an important attempt to make health care more equitable for people with disabilities.”
“For too long, medical providers have failed to address change in society, changes in technology, and changes in the kind of assistance that people need,” she said.
Among Iezzoni’s notable findings published in recent years:
Most doctors are biased. In survey results published in 2021, 82% of physicians admitted they believed people with significant disabilities have a worse quality of life than those without impairments. Only 57% said they welcomed disabled patients.
“It’s shocking that so many physicians say they don’t want to care for these patients,” said Eric Campbell, a co-author of the study and professor of medicine at the University of Colorado.
While the findings apply to disabled people of all ages, a larger proportion of older adults live with disabilities than younger age groups. About one-third of people 65 and older — nearly 19 million seniors — have a disability, according to the Institute on Disability at the University of New Hampshire.
Doctors don’t understand their responsibilities. In 2022, Iezzoni, Campbell, and colleagues reported that 36% of physicians had little to no knowledge of their responsibilities under the 1990 Americans With Disabilities Act, indicating a concerning lack of training. The ADA requires medical practices to provide equal access to people with disabilities and accommodate disability-related needs.
Among the practical consequences: Few clinics have height-adjustable tables or mechanical lifts that enable people who are frail or use wheelchairs to receive thorough medical examinations. Only a small number have scales to weigh patients in wheelchairs. And most diagnostic imaging equipment can’t be used by people with serious mobility limitations.
Iezzoni has experienced these issues directly. She relies on a wheelchair and can’t transfer to a fixed-height exam table. She told me she hasn’t been weighed in years.
Among the medical consequences: People with disabilities receive less preventive care and suffer from poorer health than other people, as well as more coexisting medical conditions. Physicians too often rely on incomplete information in making recommendations. There are more barriers to treatment and patients are less satisfied with the care they do get.
Egregiously, during the pandemic, when crisis standards of care were developed, people with disabilities and older adults were deemed low priorities. These standards were meant to ration care, when necessary, given shortages of respirators and other potentially lifesaving interventions.
There’s no starker example of the deleterious confluence of bias against seniors and people with disabilities. Unfortunately, older adults with disabilities routinely encounter these twinned types of discrimination when seeking medical care.
Such discrimination would be explicitly banned under a rule proposed by HHS in September. For the first time in 50 years, it would update Section 504 of the Rehabilitation Act of 1973, a landmark statute that helped establish civil rights for people with disabilities.
The new rule sets specific, enforceable standards for accessible equipment, including exam tables, scales, and diagnostic equipment. And it requires that electronic medical records, medical apps, and websites be made usable for people with various impairments and prohibits treatment policies based on stereotypes about people with disabilities, such as covid-era crisis standards of care.
“This will make a really big difference to disabled people of all ages, especially older adults,” said Alison Barkoff, who heads the HHS Administration for Community Living. She expects the rule to be finalized this year, with provisions related to medical equipment going into effect in 2026. Medical providers will bear extra costs associated with compliance.
Also in September, NIH designated people with disabilities as a population with health disparities that deserves further attention. This makes a new funding stream available and “should spur data collection that allows us to look with greater precision at the barriers and structural issues that have held people with disabilities back,” said Bonnielin Swenor, director of the Johns Hopkins University Disability Health Research Center.
One important barrier for older adults: Unlike younger adults with disabilities, many seniors with impairments don’t identify themselves as disabled.
“Before my mom died in October 2019, she became blind from macular degeneration and deaf from hereditary hearing loss. But she would never say she was disabled,” Iezzoni said.
Similarly, older adults who can’t walk after a stroke or because of severe osteoarthritis generally think of themselves as having a medical condition, not a disability.
Meanwhile, seniors haven’t been well integrated into the disability rights movement, which has been led by young and middle-aged adults. They typically don’t join disability-oriented communities that offer support from people with similar experiences. And they don’t ask for accommodations they might be entitled to under the ADA or the 1973 Rehabilitation Act.
Many seniors don’t even realize they have rights under these laws, Swenor said. “We need to think more inclusively about people with disabilities and ensure that older adults are fully included at this really important moment of change.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Healthiest Bread Recipe You’ll Probably Find
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝[About accidental scalding with water] Is cold water actually the best immediate treatment for a burn? Maybe there is something better, or something I should apply after the cold water.❞
If this is a case of spilled tea or similar—as in your story, which (apologies) we clipped for brevity—indeed, cold running water is best, and nothing else should be needed. It’s up to you whether you want to invest the time based on the extent of the scalding, but 10 minutes is recommended to minimize tissue damage.
If it’s a more severe scalding or burning, seek medical attention immediately. If it’s a burn to anywhere other than the airway, cold running water is still best for 10 minutes, but if you have to choose between that and professional medical attention, don’t delay the help.
If it’s a burn you’ve given 10 minutes of cold running water and it still hurts and/or has blistered, cover it in a sterile, non-adhesive dressing that extends well beyond the visible burn (because the actual damage probably extends further, and you don’t want to find this out the hard way later). If the burn is to the face, do still irrigate but not cover it; wait for help.
Do not apply any kind of cream, lotion, oil, etc. No matter how tempting, no matter where the burn is.
All of the above also goes for splashed oil, chemical burns, and electrical burns too (but obviously, make sure to get away from the electricity first).
Source: this ex-military writer was trained for this sort of thing and, suffice it to say, has dealt with more serious things than spilled tea before now.
Legal note: notwithstanding the above, we are a health science newsletter, not paramedics. Also, circumstances may differ, and best practices may change. In the case of serious injury, call emergency services first, and follow their instructions over ours.
Take care!
Share This Post
-
Which Sugars Are Healthier, And Which Are Just The Same?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From Apples to Bees, and High-Fructose Cs
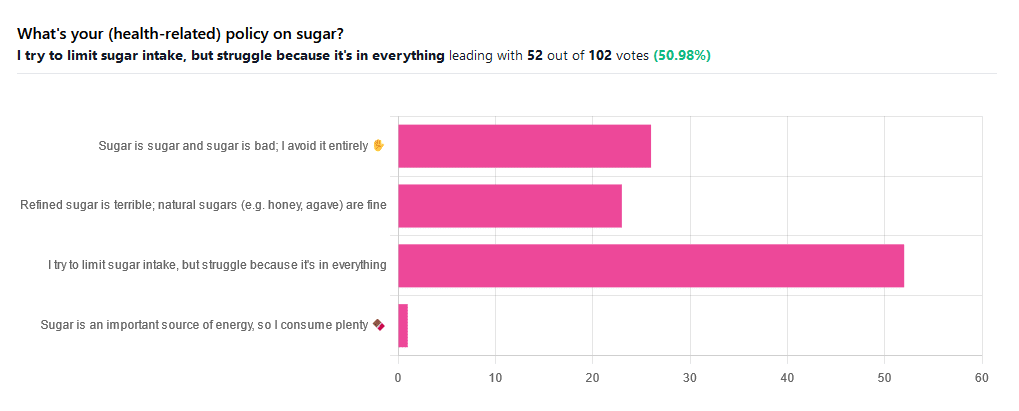
We asked you for your (health-related) policy on sugar. The trends were as follows:
- About half of all respondents voted for “I try to limit sugar intake, but struggle because it’s in everything”
- About a quarter of all respondents voted for “Refined sugar is terrible; natural sugars (e.g. honey, agave) are fine”
- About a quarter of all respondents voted for “Sugar is sugar and sugar is bad; I avoid it entirely”
- One (1) respondent voted for “Sugar is an important source of energy, so I consume plenty”
Writer’s note: I always forget to vote in these, but I’d have voted for “I try to limit sugar intake, but struggle because it’s in everything”.
Sometimes I would like to make my own [whatever] to not have the sugar, but it takes so much more time, and often money too.
So while I make most things from scratch (and typically spend about an hour cooking each day), sometimes store-bought is the regretfully practical timesaver/moneysaver (especially when it comes to condiments).
So, where does the science stand?
There has, of course, been a lot of research into the health impact of sugar.
Unfortunately, a lot of it has been funded by sugar companies, which has not helped. Conversely, there are also studies funded by other institutions with other agendas to push, and some of them will seek to make sugar out to be worse than it is.
So for today’s mythbusting overview, we’ve done our best to quality-control studies for not having financial conflicts of interest. And of course, the usual considerations of favoring high quality studies where possible Large sample sizes, good method, human subjects, that sort of thing.
Sugar is sugar and sugar is bad: True or False?
False and True, respectively.
- Sucrose is sucrose, and is generally bad.
- Fructose is fructose, and is worse.
Both ultimately get converted into glycogen (if not used immediately for energy), but for fructose, this happens mostly* in the liver, which a) taxes it b) goes very unregulated by the pancreas, causing potentially dangerous blood sugar spikes.
This has several interesting effects:
- Because fructose doesn’t directly affect insulin levels, it doesn’t cause insulin insensitivity (yay)
- Because fructose doesn’t directly affect insulin levels, this leaves hyperglycemia untreated (oh dear)
- Because fructose is metabolized by the liver and converted to glycogen which is stored there, it’s one of the main contributors to non-alcoholic fatty liver disease (at this point, we’re retracting our “yay”)
Read more: Fructose and sugar: a major mediator of non-alcoholic fatty liver disease
*”Mostly” in the liver being about 80% in the liver. The remaining 20%ish is processed by the kidneys, where it contributes to kidney stones instead. So, still not fabulous.
Fructose is very bad, so we shouldn’t eat too much fruit: True or False?
False! Fruit is really not the bad guy here. Fruit is good for you!
Fruit does contain fructose yes, but not actually that much in the grand scheme of things, and moreover, fruit contains (unless you have done something unnatural to it) plenty of fiber, which mitigates the impact of the fructose.
- A medium-sized apple (one of the most sugary fruits there is) might contain around 11g of fructose
- A tablespoon of high-fructose corn syrup can have about 27g of fructose (plus about 3g glucose)
Read more about it: Effects of high-fructose (90%) corn syrup on plasma glucose, insulin, and C-peptide in non-insulin-dependent diabetes mellitus and normal subjects
However! The fiber content (in fruit) mitigates the impact of the fructose almost entirely anyway.
And if you take fruits that are high in sugar and/but high in polyphenols, like berries, they now have a considerable net positive impact on glycemic health:
- Polyphenols and Glycemic Control
- Polyphenols and their effects on diabetes management: A review
- Dietary polyphenols as antidiabetic agents: Advances and opportunities
You may be wondering: what was that about “unless you have done something unnatural to it”?
That’s mostly about juicing. Juicing removes much (or all) of the fiber, and if you do that, you’re basically back to shooting fructose into your veins:
- Effect of Fruit Juice on Glucose Control and Insulin Sensitivity in Adults: A Meta-Analysis of 12 Randomized Controlled Trials
- Intake of Fruit, Vegetables, and Fruit Juices and Risk of Diabetes in Women
Natural sugars like honey, agave, and maple syrup, are healthier than refined sugars: True or False?
True… Sometimes, and sometimes marginally.
This is partly because of the glycemic index and glycemic load. The glycemic index scores tail off thus:
- table sugar = 65
- maple syrup = 54
- honey = 46
- agave syrup = 15
So, that’s a big difference there between agave syrup and maple syrup, for example… But it might not matter if you’re using a very small amount, which means it may have a high glycemic index but a low glycemic load.
Note, incidentally, that table sugar, sucrose, is a disaccharide, and is 50% glucose and 50% fructose.
The other more marginal health benefits come from that fact that natural sugars are usually found in foods high in other nutrients. Maple syrup is very high in manganese, for example, and also a fair source of other minerals.
But… Because of its GI, you really don’t want to be relying on it for your nutrients.
Wait, why is sugar bad again?
We’ve been covering mostly the more “mythbusting” aspects of different forms of sugar, rather than the less controversial harms it does, but let’s give at least a cursory nod to the health risks of sugar overall:
- Obesity and associated metabolic risk
- Main contributor to non-alcoholic fatty liver disease
- Increased risk of heart disease
- Insulin resistance and diabetes risk
- Cellular aging (shortened telomeres)
- 95% increased cancer risk
That last one, by the way, was a huge systematic review of 37 large longitudinal cohort studies. Results varied depending on what, specifically, was being examined (e.g. total sugar, fructose content, sugary beverages, etc), and gave up to 200% increased cancer risk in some studies on sugary beverages, but 95% increased risk is a respectable example figure to cite here, pertaining to added sugars in foods.
And finally…
The 56 Most Common Names for Sugar (Some Are Tricky)
How many did you know?
Share This Post
-
The Gift Of Aging − by Dr. Elizabeth Eckstrom & Marcy Houle
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is, as you may gather from the title, a book about getting the most out of growing older, and doing it well.
Not all of it is positive though; some of it really is about avoiding, mitigating, or coping with the negatives that tend to come with aging.
The book is full of many (38) small self-contained chapters, so it’s well-suited to reading bit-by-bit, if so inclined. Essentially, it’s a collection of essays by the two authors, arranged into categories:
- Caring for your mind
- Caring for your body
- Caring for yourself and your family
- Caring for your soul
The first two sections are mostly self-explanatory; the third is largely about estate-planning of various kinds. The fourth is highly subjective, and/but not particularly religious, by the way. It’s largely an add-on to the “caring for your mind” mental health section, but now more specifically dealing with heavy topics such as the emotional side of mortality (as opposed to the previous section’s practical considerations of same), loss, and grief.
The style is the very low end of pop-science; facts (probably true ones; nothing seemed very contentious objectively) are stated with no sources, and there is no medical jargon that’s anything more complicated than you might find on a leaflet in a doctor’s waiting room.
Bottom line: this is a very opinion-filled book, so it’s worth reading with that in mind (i.e. their opinions may differ wildly from yours in some cases), but it’s largely informed opinions, so worth at least considering even in those cases. If nothing else, this book is certainly thought-provoking.
Click here to check out The Gift Of Aging, and enjoy the gift of aging!
Share This Post
Related Posts
-
Imposter Syndrome (and why almost everyone has it)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Imposter Syndrome (and why almost everyone has it)
Imposter syndrome is the pervasive idea that we’re not actually good enough, people think we are better than we are, and at any moment we’re going to get found out and disappoint everyone.
Beyond the workplace
Imposter syndrome is most associated with professionals. It can range from a medical professional who feels like they’ve been projecting an image of confidence too much, to a writer or musician who is sure that their next piece will never live up to the acclaim of previous pieces and everyone will suddenly realize they don’t know what they’re doing, to a middle-manager who feels like nobody above or below them realizes how little they know how to do.
But! Less talked-about (but no less prevalent) is imposter syndrome in other areas of life. New parents tend to feel this strongly, as can the “elders” of a family that everyone looks to for advice and strength and support. Perhaps worst is when the person most responsible for the finances of a household feels like everyone just trusts them to keep everything running smoothly, and maybe they shouldn’t because it could all come crashing down at any moment and everyone will see them for the hopeless shambles of a human being that they really are.
Feelings are not facts
And yet (while everyone makes mistakes sometimes) the reality is that we’re all doing our best. Given that imposter syndrome affects up to 82% of people, let’s remember to have some perspective. Everyone feels like they’re winging it sometimes. Everyone feels the pressure.
Well, perhaps not everyone. There’s that other 18%. Some people are sure they’re the best thing ever. Then again, there’s probably some in that 18% that actually feel worse than the 82%—they just couldn’t admit it, even in an anonymized study.
But one thing’s for sure: it’s very, very common. Especially in high-performing women, by the way, and people of color. In other words, people who typically “have to do twice as much to get recognized as half as good”.
That said, the flipside of this is that people who are not in any of those categories may feel “everything is in my favor, so I really have no excuse to not achieve the most”, and can sometimes take very extreme actions to try to avoid perceived failure, and it can be their family that pays the price.
Things to remember
If you find imposter syndrome nagging at you, remember these things:
- There are people far less competent than you, doing the same thing
- Nobody knows how to do everything themselves, especially at first
- If you don’t know how to do something, you can usually find out
- There is always someone to ask for help, or at least advice, or at least support
At the end of the day, we evolved to eat fruit and enjoy the sun. None of us are fully equipped for all the challenges of the modern world, but if we do our reasonable best, and look after each other (and that means that you too, dear reader, deserve looking after as well), we can all do ok.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Strategic Wellness
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Strategic Wellness: planning ahead for a better life!
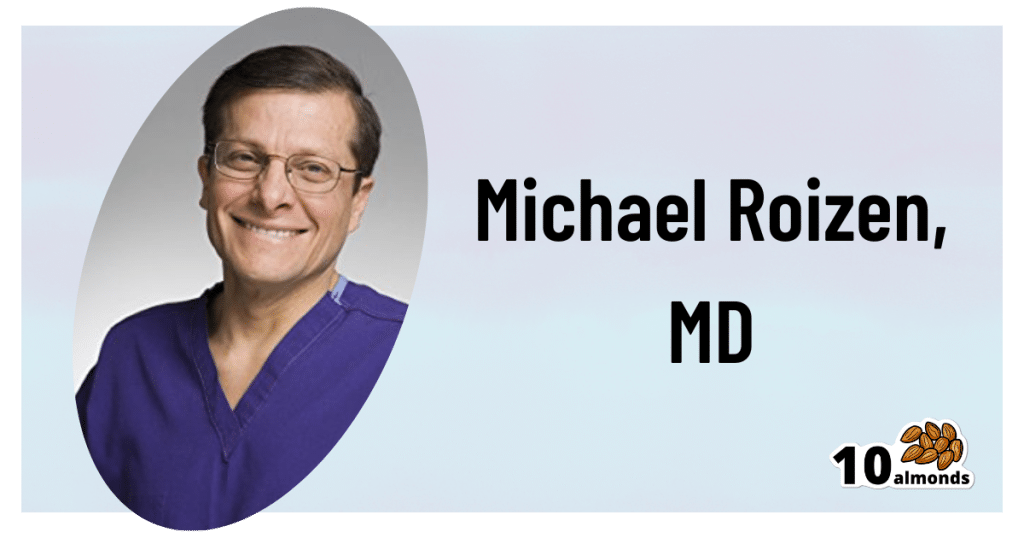
This is Dr. Michael Roizen. With hundreds of peer-reviewed publications and 14 US patents, his work has been focused on the importance of lifestyle factors in healthy living. He’s the Chief Wellness Officer at the world-famous Cleveland Clinic, and is known for his “RealAge” test and related personalized healthcare services.
If you’re curious about that, you can take the RealAge test here.
(they will require you inputting your email address if you do, though)
What’s his thing?
Dr. Roizen is all about optimizing health through lifestyle factors—most notably, diet and exercise. Of those, he is particularly keen on optimizing nutritional habits.
Is this just the Mediterranean Diet again?
Nope! Although: he does also advocate for that. But there’s more, he makes the case for what he calls “circadian eating”, optimally timing what we eat and when.
Is that just Intermittent Fasting again?
Nope! Although: he does also advocate for that. But there’s more:
Dr. Roizen takes a more scientific approach. Which isn’t to say that intermittent fasting is unscientific—on the contrary, there’s mountains of evidence for it being a healthful practice for most people. But while people tend to organize their intermittent fasting purely according to convenience, he notes some additional factors to take into account, including:
- We are evolved to eat when the sun is up
- We are evolved to be active before eating (think: hunting and gathering)
- Our insulin resistance increases as the day goes on
Now, if you’ve a quick mind about you, you’ll have noticed that this means:
- We should keep our eating to a particular time window (classic intermittent fasting), and/but that time window should be while the sun is up
- We should not roll out of bed and immediately breakfast; we need to be active for a bit first (moderate exercise is fine—this writer does her daily grocery-shopping trip on foot before breakfast, for instance… getting out there and hunting and gathering those groceries!)
- We should not, however, eat too much later in the day (so, dinner should be the smallest meal of the day)
The latter item is the one that’s perhaps biggest change for most people. His tips for making this as easy as possible include:
- Over-cater for dinner, but eat only one portion of it, and save the rest for an early-afternoon lunch
- First, however, enjoy a nutrient-dense protein-centric breakfast with at least some fibrous vegetation, for example:
- Salmon and asparagus
- Scrambled tofu and kale
- Yogurt and blueberries
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Antioxidant Matcha Snack Bars
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The antioxidants in this come not just from the matcha, but also the cacao nibs and chocolate, as well as lots of nutrients from the hazelnuts and cashews. If you’re allergic to nuts, we’ll give you substitutions that will change the nutritional profile (and flavor), but still work perfectly well and be healthy too.
You will need
For the base:
- ⅔ cup roasted hazelnuts (if allergic, substitute dessicated coconut)
- ⅔ cup chopped dates
For the main part:
- 1 cup raw cashews (if allergic, substitute raw coconut, chopped)
- ½ cup almond milk (or your preferred milk of any kind)
- ½ cup cacao nibs
- 2 tbsp lime juice
- 1 tbsp matcha powder
- 1 tbsp maple syrup (omit if you don’t care for sweetness)
For the topping (optional):
- 2oz dark chocolate, melted (and if you like, tempered—but this isn’t necessary; it’ll just make it glossier if you do)
- Spare cacao nibs, chopped nuts, or anything else you might want on there
Method
(we suggest you read everything at least once before doing anything)
1) Blend the base ingredients in a food processor until it has a coarse sticky texture, but isn’t yet a paste or dough.
2) Line a cake pan with baking paper and spread the base mix on the base; press it down to compact it a little and ensure it is flat. If there’s room, put this in the freezer while you do the next bit. If not, the fridge will suffice.
3) Blend the main part ingredients apart from the cacao nibs, until smooth. Stir in the cacao nibs with a spoon.
4) Spread the main part evenly over the base, and allow everything you’ve built (in this recipe, not in life in general) to chill in the fridge for at least 4 hours.
5) Cut it into blocks of the size and shape you want to eat them, and (if adding the optional topping) separate the blocks slightly from each other, before drizzling with the chocolate topping. Put it back in the fridge to cool this too; an hour should be sufficient.
6) Serve!
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Which Tea Is Best, By Science?
- Which Plant Milk?
- Why You Should Diversify Your Nuts!
- Cashew Nuts vs Coconut – Which is Healthier?
- Cacao vs Carob – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: