Maximize Your Misery! (7 Great Methods)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s imagine that instead of being healthily fulfilled in life, you wanted to spend your days as miserable as possible. What should you do?
Here are a few pointers:
Stay still
Avoid physical activity and/or outdoor exposure, to avoid any mood-lifting neurochemicals. In fact, remain indoors as much as possible, preferably in the same room.
If you want to absolutely maximize your misery, make your bedroom the sole space for all activities that it’s possible to do there.
Disrupt your sleep
Keep an irregular sleep schedule by varying your bedtime and wake-up times frequently. Sleep in as much as possible, and make up for it by staying up late to ensure ongoing exhaustion.
Maximize screentime
Use digital entertainment as much as possible to distract you from meaningful activities and rest—as a bonus, this will also help you to avoid self-reflection.
Begin and end your day with a device in hand.
Fuel negative emotions
If you’re going to focus on something, focus on problems you cannot control, to stoke the fires of anger and angst.
A good way of doing this is by staying informed about distressing events, while avoiding meaningful actions to address them. Contribute only in token gestures, and then lament the lack of change.
Follow your impulses
Act on short-term desires without considering long-term consequences, while avoiding behaviors that you know might improve your mood or wellbeing.
Trust that doing the same things that have not previously resulted in happiness, will continue to reliably deliver unhappiness.
Set goals to miss
It’s important that your goals should be vague, and overly ambitious in their scope and/or deliverability. Ideally you should also disregard any preparatory work that a person would normally do before embarking on such a project.
Bonus tip: you can further sabotage any chances of progress, by waiting for motivation to strike before you take any action.
Pursue happiness
Focus on chasing happiness itself, instead of improving your situation or skills. Treat happiness as an end goal, instead of a by-product of worthwhile activities.
Want to learn more?
If you’d like to know many more ways to be miserable, we featured these 7 from this book of 40, which we haven’t reviewed yet, but probably will one of these days:
How to Be Miserable: 40 Strategies You Already Use – by Dr. Randy Paterson
Alternatively…
If for some strange reason you’d rather not do those things, you might consider a previous article of ours:
How To Get Your Brain On A More Positive Track (Without Toxic Positivity)
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A Deeper Dive Into Seaweed
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We wrote briefly about nori yesterday, when we compared it with well-known superfood spirulina. In nutritional terms, it blew spirulina out of the water:
Spirulina vs Nori – Which Is Healthier?
We also previously touched on it here:
21% Stronger Bones in a Year at 62? Yes, It’s Possible (No Calcium Supplements Needed!) ← nori was an important part of the diet enjoyed here
What is nori?
Nori is a seaweed, but that can mean lots of different things. In nori’s case, it’s an aggregate of several kinds of red algae that clump together in the sea.
When dried and/or toasted (which processes improve* the nutritional value rather than diminishing it, by the way), it looks dark green or dark purple to black in color.
*Effects of pan- and air fryer-roasting on volatile and umami compounds and antioxidant activity of dried laver (Porphyra dentata) ← this is nori, by another name
If you enjoy sushi, nori is the dark flat sheety stuff that other things are often wrapped in.
The plant that has animal nutrients
As established in the head-to-head we linked above, nori is a nutritional powerhouse. But not only is it very full of the perhaps-expected vitamins and minerals, it also contains:
Omega-3 fatty acids, including EPA, which plants do not normally have (plants usually have just ALA, which the body can convert into other forms including EPA). While ALA is versatile, having EPA in food saves the body the job of converting it, and thus makes it more readily bioavailable. For more on the benefits of this, see:
What Omega-3 Fatty Acids Really Do For Us
Iodine, which land plants don’t generally have, but seaweed usually does. However, nori contains less iodine than other kinds of seaweed, which is (counterintuitively) good, since other kinds of seaweed often contain megadoses that go too far the other way and can cause different health problems.
- Recommended daily amount of iodine: 150µg ← note that’s micrograms, not milligrams
- One 10g serving of dried nori contains: 232µg ← this is good
- Tolerable daily upper limit of iodine: 1,100µg (i.e: 1.1mg)
- One 10g serving of dried kombu (kelp) contains: 13,270µg (i.e: 13.3mg) ← this is far too much; not good!
So: a portion of nori puts us into the healthiest spot of the range, whereas a portion of another example seaweed would put us nearly 13x over the tolerable upper limit.
For why this matters, see:
- 8 Signs Of Iodine Deficiency You Might Not Expect
- Foods For Managing Hypothyroidism (incl. Hashimoto’s)
- Eat To Beat Hyperthyroidism!
As you might note from the mentions of both hypo- and hyperthyroidism, (which are exacerbated by too little and too much iodine, respectively) hitting the iodine sweet spot is important, and nori is a great way to do that.
Vitamin B12, again not usually found in plants (most vegans supplement, often with nutritional yeast, which is technically neither an animal nor a plant). However, nori scores even higher:
Vitamin B12-Containing Plant Food Sources for Vegetarians
Beyond nutrients
Nori is also one of the few foods that actually live up the principle of a “detox diet”, as it can help remove toxins such as dioxins:
Detox diets for toxin elimination and weight management: a critical review of the evidence
It’s also been…
❝revealed to have anti-aging, anti-cancer, anti-coagulant, anti-inflammatory, anti-microbial, anti-oxidant, anti-diabetic, anti-Alzheimer and anti-tuberculose activities.❞
~ Dr. Şükran Çakir Arica et al.
Read: A study on the rich compounds and potential benefits of algae: A review
(for this to make sense you will need to remember that nori is, as we mentioned, an aggregate of diverse red algae species; in that paper, you can scroll down to Table 1, and see which species has which qualities. Anything whose name starts with “Porphyra” or “Porphridum” is found in nori)
Is it safe?
Usually! There are two potential safety issues:
- Seaweed can, while it’s busy absorbing valuable minerals from the sea, also absorb heavy metals if there are such pollutants in the region. For this reason, it is good to buy a product with trusted certifications, such that it will have been tested for such along the way.
- Seaweed can, while it’s busy absorbing things plants don’t usually have from the sea, also absorb allergens from almost-equally-small crustaceans. So if you have a seafood allergy, seaweed could potentially trigger that.
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Share This Post
-
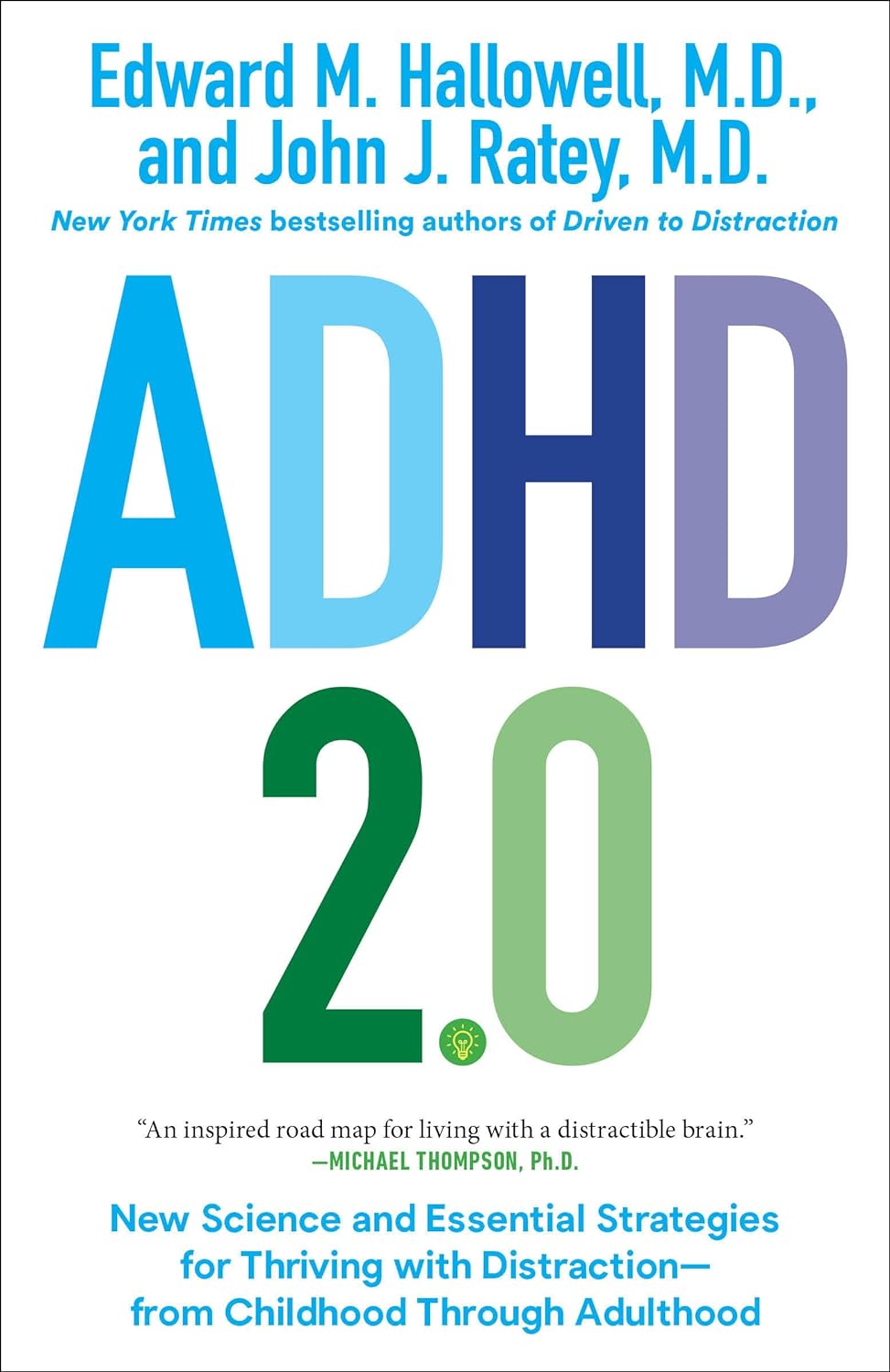
ADHD 2.0 – by Dr. Edward Hallowell & Dr. John Ratey
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of ADHD literature is based on the assumption that the reader is a 30-something parent of a child with ADHD. This book, on the other hand, addresses all ages, and includes just as readily the likelihood that the person with ADHD is the reader, and/or the reader’s partner.
The authors cover such topics as:
- ADHD mythbusting, before moving on to…
- The problems of ADHD, and the benefits that those exact same traits can bring too
- How to leverage those traits to get fewer of the problems and more of the benefits
- The role of diet beyond the obvious, including supplementation
- The role of specific exercises (especially HIIT, and balance exercises) in benefiting the ADHD brain
- The role of medications—and arguments for and gainst such
The writing style is… Thematic, let’s say. The authors have ADHD and it shows. So, expect comprehensive deep-dives from whenever their hyperfocus mode kicked in, and expect no stones left unturned. That said, it is very readable, and well-indexed too, for ease of finding specific sub-topics.
Bottom line: if you are already very familiar with ADHD, you may not learn much, and might reasonably skip this one. However, if you’re new to the topic, this book is a great—and practical—primer.
Share This Post
-
How Much Difference Do Probiotic Supplements Make, Really?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Much Difference Do Probiotic Supplements Make?
There are three main things that get talked about with regard to gut health:
- Prebiotics (fibrous foods)
- Probiotics (things containing live “good” bacteria)
- Postbiotics (things to help them thrive)
Today we’ll be talking about probiotics, but if you’d like a refresher on general gut health, here’s our previous main feature:
Making Friends With Your Gut (You Can Thank Us Later)
What bacteria are in probiotics?
There are many kinds, but the most common by far are Lactobacillus sp. and Bifidobacteria sp.
Taxonomical note: “sp.” just stands for “species”. The first name is the genus, which contains a plurality of (sometimes, many) species.
Lactobacillus acidophilus, also written L. acidophilus, is a common species of Lactobacillus sp. in probiotics.
Bifidobacterium bifidum, also written B. bifidum, is a common species of Bifidobacterium sp. in probiotics.
What difference do they make?
First, and perhaps counterintuitively, putting more bacteria into your gut has a settling effect on the digestion. In particular, probiotics have been found effective against symptoms of IBS and ulcerative colitis, (but not Crohn’s):
- Probiotics in Irritable Bowel Syndrome: An Up-to-Date Systematic Review
- The role of probiotics in the prevention and treatment of IBS and other related diseases: a systematic review of randomized human clinical trials
- Safety and Potential Role of Lactobacillus rhamnosus GG Administration as Monotherapy in Ulcerative Colitis Patients
- Probiotics for induction of remission in Crohn’s disease
Probiotics are also helpful against diarrhea, including that caused by infections and/or antibiotics, as well as to reduce antibiotic resistance:
- Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children
- Probiotic approach to prevent antibiotic resistance
Probiotics also boost the immune system outside of the gut, too, for example reducing the duration of respiratory infections:
You may recallthe link between gut health and brain health, thanks in large part to the vagus nerve connecting the two:
The Brain-Gut Highway: A Two-Way Street
No surprises, then, that probiotics benefit mental health. See:
- The effects of probiotics on mental health and hypothalamic-pituitary-adrenal axis: A randomized, double-blind, placebo-controlled trial
- A randomized controlled trial to test the effect of multispecies probiotics on cognitive reactivity to sad mood
- Clinical and metabolic response to probiotic administration in patients with major depressive disorder: A randomized, double-blind, placebo-controlled trial
There are so many kinds; which should I get?
Diversity is good, so more kinds is better. However, if you have specific benefits you’d like to enjoy, you may want to go stronger on particular strains:
Choosing an appropriate probiotic product for your patient: An evidence-based practical guide
Where can I get them?
We don’t sell them, but here’s an example product on Amazon, for your convenience.
Alternatively, you can check out today’s sponsor, who also sell such; we recommend comparing products and deciding which will be best for you
Enjoy!
Share This Post
Related Posts
-
Codependent No More – by Melody Beattie
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a book review, not a book summary, but first let’s quickly cover a common misconception, because the word “codependent” gets misused a lot in popular parlance:
- What codependence isn’t: “we depend on each other and must do everything together”
- What codependence is:“person 1 has a dependency on a substance (or perhaps a behavior, such as gambling); person 2 is trying to look after person 1, and so has developed a secondary relationship with the substance/behavior. Person 2 is now said to be codependent, because it becomes all-consuming for them too, even if they’re not using the substance/behavior directly”
Funny how often it happens that the reality is more complex than the perception, isn’t it?
Melody Beattie unravels all this for us. We get a compassionate and insightful look at how we can look after ourselves, while looking after another. Perhaps most importantly: how and where to draw a line of what we can and cannot do/change for them.
Because when we love someone, of course we want to fight their battles with them, if not for them. But if we want to be their rock of strength, we can’t get lost in it too, and of course that hurts.
Beatty takes us through these ideas and more, for example:
- How to examine our own feelings even when it’s scary
- How to practice self-love and regain self-worth, while still caring for them
- How to stop being reactionary, step back, and act with purpose
If the book has any weak point, it’s that it repeatedly recommends 12-step programs, when in reality that’s just one option. But for those who wish to take another approach, this book does not require involvement in a 12-step program, so it’s not a barrier to usefulness.
Click here to check out Codependent No More and take care of yourself, too
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Codependency Isn’t What Most People Think It Is
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Codependency isn’t what most people think it is
In popular parlance, people are often described as “codependent” when they rely on each other to function normally. That’s interdependent mutualism, and while it too can become a problem if a person is deprived of their “other half” and has no idea how to do laundry and does not remember to take their meds, it’s not codependency.
Codependency finds its origins in the treatment and management of alcoholism, and has been expanded to encompass other forms of relationships with dependence on substances and/or self-destructive behaviors—which can be many things, including the non-physical, for example a pattern of irresponsible impulse-spending, or sabotaging one’s own relationship(s).
We’ll use the simplest example, though:
- Person A is (for example) an alcoholic. They have a dependency.
- Person B, married to A, is not an alcoholic. However, their spouse’s dependency affects them greatly, and they do what they can to manage that, and experience tension between wanting to “save” their spouse, and wanting their spouse to be ok, which latter, superficially, often means them having their alcohol.
Person B is thus said to be “codependent”.
The problem with codependency
The problems of codependency are mainly twofold:
- The dependent partner’s dependency is enabled and thus perpetuated by the codependent partner—they might actually have to address their dependency, if it weren’t for their partner keeping them from too great a harm (be it financially, socially, psychologically, medically, whatever)
- The codependent partner is not having a good time of it either. They have the stress of two lives with the resources (e.g. time) of one. They are stressing about something they cannot control, understandably worrying about their loved one, and, worse: every action they might take to “save” their loved one by reducing the substance use, is an action that makes their partner unhappy, and causes conflict too.
Note: codependency is often a thing in romantic relationships, but it can appear in other relationships too, e.g. parent-child, or even between friends.
See also: Development and validation of a revised measure of codependency
How to deal with this
If you find yourself in a codependent position, or are advising someone who is, there are some key things that can help:
- Be a nurturer, not a rescuer. It is natural to want to “rescue” someone we care about, but there are some things we cannot do for them. Instead, we must look for ways to build their strength so that they can take the steps that only they can take to fix the problem.
- Establish boundaries. Practise saying “no”, and also be clear over what things you can and cannot control—and let go of the latter. Communicate this, though. An “I’m not the boss of you” angle can prompt a lot of people to take more personal responsibility.
- Schedule time for yourself. You might take some ideas from our previous tangentially-related article:
How To Avoid Carer Burnout (Without Dropping Care)
Want to read more?
That’s all we have space for today, but here’s a very useful page with a lot of great resources (including questionnaires and checklist and things, in case you’re thinking “is it, or…?”)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
When You “Should” Be In Better Shape
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s easy to think that we “should” be many things that we aren’t. However, it can be counterproductive to implementing real change:
The problem with “should”
The word “should” often sabotages changes in mindset and habit formation. Saying things like “I should be further along” typically leads to frustration, feelings of failure, and ultimately a lack of motivation to take action. Yes, in the first instance, “I should…” can be a motivator, but when your goals are not achieved by the second session, and the “I should…” is still there, the subconscious says “well, clearly this is not working”. Even though the conscious mind can easily see the fallacy in that dysfunctional line of thinking, the subconscious is easily swayed by such things, and in turn easily sways our actual behaviors.
Also, even before that, if goals feel impossible, people often do nothing instead of making small, manageable changes.
So, what should we do instead?
Step 1: assess your current lifestyle and priorities. Your current results are a reflection of past habits and actions, including dieting practices, inconsistent workouts, and lack of planning. Instead of searching for a “perfect plan,” first acknowledge your current lifestyle and priorities. Then, identify which habits are beneficial, which ones hold you back, and what common excuses you make. By understanding where you are now, you can create a sustainable plan that fits your life rather than fighting against it.
Step 2: define your future lifestyle. It’s not enough to just set goals—you need to define what the lifestyle associated with those goals looks like. Recognize that real change requires adjustments in habits and routines. Don’t stress over whether these changes feel overwhelming; simply identify what might be necessary. Writing things down (and then consulting them often, not just putting them away never to be seen again) makes them more tangible and helps create a roadmap for progress.
Step 3: make one small change today. Rather than making vague or overwhelming changes, start with one small, realistic step that aligns with your goals. Building momentum through cumulatively beneficial small actions leads to longer-lasting motivation. Also, instead of focusing on what you need to cut out, look for positive habits to add, as this makes change easier. Track your progress visibly—like using a checklist—and commit to revisiting and adding new changes weekly.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
How To Plan For The Unplannable And Always Follow Through
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: