Managing Your Mortality
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Planning Is a Matter of Life and Death
Barring medical marvels as yet unrevealed, we are all going to die. We try to keep ourselves and our loved ones in good health, but it’s important to be prepared for the eventuality of death.
While this is not a cheerful topic, considering these things in advance can help us manage a very difficult thing, when the time comes.
We’ve put this under “Psychology Sunday” as it pertains to processing our own mortality, and managing our own experiences and the subsequent grief that our death may invoke in our loved ones.
We’ll also be looking at some of the medical considerations around end-of-life care, though.
Organizational considerations
It’s generally considered good to make preparations in advance. Write (or update) a Will, tie up any loose ends, decide on funerary preferences, perhaps even make arrangements with pre-funding. Life insurance, something difficult to get at a good rate towards the likely end of one’s life, is better sorted out sooner rather than later, too.
Beyond bureaucracy
What’s important to you, to have done before you die? It could be a bucket list, or it could just be to finish writing that book. It could be to heal a family rift, or to tell someone how you feel.
It could be more general, less concrete: perhaps to spend more time with your family, or to engage more with a spiritual practice that’s important to you.
Perhaps you want to do what you can to offset the grief of those you’ll leave behind; to make sure there are happy memories, or to make any requests of how they might remember you.
Lest this latter seem selfish: after a loved one dies, those who are left behind are often given to wonder: what would they have wanted? If you tell them now, they’ll know, and can be comforted and reassured by that.
This could range from “bright colors at my funeral, please” to “you have my blessing to remarry if you want to” to “I will now tell you the secret recipe for my famous bouillabaisse, for you to pass down in turn”.
End-of-life care
Increasingly few people die at home.
- Sometimes it will be a matter of fighting tooth-and-nail to beat a said-to-be-terminal illness, and thus expiring in hospital after a long battle.
- Sometimes it will be a matter of gradually winding down in a nursing home, receiving medical support to the end.
- Sometimes, on the other hand, people will prefer to return home, and do so.
Whatever your preferences, planning for them in advance is sensible—especially as money may be a factor later.
Not to go too much back to bureaucracy, but you might also want to consider a Living Will, to be enacted in the case that cognitive decline means you cannot advocate for yourself later.
Laws vary from place to place, so you’ll want to discuss this with a lawyer, but to give an idea of the kinds of things to consider:
National Institute on Aging: Preparing A Living Will
Palliative care
Palliative care is a subcategory of end-of-life care, and is what occurs when no further attempts are made to extend life, and instead, the only remaining goal is to reduce suffering.
In the case of some diseases including cancer, this may mean coming off treatments that have unpleasant side-effects, and retaining—or commencing—pain-relief treatments that may, as a side-effect, shorten life.
Euthanasia
Legality of euthanasia varies from place to place, and in some times and places, palliative care itself has been considered a form of “passive euthanasia”, that is to say, not taking an active step to end life, but abstaining from a treatment that prolongs it.
Clearer forms of passive euthanasia include stopping taking a medication without which one categorically will die, or turning off a life support machine.
Active euthanasia, taking a positive action to end life, is legal in some places and the means varies, but an overdose of barbiturates is an example; one goes to sleep and does not wake up.
It’s not the only method, though; options include benzodiazepines, and opioids, amongst others:
Efficacy and safety of drugs used for assisted dying
Unspoken euthanasia
An important thing to be aware of (whatever your views on euthanasia) is the principle of double-effect… And how it comes to play in palliative care more often than most people think.
Say a person is dying of cancer. They opt for palliative care; they desist in any further cancer treatments, and take medication for the pain. Morphine is common. Morphine also shortens life.
It’s common for such a patient to have a degree of control over their own medication, however, after a certain point, they will no longer be in sufficient condition to do so.
After this point, it is very common for caregivers (be they medical professionals or family members) to give more morphine—for the purpose of reducing suffering, of course, not to kill them.
In practical terms, this often means that the patient will die quite promptly afterwards. This is one of the reasons why, after sometimes a long-drawn-out period of “this person is dying”, healthcare workers can be very accurate about “it’s going to be in the next couple of days”.
The take-away from this section is: if you would like for this to not happen to you or your loved one, you need to be aware of this practice in advance, because while it’s not the kind of thing that tends to make its way into written hospital/hospice policies, it is very widespread and normalized in the industry on a human level.
Further reading: Goods, causes and intentions: problems with applying the doctrine of double effect to palliative sedation
One last thing…
Planning around our own mortality is never a task that seems pressing, until it’s too late. We recommend doing it anyway, without putting it off, because we can never know what’s around the corner.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Covering obesity: 6 tips for dispelling myths and avoiding stigmatizing news coverage
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When researchers looked at news coverage of obesity in the United States and the United Kingdom a few years ago, they found that images in news articles often portrayed people with larger bodies “in a stigmatizing manner” — they emphasized people’s abdomens, for example, or showed them eating junk food, wearing tight clothes or lounging in front of a TV.
When people with larger bodies were featured in photos and videos, nearly half were shown only from their necks down or with part of their heads missing, according to the analysis, published in November 2023. The researchers examined a total of 445 images posted to the websites of four U.S. news outlets and four U.K. news outlets between August 2018 and August 2019.
The findings underscore the need for dramatic changes in the way journalists report on obesity and people who weigh more than what medical authorities generally consider healthy, Rebecca Puhl, one of the paper’s authors, told The Journalist’s Resource in an email interview.
“Using images of ‘headless stomachs’ is dehumanizing and stigmatizing, as are images that depict people with larger bodies in stereotypical ways (e.g., eating junk food or being sedentary),” wrote Puhl, deputy director of the Rudd Center for Food Policy and Health at the University of Connecticut and a leading scholar on weight stigma.
She noted that news images influence how the public views and interacts with people with obesity, a complicated and often misunderstood condition that the American Medical Association considers a disease.
In the U.S., an estimated 42% of adults aged 20 years and older have obesity, a number researchers predict will rise to 50% over the next six years. While the disease isn’t as common in other parts of the planet, the World Obesity Federation projects that by 2035, more than half the global population will have obesity or overweight.
Several other studies Puhl has conducted demonstrate that biased new images can have damaging consequences for individuals affected by obesity.
“Our research has found that seeing the stigmatizing image worsens people’s attitudes and weight bias, leading them to attribute obesity to laziness, increasing their dislike of people with higher weight, and increasing desire for social distance from them,” Puhl explained.
Dozens of studies spotlight problems in news coverage of obesity in the U.S. and abroad. In addition to stigmatizing images, journalists use stigmatizing language, according to a 2022 research review in eClinicalMedicine, a journal published by The Lancet.
The research also suggests people with higher weights feel excluded and ridiculed by news outlets.
“Overt or covert discourses in news media, social media, and public health campaigns included depictions of people with overweight or obesity as being lazy, greedy, undisciplined, unhappy, unattractive, and stupid,” write the authors of the review, which examines 113 academic studies completed before Dec. 2, 2021.
To help journalists reflect on and improve their work, The Journalist’s Resource asked for advice from experts in obesity, weight stigma, health communication and sociolinguistics. They shared their thoughts and opinions, which we distilled into the six tips that appear below.
In addition to Puhl, we interviewed these six experts:
Jamy Ard, a professor of epidemiology and prevention at Wake Forest University School of Medicine and co-director of the Wake Forest Baptist Health Weight Management Center. He’s also president of The Obesity Society, a professional organization of researchers, health care providers and other obesity specialists.
Leslie Cofie, an assistant professor of health education and promotion at East Carolina University’s College of Health and Human Performance. He has studied obesity among immigrants and military veterans.
Leslie Heinberg, director of Enterprise Weight Management at the Cleveland Clinic, an academic medical center. She’s also vice chair for psychology in the Cleveland Clinic’s Center for Behavioral Health Department of Psychiatry and Psychology.
Monu Khanna, a physician in Missouri who is board certified in obesity medicine.
Jenn Lonzer, manager of the Cleveland Clinic Health Library and the co-author of several academic papers on health communication.
Cindi SturtzSreetharan, an anthropologist and professor at the Arizona State University School of Human Evolution and Social Change. She studies the language people of different cultures use to describe human bodies.
1. Familiarize yourself with recent research on what causes obesity and how obesity can affect a person’s health. Many long-held beliefs about the disease are wrong.
Journalists often report incorrect or misleading information about obesity, possibly because they’re unaware that research published in recent decades dispels many long-held beliefs about the disease, the experts say. Obesity isn’t simply the result of eating too many calories and doing too little exercise. A wide range of factors drive weight gain and prevent weight loss, many of which have nothing to do with willpower or personal choices.
Scholars have learned that stress, gut health, sleep duration and quality, genetics, medication, personal income, access to healthy foods and even climate can affect weight regulation. Prenatal and early life experiences also play a role. For example, childhood trauma such as child abuse can become “biologically embedded,” altering children’s brain structures and influencing their long-term physical and mental health, according to a 2020 research review published in the journal Physiology & Behavior.
“The causes of obesity are numerous and each individual with obesity will have a unique set of contributors to their excess weight gain,” Jamy Ard, president of The Obesity Society, wrote to The Journalist’s Resource.
The experts urge journalists to help dispel myths, correct misinformation and share new research findings. News outlets should examine their own work, which often “ignores the science and sets up situation blaming,” says Leslie Heinberg, director of Enterprise Weight Management at the Cleveland Clinic.
“So much of the media portrayal is simply ‘This is a person who eats too much and the cure is simply to eat less or cut out that food’ or something overly, overly simplistic,” Heinberg says.
Journalists need to build their knowledge of the problem before they can explain it to their audiences. Experts point out that educating policymakers, health care providers and the public about obesity is key to eliminating the stigma associated with having a larger body.
Weight stigma alone is so physically and emotionally damaging that 36 international experts issued a consensus statement in 2020 to raise awareness about it. The document, endorsed by dozens of medical and academic organizations, outlines 13 recommendations for eliminating weight bias and stigma.
Recommendation No. 5: “We call on the media to produce fair, accurate, and non-stigmatizing portrayals of obesity. A commitment from the media is needed to shift the narrative around obesity.”
2. Use person-first language — the standard among health and medical professionals for communicating about people with chronic diseases.
The experts we interviewed encourage journalists to ditch the adjectives “obese” and “overweight” because they are dehumanizing. Use person-first language, which avoids labeling people as their disease by putting the person before the disease.
Instead of saying “an obese teenager,” say “a teenager who has obesity” or “a teenager affected by obesity.” Instead of writing “overweight men,” write “men who have overweight.”
Jenn Lonzer, manager of the Cleveland Clinic Health Library, says using “overweight” as a noun might look and sound awkward at first. But it makes sense considering other diseases are treated as nouns, she notes. Journalists would not typically refer to someone in a news story as “a cancerous person,” for example. They would report that the individual has cancer.
It’s appropriate to refer to people with overweight or obesity using neutral weight terminology. Puhl wrote that she uses “people with higher body weight” or “people with high weight” and, sometimes, “people with larger bodies” in her own writing.
While the Associated Press stylebook offers no specific guidance on the use of terms such as “obese” or “overweight,” it advises against “general and often dehumanizing ‘the’ labels such as the poor, the mentally ill, the disabled, the college-educated.”
The Association of Health Care Journalists recommends person-first language when reporting on obesity. But it also advises journalists to ask sources how they would like to be characterized, provided their weight or body size is relevant to the news story.
Anthropologist Cindi SturtzSreetharan, who studies language and culture, says sources’ responses to that question should be part of the story. Some individuals might prefer to be called “fat,” “thick” or “plus-sized.”
“I would include that as a sentence in the article — to signal you’ve asked and that’s how they want to be referred to,” SturtzSreetharan says.
She encourages journalists to read how authors describe themselves in their own writing. Two books she recommends: Thick by Tressie McMillan Cottom and Heavy: An American Memoir by Kiese Laymon.
3. Carefully plan and choose the images that will accompany news stories about obesity.
Journalists need to educate themselves about stigma and screen for it when selecting images, Puhl noted. She shared these four questions that journalists should ask themselves when deciding how to show people with higher weights in photos and video.
- Does the image imply or reinforce negative stereotypes?
- Does it provide a respectful portrayal of the person?
- Who might be offended, and why?
- Can an alternative image convey the same message and eliminate possible bias?
“Even if your written piece is balanced, accurate, and respectful, a stigmatizing image can undermine your message and promote negative societal attitudes,” Puhl wrote via email.
Lonzer says newsrooms also need to do a better job incorporating images of people who have different careers, interests, education levels and lifestyles into their coverage of overweight and obesity.
“We are diverse,” says Lonzer, who has overweight. “We also have diversity in body shape and size. It’s good to have images that reflect what Americans look like.”
If you’re looking for images and b-roll videos that portray people with obesity in non-stigmatizing ways, check out the Rudd Center Media Gallery. It’s a collection of original images of people from various demographic groups that journalists can use for free in their coverage.
The Obesity Action Coalition, a nonprofit advocacy organization, also provides images. But journalists must sign up to use the OAC Bias-Free Image Gallery.
Other places to find free images: The World Obesity Image Bank, a project of the World Obesity Federation, and the Flickr account of Obesity Canada.
4. Make sure your story does not reinforce stereotypes or insinuate that overcoming obesity is simply a matter of cutting calories and doing more exercise.
“Think about the kinds of language used in the context of eating habits or physical activity, as some can reinforce shame or stereotypes,” Puhl wrote.
She suggested journalists avoid phrases such as “resisting temptations,” “cheating on a diet,” “making excuses,” “increasing self-discipline” and “lacking self-control” because they perpetuate the myth that individuals can control their weight and that the key to losing weight is eating less and moving more.
Lonzer offers this advice: As you work on stories about obesity or weight-related issues, ask yourself if you would use the same language and framing if you were reporting on someone you love.
Here are other questions for journalists to contemplate:
“Am I treating this as a complex medical condition or am I treating it as ‘Hey, lay off the French fries?’” Lonzer adds. “Am I treating someone with obesity differently than someone with another disease?”
It’s important to also keep in mind that having excess body fat does not, by itself, mean a person is unhealthy. And don’t assume everyone who has a higher weight is unhappy about it.
“Remember, not everyone with obesity is suffering,” physician Monu Khanna wrote to The Journalist’s Resource.
5. To help audiences understand how difficult it is to prevent and reduce obesity, explain that even the places people live can affect their waistlines.
When news outlets report on obesity, they often focus on weight-loss programs, surgical procedures and anti-obesity medications. But there are other important issues to cover. Experts stress the need to help the public understand how factors not ordinarily associated with weight gain or loss can influence body size.
For example, a paper published in 2018 in the American Journal of Preventive Medicine indicates adults who are regularly exposed to loud noise have a higher waist circumference than adults who are not. Research also finds that people who live in neighborhoods with sidewalks and parks are more active.
“One important suggestion I would offer to journalists is that they need to critically explore environmental factors (e.g., built environment, food deserts, neighborhood safety, etc.) that lead to disproportionately high rates of obesity among certain groups, such as low-income individuals and racial/ethnic minorities,” Leslie Cofie, an assistant professor at East Carolina University, wrote to The Journalist’s Resource.
Cofie added that moving to a new area can prompt weight changes.
“We know that immigrants generally have lower rates of obesity when they first migrate to the U.S.,” he wrote. “However, over time, their obesity rates resemble that of their U.S.-born counterparts. Hence, it is critical for journalists to learn about how the sociocultural experiences of immigrants change as they adapt to life in the U.S. For example, cultural perspectives about food, physical activities, gender roles, etc. may provide unique insights into how the pre- and post-migration experiences of immigrants ultimately contribute to the unfavorable trends in their excessive weight gain.”
Other community characteristics have been linked to larger body sizes for adults or children: air pollution, lower altitudes, higher temperatures, lower neighborhood socioeconomic status, perceived neighborhood safety, an absence of local parks and closer proximity to fast-food restaurants.
6. Forge relationships with organizations that study obesity and advocate on behalf of people living with the disease.
Several organizations are working to educate journalists about obesity and help them improve their coverage. Five of the most prominent ones collaborated on a 10-page guide book, “Guidelines for Media Portrayals of Individuals Affected by Obesity.”
- The Rudd Center for Food Policy and Health, based at the University of Connecticut, “promotes solutions to food insecurity, poor diet quality, and weight bias through research and policy,” according to its website. Research topics include food and beverage marketing, weight-related bullying and taxes on sugary drinks.
- The Obesity Society helps journalists arrange interviews with obesity specialists. It also offers journalists free access to its academic journal, Obesity, and free registration to ObesityWeek, an international conference of researchers and health care professionals held every fall. This year’s conference is Nov. 2-6 in San Antonio, Texas.
- The Obesity Medicine Association represents health care providers who specialize in obesity treatment and care. It also helps journalists connect with obesity experts and offers, on an individual basis, free access to its events, including conferences and Obesity Medicine Fundamentals courses.
- The Obesity Action Coalition offers free access to its magazine, Weight Matters, and guides on weight bias at work and in health care.
- The American Society for Metabolic and Bariatric Surgery represents surgeons and other health care professionals who work in the field of metabolic and bariatric surgery. It provides the public with resources such as fact sheets and brief explanations of procedures such as the Roux-en-Y Gastric Bypass.
For further reading
Weight Stigma in Online News Images: A Visual Content Analysis of Stigma Communication in the Depictions of Individuals with Obesity in U.S. and U.K. News
Aditi Rao, Rebecca Puhl and Kirstie Farrar. Journal of Health Communication, November 2023.Influence and Effects of Weight Stigmatization in Media: A Systematic Review
James Kite; et al. eClinicalMedicine, June 2022.Has the Prevalence of Overweight, Obesity and Central Obesity Leveled Off in the United States? Trends, Patterns, Disparities, and Future Projections for the Obesity Epidemic
Youfa Wang; et al. International Journal of Epidemiology, June 2020.This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Share This Post
-
Managing [E-word] Dysfunction Reactions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
We had several requests pertaining to veganism, meatless mondays, and substitutions in recipes—so we’re going to cover those on a different day!
As for questions we’re answering today…
Q: Information on [e-word] dysfunction for those who have negative reactions to [the most common medications]?
When it comes to that particular issue, one or more of these three factors are often involved:
- Hormones
- Circulation
- Psychology
The most common drugs (that we can’t name here) work on the circulation side of things—specifically, by increasing the localized blood pressure. The exact mechanism of this drug action is interesting, albeit beyond the scope of a quick answer here today. On the other hand, the way that they work can cause adverse blood-pressure-related side effects for some people; perhaps you’re one of them.
To take matters into your own hands, so to speak, you can address each of those three things we just mentioned:
Hormones
Ask your doctor (or a reputable phlebotomy service) for a hormone test. If your free/serum testosterone levels are low (which becomes increasingly common in men over the age of 45), they may prescribe something—such as testosterone shots—specifically for that.
This way, it treats the underlying cause, rather than offering a workaround like those common pills whose names we can’t mention here.
Circulation
Look after your heart health; eat for your heart health, and exercise regularly!
Cold showers/baths also work wonders for vascular tone—which is precisely what you need in this matter. By rapidly changing temperatures (such as by turning off the hot water for the last couple of minutes of your shower, or by plunging into a cold bath), your blood vessels will get practice at constricting and maintaining that constriction as necessary.
Psychology
[E-word] dysfunction can also have a psychological basis. Unfortunately, this can also then be self-reinforcing, if recalling previous difficulties causes you to get distracted/insecure and lose the moment. One of the best things you can do to get out of this catch-22 situation is to not worry about it in the moment. Depending on what you and your partner(s) like to do in bed, there are plenty of other equally respectable options, so just switch track!
Having a conversation about this in advance will probably be helpful, so that everyone’s on the same page of the script in that eventuality, and it becomes “no big deal”. Without that conversation, misunderstandings and insecurities could arise for your partner(s) as well as yourself (“aren’t I desirable enough?” etc).
So, to recap, we recommend:
- Have your hormones checked
- Look after your circulation
- Make the decision to have fun!
Share This Post
-
Can you get sunburnt or UV skin damage through car or home windows?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When you’re in a car, train or bus, do you choose a seat to avoid being in the sun or do you like the sunny side?
You can definitely feel the sun’s heat through a window. But can you get sunburn or skin damage when in your car or inside with the windows closed?
Let’s look at how much UV (ultraviolet) radiation passes through different types of glass, how tinting can help block UV, and whether we need sunscreen when driving or indoors.
Zac Harris/Unsplash What’s the difference between UVA and UVB?
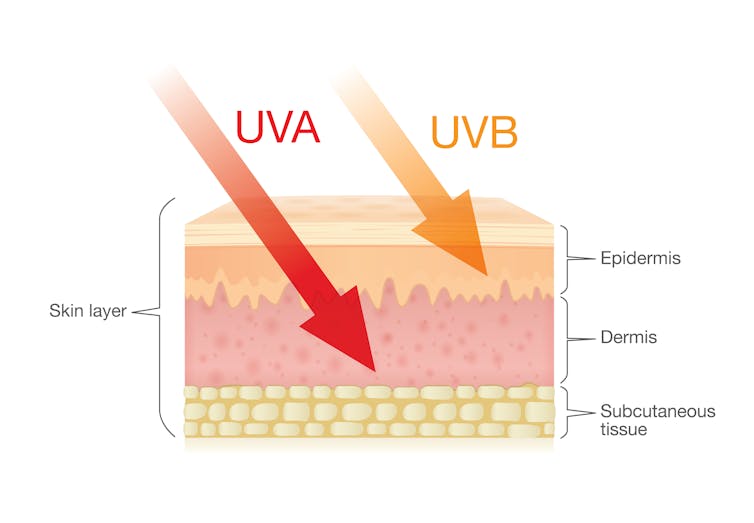
Of the total UV radiation that reaches Earth, about 95% is UVA and 5% is UVB.
UVB only reaches the upper layers of our skin but is the major cause of sunburn, cataracts and skin cancer.
UVA penetrates deeper into our skin and causes cell damage that leads to skin cancer.
UVA penetrates deeper than UVB. Shutterstock/solar22 Glass blocks UVA and UVB radiation differently
All glass used in house, office and car windows completely blocks UVB from passing through.
But only laminated glass can completely block UVA. UVA can pass through other glass used in car, house and office windows and cause skin damage, increasing the risk of cancer.
Car windscreens block UVA, but the side and rear windows don’t
A car’s front windscreen lets in lots of sunshine and light. Luckily it blocks 98% of UVA radiation because it is made of two layers of laminated glass.
But the side and rear car windows are made of tempered glass, which doesn’t completely block UVA. A study of 29 cars found a range from 4% to almost 56% of UVA passed through the side and rear windows.
The UVA protection was not related to the car’s age or cost, but to the type of glass, its colour and whether it has been tinted or coated in a protective film. Grey or bronze coloured glass, and window tinting, all increase UVA protection. Window tinting blocks around 95% of UVA radiation.
In a separate study from Saudi Arabia, researchers fitted drivers with a wearable radiation monitor. They found drivers were exposed to UV index ratings up to 3.5. (In Australia, sun protection is generally recommended when the UV index is 3 or above – at this level it takes pale skin about 20 minutes to burn.)
So if you have your windows tinted, you should not have to wear sunscreen in the car. But without tinted windows, you can accumulate skin damage.
UV exposure while driving increases skin cancer risk
Many people spend a lot of time in the car – for work, commuting, holiday travel and general transport. Repeated UVA radiation exposure through car side windows might go unnoticed, but it can affect our skin.
Indeed, skin cancer is more common on the driver’s side of the body. A study in the United States (where drivers sit on the left side) found more skin cancers on the left than the right side for the face, scalp, arm and leg, including 20 times more for the arm.
Another US study found this effect was higher in men. For melanoma in situ, an early form of melanoma, 74% of these cancers were on the on the left versus 26% on the right.
Earlier Australian studies reported more skin damage and more skin cancer on the right side.
Cataracts and other eye damage are also more common on the driver’s side of the body.
What about UV exposure through home or office windows?
We see UV damage from sunlight through our home windows in faded materials, furniture or plastics.
Most glass used in residential windows lets a lot of UVA pass through, between 45 and 75%.
Residential windows can let varied amounts of UVA through. Sherman Trotz/Pexels Single-pane glass lets through the most UVA, while thicker, tinted or coated glass blocks more UVA.
The best options are laminated glass, or double-glazed, tinted windows that allow less than 1% of UVA through.
Skylights are made from laminated glass, which completely stops UVA from passing through.
Most office and commercial window glass has better UVA protection than residential windows, allowing less than 25% of UVA transmission. These windows are usually double-glazed and tinted, with reflective properties or UV-absorbent chemicals.
Some smart windows that reduce heat using chemical treatments to darken the glass can also block UVA.
So when should you wear sunscreen and sunglasses?
The biggest risk with skin damage while driving is having the windows down or your arm out the window in direct sun. Even untinted windows will reduce UVA exposure to some extent, so it’s better to have the car window up.
For home windows, window films or tint can increase UVA protection of single pane glass. UVA blocking by glass is similar to protection by sunscreen.
When you need to use sunscreen depends on your skin type, latitude and time of the year. In a car without tinted windows, you could burn after one hour in the middle of the day in summer, and two hours in the middle of a winter’s day.
But in the middle of the day next to a home window that allows more UVA to pass through, it could take only 30 minutes to burn in summer and one hour in winter.
When the UV index is above three, it is recommended you wear protective sunglasses while driving or next to a sunny window to avoid eye damage.
Theresa Larkin, Associate Professor of Medical Sciences, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Radishes vs Carrots – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing radishes to carrots, we picked the carrots.
Why?
In terms of macros, carrots have more fiber and carbs; the two root vegetables both have comparable (low) glycemic indices, so we’re saying that the one with more fiber wins, and that’s carrots.
In the category of vitamins, radishes have more of vitamins B9 and C, while carrots have more of vitamins A, B1, B2, B3, B5, B6, E, K, and choline. An easy win for carrots.
When it comes to minerals, radishes have more selenium, while carrots have more calcium, magnesium, manganese, phosphorus, and potassium. Another clear win for carrots.
In terms of polyphenols, radishes do have some, but carrots have more, and thus win this category too.
All in all, enjoy either or both, but carrots deliver the most nutrients by far!
Want to learn more?
You might like to read:
What Do The Different Kinds Of Fiber Do? 30 Foods That Rank Highest
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Which Sugars Are Healthier, And Which Are Just The Same?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From Apples to Bees, and High-Fructose Cs
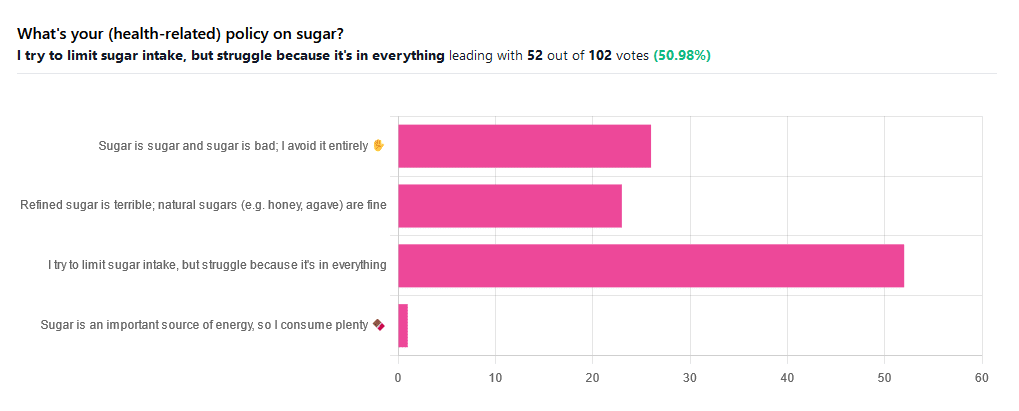
We asked you for your (health-related) policy on sugar. The trends were as follows:
- About half of all respondents voted for “I try to limit sugar intake, but struggle because it’s in everything”
- About a quarter of all respondents voted for “Refined sugar is terrible; natural sugars (e.g. honey, agave) are fine”
- About a quarter of all respondents voted for “Sugar is sugar and sugar is bad; I avoid it entirely”
- One (1) respondent voted for “Sugar is an important source of energy, so I consume plenty”
Writer’s note: I always forget to vote in these, but I’d have voted for “I try to limit sugar intake, but struggle because it’s in everything”.
Sometimes I would like to make my own [whatever] to not have the sugar, but it takes so much more time, and often money too.
So while I make most things from scratch (and typically spend about an hour cooking each day), sometimes store-bought is the regretfully practical timesaver/moneysaver (especially when it comes to condiments).
So, where does the science stand?
There has, of course, been a lot of research into the health impact of sugar.
Unfortunately, a lot of it has been funded by sugar companies, which has not helped. Conversely, there are also studies funded by other institutions with other agendas to push, and some of them will seek to make sugar out to be worse than it is.
So for today’s mythbusting overview, we’ve done our best to quality-control studies for not having financial conflicts of interest. And of course, the usual considerations of favoring high quality studies where possible Large sample sizes, good method, human subjects, that sort of thing.
Sugar is sugar and sugar is bad: True or False?
False and True, respectively.
- Sucrose is sucrose, and is generally bad.
- Fructose is fructose, and is worse.
Both ultimately get converted into glycogen (if not used immediately for energy), but for fructose, this happens mostly* in the liver, which a) taxes it b) goes very unregulated by the pancreas, causing potentially dangerous blood sugar spikes.
This has several interesting effects:
- Because fructose doesn’t directly affect insulin levels, it doesn’t cause insulin insensitivity (yay)
- Because fructose doesn’t directly affect insulin levels, this leaves hyperglycemia untreated (oh dear)
- Because fructose is metabolized by the liver and converted to glycogen which is stored there, it’s one of the main contributors to non-alcoholic fatty liver disease (at this point, we’re retracting our “yay”)
Read more: Fructose and sugar: a major mediator of non-alcoholic fatty liver disease
*”Mostly” in the liver being about 80% in the liver. The remaining 20%ish is processed by the kidneys, where it contributes to kidney stones instead. So, still not fabulous.
Fructose is very bad, so we shouldn’t eat too much fruit: True or False?
False! Fruit is really not the bad guy here. Fruit is good for you!
Fruit does contain fructose yes, but not actually that much in the grand scheme of things, and moreover, fruit contains (unless you have done something unnatural to it) plenty of fiber, which mitigates the impact of the fructose.
- A medium-sized apple (one of the most sugary fruits there is) might contain around 11g of fructose
- A tablespoon of high-fructose corn syrup can have about 27g of fructose (plus about 3g glucose)
Read more about it: Effects of high-fructose (90%) corn syrup on plasma glucose, insulin, and C-peptide in non-insulin-dependent diabetes mellitus and normal subjects
However! The fiber content (in fruit) mitigates the impact of the fructose almost entirely anyway.
And if you take fruits that are high in sugar and/but high in polyphenols, like berries, they now have a considerable net positive impact on glycemic health:
- Polyphenols and Glycemic Control
- Polyphenols and their effects on diabetes management: A review
- Dietary polyphenols as antidiabetic agents: Advances and opportunities
You may be wondering: what was that about “unless you have done something unnatural to it”?
That’s mostly about juicing. Juicing removes much (or all) of the fiber, and if you do that, you’re basically back to shooting fructose into your veins:
- Effect of Fruit Juice on Glucose Control and Insulin Sensitivity in Adults: A Meta-Analysis of 12 Randomized Controlled Trials
- Intake of Fruit, Vegetables, and Fruit Juices and Risk of Diabetes in Women
Natural sugars like honey, agave, and maple syrup, are healthier than refined sugars: True or False?
True… Sometimes, and sometimes marginally.
This is partly because of the glycemic index and glycemic load. The glycemic index scores tail off thus:
- table sugar = 65
- maple syrup = 54
- honey = 46
- agave syrup = 15
So, that’s a big difference there between agave syrup and maple syrup, for example… But it might not matter if you’re using a very small amount, which means it may have a high glycemic index but a low glycemic load.
Note, incidentally, that table sugar, sucrose, is a disaccharide, and is 50% glucose and 50% fructose.
The other more marginal health benefits come from that fact that natural sugars are usually found in foods high in other nutrients. Maple syrup is very high in manganese, for example, and also a fair source of other minerals.
But… Because of its GI, you really don’t want to be relying on it for your nutrients.
Wait, why is sugar bad again?
We’ve been covering mostly the more “mythbusting” aspects of different forms of sugar, rather than the less controversial harms it does, but let’s give at least a cursory nod to the health risks of sugar overall:
- Obesity and associated metabolic risk
- Main contributor to non-alcoholic fatty liver disease
- Increased risk of heart disease
- Insulin resistance and diabetes risk
- Cellular aging (shortened telomeres)
- 95% increased cancer risk
That last one, by the way, was a huge systematic review of 37 large longitudinal cohort studies. Results varied depending on what, specifically, was being examined (e.g. total sugar, fructose content, sugary beverages, etc), and gave up to 200% increased cancer risk in some studies on sugary beverages, but 95% increased risk is a respectable example figure to cite here, pertaining to added sugars in foods.
And finally…
The 56 Most Common Names for Sugar (Some Are Tricky)
How many did you know?
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Bath vs Shower – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing bathing to showering, we picked the shower.
Why?
For the basic task of getting your body clean, the shower is better as it is an entirely one-way process. Clean water hits your body, dirty water leaves it, and no dirt is making its way back.
Baths do not have this advantage, and if you enter a bath dirty, you will then be sitting in dirty water. You will leave it a lot cleaner than you entered it (because a lot of the dirt stayed in the bathwater to be drained away after the bath), but not as clean as if you had showered.
One could argue soap or equivalent will prevent the dirt re-sticking, and that’s true, but it’s true for soap in the shower too, so it doesn’t offset anything.
Additionally, being immersed in water for more than 15 minutes can start to have a (paradoxically) dehydrating effect on the skin; this happens not only because of losing skin oils to the water, but also because of osmosis, the resultant mild edema, the body’s homeostatic response to the mild edema, then getting out the bath and drying, leaving one with the response having now just caused dehydrated skin.
Baths do have some health advantages! And these come primarily from the mental health benefits of relaxation in warm water and/or generally pampering oneself. Additionally, some bath oils or bath salts can be beneficial in a way that couldn’t be administered the same way in the shower.
Best of both worlds?
In some parts of the world (Thailand and Turkey come to mind; doubtlessly there are many others) there are traditions of first taking a shower to get clean, and then taking a bath for the rest of the bathing experience. As a bonus, the bathing experience is then all the more pleasant for the water remaining just as clean as it was to start with.
However, if you do have to pick one (and for the purpose of our “This or That” exercise, we do), then it’s the shower, hands-down.
Want to read more?
You might want to also take into account how it’s still possible to have too much of a good thing:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: