Metformin For Weight-Loss & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Metformin Without Diabetes?
Metformin is a diabetes drug; it works by:
- decreasing glucose absorption from the gut
- decreasing glucose production in the liver
- increasing glucose sensitivity
It doesn’t change how much insulin is secreted, and is unlikely to cause hypoglycemia, making it relatively safe as diabetes drugs go.
It’s a biguanide drug, and/but so far as science knows (so far), its mechanism of action is unique (i.e. no other drug works the same way that metformin does).
Today we’ll examine its off-label uses and see what the science says!
A note on terms: “off-label” = when a drug is prescribed to treat something other than the main purpose(s) for which the drug was approved.
Other examples include modafinil against depression, and beta-blockers against anxiety.
Why take it if not diabetic?
There are many reasons people take it, including just general health and life extension:
However, its use was originally expanded (still “off-label”, but widely prescribed) past “just for diabetes” when it showed efficacy in treating pre-diabetes. Here for example is a longitudinal study that found metformin use performed similarly to lifestyle interventions (e.g. diet, exercise, etc). In their words:
❝ Lifestyle intervention or metformin significantly reduced diabetes development over 15 years. There were no overall differences in the aggregate microvascular outcome between treatment groups❞
But, it seems it does more, as this more recent review found:
❝Long-term weight loss was also seen in both [metformin and intensive lifestyle intervention] groups, with better maintenance under metformin.
Subgroup analyses from the DPP/DPPOS have shed important light on the actions of metformin, including a greater effect in women with prior gestational diabetes, and a reduction in coronary artery calcium in men that might suggest a cardioprotective effect.
Long-term diabetes prevention with metformin is feasible and is supported in influential guidelines for selected groups of subjects.❞
Source: Metformin for diabetes prevention: update of the evidence base
We were wondering about that cardioprotective effect, so…
Cardioprotective effect
In short, another review (published a few months after the above one) confirmed the previous findings, and also added:
❝Patients with BMI > 35 showed an association between metformin use and lower incidence of CVD, including African Americans older than age 65. The data suggest that morbidly obese patients with prediabetes may benefit from the use of metformin as recommended by the ADA.❞
We wondered about the weight loss implications of this, and…
For weight loss
The short version is, it works:
- Effectiveness of metformin on weight loss in non-diabetic individuals with obesity
- Metformin for weight reduction in non-diabetic patients: a systematic review and meta-analysis
- Metformin induces weight loss associated with gut microbiota alteration in non-diabetic obese women
…and many many more where those came from. As a point of interest, it has also been compared and contrasted to GLP-1 agonists.
Compared/contrasted with GLP-1 agonists
It’s not quite as effective for weight loss, and/but it’s a lot cheaper, is tablets rather than injections, has fewer side effects (for most people), and doesn’t result in dramatic yoyo-ing if there’s an interruption to taking it:
Or if you prefer a reader-friendly pop-science version:
Ozempic vs Metformin: Comparing The Two Diabetes Medications
Is it safe?
For most people yes, but there are a stack of contraindications, so it’s best to speak with your doctor. However, particular things to be aware of include:
- Usually contraindicated if you have kidney problems of any kind
- Usually contraindicated if you have liver problems of any kind
- May be contraindicated if you have issues with B12 levels
See also: Metformin: Is it a drug for all reasons and diseases?
Where can I get it?
As it’s a prescription-controlled drug, we can’t give you a handy Amazon link for this one.
However, many physicians are willing to prescribe it for off-label use (i.e., for reasons other than diabetes), so speak with yours (telehealth options may also be available).
If you do plan to speak with your doctor and you’re not sure they’ll be agreeable, you might want to get this paper and print it to take it with you:
Off-label indications of Metformin – Review of Literature
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Nutrition To Combat Lymphedema & Lipedema
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Kelly Sturm is a rehab specialist (Doctor of Physical Therapy), and also a certified lymphedema therapist. Here’s what helps her patients with lymphedema and lipedema:
Don’t fan the flames
Lymphedema and lipedema are inflammatory lymphatic diseases affecting mostly women. As such, an anti-inflammatory diet will be important, but there are other factors too:
- Anti-inflammatory diet: this is to reduce the chronic inflammation associated with lymphatic diseases. This means eating plenty of fruit and vegetables, especially berries and leafy greens, and avoiding things like sugar, alcohol, caffeine, and processed foods. And of course, don’t smoke.
- Intermittent fasting: this also helps by giving the body a chance to correct itself; when the body isn’t digesting food, it has a lot more resources to devote to its favorite activity: maintenance. This results in lower inflammation, and better fat redistribution.
- Weight loss: not a bandwagon we often get on at 10almonds as it’s rarely the most important thing, but in this case it is of high importance (second only to dealing with the inflammation), as excess weight around the lymph nodes and vessels can lead to dysfunction and swelling. Thus, reducing the weight can ease that and allow the body to heal.
For more details on all of the above, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Eat To Beat Inflammation ← also some non-dietary advice in there too
- Ask Not What Your Lymphatic System Can Do For You…
- Lose Weight, But Healthily ← more useful than just trying to run a calorie deficit
Take care!
Share This Post
-
The Best Form Of Sugar During Exercise
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝What is the best form of sugar for an energy kick during exercise? Both type of sugar eg glicoae fructose dextrose etc and medium, ie drink, gel, solids etc❞
Great question! Let’s be clear first that we’re going to answer this specifically for the context of during exercise.
Because, if you’re not actively exercising strenuously right at the time when you’re taking the various things we’re going to be talking about, the results will not be the same.
For scenarios that are anything less than “I am exercising right now and my muscles (not joints, or anything else) are feeling the burn”, then instead please see this:
Snacks & Hacks: Eating For Energy (In Ways That Actually Work)
Because, to answer your question, we’re going to be going 100% against the first piece of advice in that article, which was “Skip the quasi-injectables”, i.e., anything marketed as very quick release. Those things are useful for diabetics to have handy just in case of needing to urgently correct a hypo, but for most people most of the time, they’re not. See also:
Which Sugars Are Healthier, And Which Are Just The Same?
However…
When strenuously exercising in a way that is taxing our muscles, we do not have to worry about the usual problem of messing up our glucose metabolism by overloading our body with sugars faster than it can use it (thus: it has to hurriedly convert glucose and shove it anywhere it’ll fit to put it away, which is very bad for us), because right now, in the exercise scenario we’re describing, the body is already running its fastest metabolism and is grabbing glucose anywhere it can find it.
Which brings us to our first key: the best type of sugar for this purpose is glucose. Because:
- glucose: the body can use immediately and easily convert whatever’s spare to glycogen (a polysaccharide of glucose) for storage
- fructose: the body cannot use immediately and any conversion of fructose to glycogen has to happen in the liver, so if you take too much fructose (without anything to slow it down, such as the fiber in whole fruit), you’re not only not going to get usable energy (the sugar is just going to be there in your bloodstream, circulating, not getting used, because it doesn’t trigger insulin release and insulin is the gatekeeper that allows sugar to be used), but also, it’s going to tax the liver, which if done to excess, is how we get non-alcoholic fatty liver disease.
- sucrose: is just a disaccharide of glucose and fructose, so it first gets broken down into those, and then its constituent parts get processed as above. Other disaccharides you’ll see mentioned sometimes are maltose and lactose, but again, they’re just an extra step removed from useful metabolism, so to save space, we’ll leave it at that for those today.
- dextrose: is just glucose, but when the labeller is feeling fancy. It’s technically informational because it specifies what isomer of glucose it is, but basically all glucose found in food is d-glucose, i.e. dextrose. Other isomers of glucose can be synthesized (very expensively) in laboratories or potentially found in obscure places (the universe is vast and weird), but in short: unless someone’s going to extreme lengths to get something else, all glucose we encounter is dextrose, and all (absolutely all) dextrose is glucose.
We’d like to show scientific papers contesting these head-to-head for empirical proof, but since the above is basic chemistry and physiology, all we could find is papers taking this for granted and stating in their initial premise that sports drinks, gels, bars usually contain glucose as their main sugar, potentially with some fructose and sucrose. Like this one:
A Comprehensive Study on Sports and Energy Drinks
As for how to take it, again this is the complete opposite of our usual health advice of “don’t drink your calories”, because in this case, for once…
(and again, we must emphasize: only while actively doing strenuous exercise that is making specifically your muscles burn, not your joints or anything else; if your joints are burning you need to rest and definitely don’t spike your blood sugars because that will worsen inflammation)
…just this once, we do want those sugars to be zipping straight into the blood. Which means: liquid is best for this purpose.
And when we say liquid: gel is the same as a drink, so far as the body is concerned, provided the body in question is adequately hydrated (i.e., you are also drinking water).
Here are a pair of studies (by the same team, with the same general methodology), testing things head-to-head, with endurance cyclists on 6-hour stationary cycle rides:
CHO Oxidation from a CHO Gel Compared with a Drink during Exercise
Meanwhile, liquid beat solid, but only significantly so from the 90-minute mark onwards, and even that significant difference was modest (i.e. it’s clinically significant, it’s a statistically reliable result and improbable as random happenstance, but the actual size of the difference was not huge):
Oxidation of Solid versus Liquid CHO Sources during Exercise
We would hypothesize that the reason that liquids only barely outperformed solids for this task is precisely because the solids in question were also designed for the task. When a company makes a fast-release energy bar, they don’t load it with fiber to slow it down. Which differentiates this greatly from, say, getting one’s sugars from whole fruit.
If the study had compared apples to apple juice, we hypothesize the results would have been very different. But alas, if that study has been done, we couldn’t find it.
Today has been all about what’s best during exercise, so let’s quickly finish with a note on what’s best before and after:
Before: What To Eat, Take, And Do Before A Workout
After: Overdone It? How To Speed Up Recovery After Exercise
Take care!
Share This Post
-
Happy Mind, Happy Life – by Dr. Rangan Chatterjee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s start with a “why”. If happiness doesn’t strike you as a worthwhile goal in and of itself, Dr. Chatterjee discusses the health implications of happiness/unhappiness.
And, yes, including in studies where other factors were controlled for, so he shows how happiness/unhappiness does really have a causal role in health—it’s not just a matter of “breaking news: sick people are less happy”.
The author, a British GP (General Practitioner, the equivalent of what the US calls a “family doctor”) with decades of experience, has found a lot of value in the practice of holistic medicine. For this reason, it’s what he recommends to his patients at work, in his books, his blog, and his regular spot on a popular BBC breakfast show.
The writing style is relaxed and personable, without skimping on information density. Indeed, Dr. Chatterjee offers many pieces of holistic health advice, and dozens of practical exercises to boost your happiness and proof you against adversity.
Because, whatever motivational speakers may say, we can’t purely “think ourselves happy”; sometimes we have real external threats and bad things in life. But, we can still improve our experience of even these things, not to mention suffer less, and get through it in better shape with a smile at the end of it.
Bottom line: if you’d like to be happier and healthier (who wouldn’t?), then this book is a sure-fire way to set you on that path.
Click here to check out Happy Mind, Happy Life and upgrade yours!
Share This Post
Related Posts
-
This Chair Rocks: A Manifesto Against Ageism – by Ashton Applewhite
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s easy to think of ageism as being 80% “nobody will hire me because I am three years away from standard retirement age”, but it’s a lot more pervasive than that. And some of it, perhaps the most insidious, is the ageism that we can sometimes internalize without thinking it through.
10almonds readers love to avoid/reverse aging (and this reviewer is no different!), but it’s good once in a while to consider our priorities and motivations, for example:
- There is merit in being able to live without disability or discomfort
- There is harm in feeling a need to pass for younger than we are
And yet, even things such as disabilities are, Applewhite fairly argues, not to be feared. Absolutely avoided if reasonably possible of course, yes, but if they happen they happen and it’s good that we be able to make our peace with that, because most people have at least some kind of disability before the end, and can still strive to make the most of the precious gift that is life. The goal can and should be to play the hand we’re dealt and to live as well as we can—whatever that latter means for us personally.
Many people’s life satisfaction goes up in later years, and Applewhite hypothesizes that while some of that can be put down to circumstances (often no longer overwhelmed with work etc, often more financially stable), a lot is a matter of having come to terms with “losing” youth and no longer having that fear. Thus, a new, freer age of life begins.
The book does cover many other areas too, more than we can list here (but for example: ranging from pro/con brain differences to sex and intimacy), and the idea that long life is a team sport, and that we should not fall into the all-American trap of putting independence on a pedestal. Reports of how aging works with close-knit communities in the supercentenarian Blue Zones can be considered to quash this quite nicely, for instance.
The style is casual and entertaining, and yet peppered with scholarly citations, which stack up to 30 pages of references at the back.
Bottom line: getting older is a privilege that not everyone gets to have, so who are we to squander it? This book shares a vital sense of perspective, and is a call-to-arms for us all to do better, together.
Click here to check out This Chair Rocks, and indeed rock it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Spiced Fruit & Nut Chutney
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
‘Tis the season to make the chutney that will then be aged chutney when you want it later! And unlike supermarket varieties with their ingredients list that goes “Sugar, spirit vinegar, inverted glucose-fructose syrup,” this one has an array of health-giving fruits and nuts (just omit the nuts if you or someone you may want to give this to has an allergy), and really nothing bad in here at all. And of course, tasty healthful spices!
You will need
- 2 red onions, chopped
- 1½ cups dried apricots, chopped
- 1½ cups dried figs, chopped
- 1 cup raisins
- ½ cup apple cider vinegar
- ½ cup slivered almonds
- ½ lime, chopped and deseeded
- ¼ bulb garlic, chopped
- 1 hot pepper, chopped (your choice what kind; omit if you don’t like heat at all; multiply if you want more heat)
- 2 tablespoons honey or maple syrup (omit for a less sweet chutney; there is sweetness in the dried fruits already, after all)
- 1 tbsp freshly grated ginger
- 2 tsp sweet cinnamon
- 1 tsp nutmeg
- 1 tsp black pepper
- ½ teaspoon allspice
- ½ MSG or 1 tsp low-sodium salt
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a heavy-based pan that will be large enough for all ingredients to go into eventually. Fry the onions on a gentle heat for around 15 minutes. We don’t need to caramelize them yet (this will happen with time), but we do want them soft and sweet already.
2) Add the ginger, garlic, and chili, and stir in well.
3) When the onions start to brown, add the fruit and stir well to mix thoroughly.
4) Add the honey or maple syrup (if using), and the vinegar; add the remaining spices/seasonings, so everything is in there now except the almonds.
5) Cook gently for another 30 minutes while stirring. At some point it’ll become thick and sticky; add a little water as necessary. You don’t want to drown it, but you do want it to stay moist. It’ll probably take only a few tablespoons of added water in total, but add them one at a time and stir in before judging whether more is needed. By the end of the 30 minutes, it should be more solid, to the point it can stand up by itself.
6) Add the almonds, stir to combine, and leave to cool. Put it in jars until you need it (or perhaps give it as gifts).
Alternative method: if you don’t want to be standing at a stove stirring for about an hour in total, you can use a slow cooker / crock pot instead. Put the same ingredients in the same order, but don’t stir them, just leave them in layers (this is because of the pattern of heat distribution; it’ll be hotter at the bottom, so the things that need to be more cooked should be there, and the design means they won’t burn) for about two hours, then stir well to mix thoroughly, and leave it for another hour or two, before turning it off to let it cool. Put it in jars until you need it (or perhaps give it as gifts).
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Top 8 Fruits That Prevent & Kill Cancer ← figs and apricots appear here
- Apricots vs Peaches – Which is Healthier? ← have a guess
- Almonds vs Walnuts – Which is Healthier? ← almonds won, but walnuts were close and would also work in this recipe
- Pistachios vs Almonds – Which is Healthier? ← almonds won, but pistachios were close and would also work in this recipe
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we scored 4/5 today!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
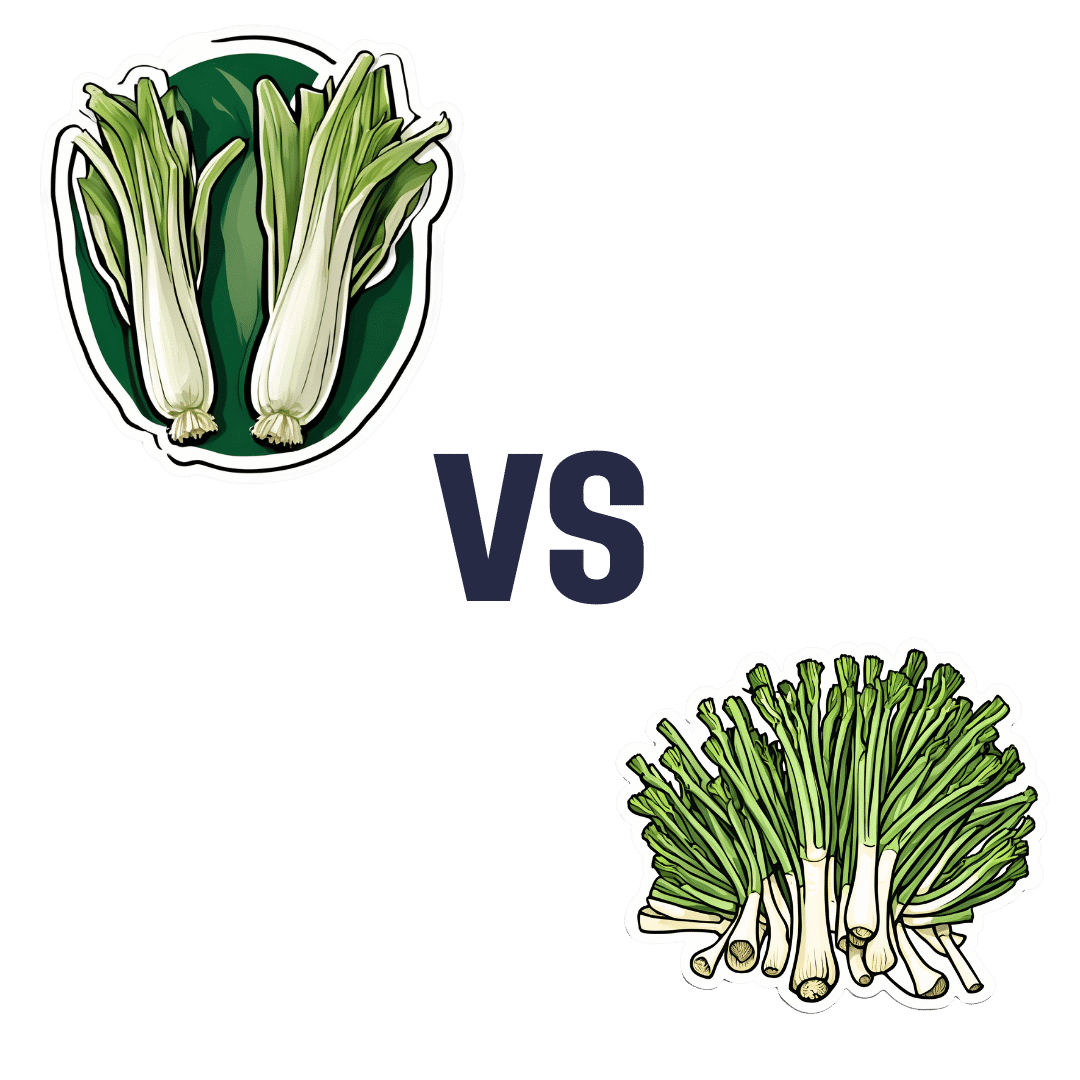
Leek vs Scallions – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing leek to scallions, we picked the leek.
Why?
In terms of macros, scallions might have a point: scallions have the lower glycemic index, thanks to leek having more carbs for the same amount of fiber. That said, leek already has a low glycemic index, so this is not a big deal.
When it comes to vitamins, leek has more of vitamins B1, B2, B3, B5, B6, B9, E, and choline, while scallions have more of vitamins A, C, and K. Noteworthily, a cup of chopped leek already provides the daily dose of vitamins A and K, and the difference in levels of vitamin C is minimal. All in all, an easy 8:3 win for leeks here, even without taking that into account.
In the category of minerals, leek has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and selenium, while scallions have a little more zinc.
Both of these allium-family plants (i.e., related to garlic) have an abundance of polyphenols, especially kaempferol.
Of course, enjoy whatever goes best with your meal, but if you’re looking for nutritional density, then leek is where it’s at.
Want to learn more?
You might like to read:
The Many Health Benefits Of Garlic
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: