The Science Of Sounds
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We Think You Might Like The Sound Of This…
We’ve written before about the benefits of mindfulness meditation, and how to do it.
We also reviewed a great book on a related topic:
This is Your Brain On Music – by Dr. Daniel Levitin
(yes, that’s the same neuroscientist that we featured as an expert talking about The Five Keys of Aging Healthily)
But what happens when we combine the two?
Mantra meditation & music
Most scientific studies that have been undertaken with regard to meditation tend to focus on mindfulness meditation. It’s easy, effective, and (which makes a difference when it comes to publication bias) is a very safe bet when it comes to funding.
However, today we’re going to look at mantra meditation, which has a lot in common, neurologically speaking, with music. Indeed, when the two were compared separately in a randomized control trial:
❝Daily mantra meditation or classical music listening may be beneficial for cognitive outcomes and quality of life of breast cancer survivors with cancer-related cognitive impairment.
The cognitive benefits appear to be sustained beyond the initial intervention period.❞
One possible reason for some of the similar benefits is the vagus nerve—whether intoning a mantra, or humming along to music, the vibrations can stimulate the vagus nerve, which in turn activates the parasympathetic nervous system, resulting in body-wide relaxation:
The Vagus Nerve (And How You Can Make Use Of It)
How effective is mantra meditation?
According to a large recent narrative review, it depends on your goal:
❝Based on the studies in the four important areas presented, there is no doubt of a strong connection between mantra meditation and human health.
Strong evidence has been found that practicing mantra meditation is effective in relieving stress and in coping with hypertension.
For the other two areas: anxiety and immunity, the evidence is inconclusive or not strong enough to firmly support the claim that the mantra meditation can be used to reduce anxiety or to improve immunity. ❞
Read in full: Scientific Evidence of Health Benefits by Practicing Mantra Meditation: Narrative Review
this is a very interesting read if you do have the time!
How do I practice mantra meditation?
The definition is broad, but the critical criteria are:
- You meditate…
- …using a mantra
Lest that seem flippant: those really are the two key points!
Meditation comes in various forms, and mantra meditation is a form of focussed meditation. While some focussed meditation forms may use a candle or some other focal point, in mantra meditation, the mantra itself provides the focus.
You may be wondering: what should the mantra be?
Classic and well-tested mantras include such simple things as the monosyllabic Sanskrit “Om” or “Ham”. We’re a health science newsletter, so we’ll leave esoteric meanings to other publications as they are beyond our scope, but we will say that these result, most naturally, in the humming sound that we mentioned earlier stimulates the vagus nerve.
But that’s not the only way. Practitioners of religions that have repetitive prayer systems (e.g. anything that uses prayer beads, for example) also provide the basis of focused meditation, using a mantra (in this case, usually a very short oft-repeated prayer phrase).
How long is needed for benefits?
Most studies into mantra meditation have used timed sessions of 15–30 minutes, with 20 minutes being a commonly-used session length, once per day. However…
- Vagus nerve benefits should appear a lot more quickly than that (under 5 minutes) in the case of mantras that cause that vibration we mentioned.
- Repetitive spoken prayers (or similar repeated short phrases, for the irreligious) will generally effect relaxation in whatever period of time it takes for your brain to be fully focused on what you are doing now, instead of what you were thinking about before. If using counting beads, then you probably already know what number works for you.
(again, as a health science publication, we cannot comment on any otherworldly benefits, but the worldly benefits seem reason enough to consider these practices for their potential therapeutic effects)
10almonds tip: for any meditative practice that you want to take approximately a given period of time, we recommend investing in a nice sand timer like this one, as this will not result in a jarring alarm going off!
Like to jazz things up a little?
Enjoy: Meditation That You’ll Actually Enjoy ← Meditation games!
Prefer to keep things to the basics?
Enjoy: No Frills, Evidence-Based Mindfulness ← The simplest scientific approach
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Are “Adaptogens” Anyway? (And Other Questions Answered)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I tried to use your calculator for heart health, and was unable to enter in my height or weight. Is there another way to calculate? Why will that field not populate?❞
(this is in reference to yesterday’s main feature “How Are You, Really? And How Old Is Your Heart?“)
How strange! We tested it in several desktop browsers and several mobile browsers, and were unable to find any version that didn’t work. That includes switching between metric and imperial units, per preference; both appear to work fine. Do be aware that it’ll only take numerical imput, though.
Did anyone else have this problem? Let us know! (You can reply to this email, or use the handy feedback widget at the bototm)
❝I may have missed it, but how much black pepper provides benefits?❞
So, for any new subscribers joining us today, this is about two recent main features:
As for a daily dosage of black pepper, it varies depending on the benefit you’re looking for, but:
- 5–20mg of piperine is the dosage range used in most scientific studies we looked at
- 10mg is a very common dosage found in many popular supplements
- That’s the mass of piperine though, so if taking it as actual black pepper rather than as an extract, ½ teaspoon is considered sufficient to enjoy benefits.
❝I loved the health benefits of pepper. I do not like pepper. Where can I get it as a supplement?❞
You can simply buy whole black peppercorns and take a few with water as though they were tablets. Your stomach acid will do the rest. Black pepper is also good for digestion, so taking it with a meal is best.
You can buy piperine (black pepper extract) by itself as a supplement in powder form, but if you don’t like black pepper, you will probably not like this powder either. We couldn’t find it readily in capsule form.
You can buy piperine (black pepper extract) as an adjunct to other supplements, with perhaps the most common/popular being turmeric capsules that also contain 10mg (or more) piperine per capsule. Shop around if you like, but here’s one that has 15mg piperine* per capsule, for example.
*They call it “Bioperine®” but that is literally just piperine. Same goes if you see “Absorbagen™”, it’s still just piperine.
❝What do you mean when you say that something is adaptogenic?❞
Simple version: it means it helps the body adapt to stress, by adjusting the body’s natural responses. Thus, adaptogenic supplements can be contrasted with tranquilizing drugs that mask stress by brute force, for example.
Technical version: adaptogenic activity refers to improving physiological stress resilience, such as by moderating and modulating hypothalamic–pituitary–adrenal axis signaling, and/or by regulating levels of endogenic compounds involved in the cellular stress response.
Read more (technical version):
Read more (simple version):
European Medicines Agency’s Reflection Paper On The Adaptogenic Concept
Enjoy!
Share This Post
-
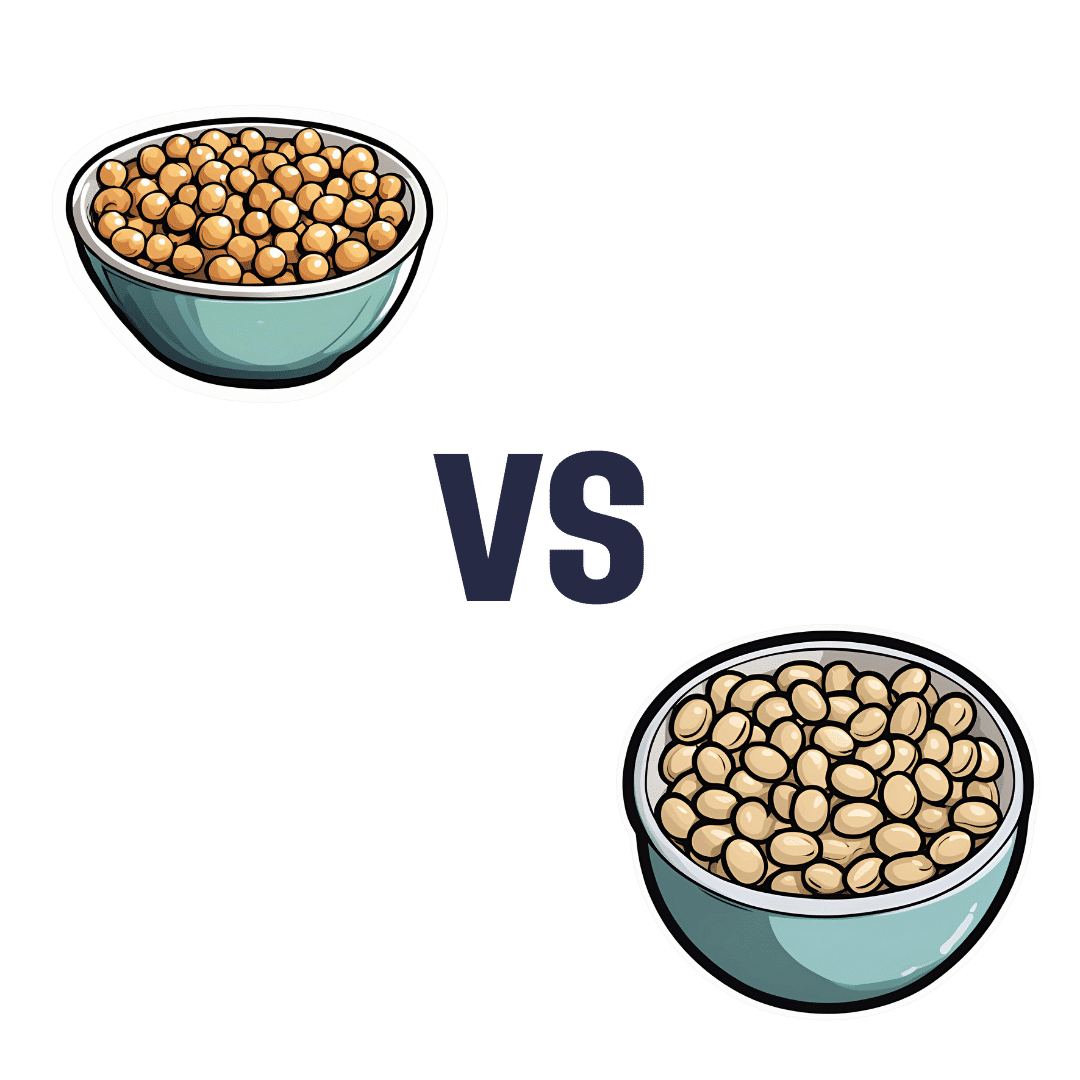
Chickpeas vs Soybeans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing chickpeas to soybeans, we picked the soybeans.
Why?
Both are great! But:
In terms of macros, chickpeas have more than 3x the carbs and only very slightly more fiber, while soybeans have more than 2x the protein. Given the ratio of carbs to fiber in each, soybeans also have the lower glycemic index, so all in all, we’re calling this a win for soybeans.
In the category of vitamins, chickpeas have more of vitamins A, B3, B5, and B9, while soybeans have more of vitamins B1, B2, B6, C, K, and choline—another win for soybeans.
When it comes to minerals, chickpeas have more manganese and zinc, while soybeans have more calcium, copper, iron, magnesium, phosphorus, potassium, and selenium—meaning soybeans win yet again.
Two extra things to know:
- Chickpeas are naturally high in FODMAPs, which can be problematic for a minority of people—however, canned chickpeas are not.
- Soybeans are famously high in phytoestrogens, however, the human body cannot actually use these as estrogen (we are not plants and our physiology is different). This means that on the one hand they won’t help against menopause (aside from the ways in which any nutrient-dense food would help), but on the other, they aren’t a cancer risk, and no, they won’t feminize men/boys in the slightest. You/they would be more at risk from beef and dairy, as the cows have usually been given extra estrogen, and those are animal hormones, not plant hormones.
All in all, chickpeas are a wonderful food, but soybeans beat them by most nutritional metrics.
Want to learn more?
You might like to read:
Why You Can’t Skimp On Amino Acids ← soybeans also have a great amino acid profile!
Enjoy!
Share This Post
-
Make Your Coffee Heart-Healthier!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Health-Hack Your Coffee
We have previously written about the general health considerations (benefits and potential problems) of coffee:
The Bitter Truth About Coffee (or is it?)
Today, we will broadly assume that you are drinking coffee (in general, not necessarily right now, though if you are, same!) and would like to continue to do so. We also assume you’d like to do so as healthily as possible.
Not all coffees are created equal
If you order a coffee in France or Italy without specifying what kind, the coffee you receive will be short, dark,
and handsomeand without sugar. Healthwise, this is not a bad starting point. However…- It will usually be espresso
- Or it may be what in N. America is called a French press (in Europe it’s just called a cafetière)
Both of these kinds of coffee mean that cafestol, a compound found in the oily part of coffee and which is known to raise LDL (“bad” cholesterol”), stays in the drink.
Read: Cafestol and Kahweol: A Review on Their Bioactivities and Pharmacological Properties
Also: Cafestol extraction yield from different coffee brew mechanisms
If you’re reading that second one and wondering what a mocha pot or a Turkish coffee is, they are these things:
- Mocha pot: a stovetop device used for making espresso without an espresso machine
- Turkish coffee pot: also a stovetop device; this thing makes some of the strongest coffee you have ever encountered. Turks usually add sugar (this writer doesn’t; but my taste in coffee been described as “coffee like a punch in the face”)
So, wonderful as they are for those of us who love strong coffee, they also produce the highest in-drink levels of cafestol. If you’d like to cut the cafestol (for example, if you are keeping an eye on your LDL), we recommend…
The humble filter coffee
Whether by your favorite filter coffee machine or a pour-over low-tech coffee setup of the kind you could use even without an electricity supply, the filter keeps more than just the coffee grinds out; it keeps the cafestol out too; most of it, anyway, depending on what kind of filter you use, and the grind of the coffee:
Physical characteristics of the paper filter and low cafestol content filter coffee brews
What about instant coffee?
It has very little cafestol in it. It’s up to you whether that’s sufficient reason to choose it over any other form of coffee (this coffee-lover could never)
Want to make any coffee healthier?
This one isn’t about the cafestol, but…
If you take l-theanine (see here for our previous main feature about l-theanine), the l-theanine acts as a moderator and modulator of the caffeine, amongst other benefits:
The Cognitive-Enhancing Outcomes of Caffeine and L-theanine: A Systematic Review
As to where to get that, we don’t sell it, but here’s an example product on Amazon
Enjoy!
Share This Post
Related Posts
-
How To Keep Your Mind From Wandering
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whether your mind keeps wandering more as you get older, or you’re a young student whose super-active brain is more suited to TikTok than your assigned reading, sustained singular focus can be a challenge for everyone—and yet (alas!) it remains a required skill for so much in life.
Today’s edition of 10Almonds presents a nifty trick to get yourself through those tasks! We’ll also be taking some time to reply to your questions and comments, in our weekly interactive Q&A.
First of all though, we’ve a promise to make good on, so…
How To Stay On The Ball (Or The Tomato?) The Easy Way
For most of us, we face three main problems when it comes to tackling our to-dos:
- Where to start?
- The task seems intimidating in its size
- We get distracted and/or run out of energy
If you’re really not sure where to start, we recommended a powerful tool in last Friday’s newsletter!
For the rest, we love the Pomodoro Technique:
- Set a timer for 25 minutes, and begin your task.
- Keep going until the timer is done! No other tasks, just focus.
- Take a 5-minute break.
- Repeat
This approach has three clear benefits:
- No matter the size of the task, you are only committing to 25 minutes—everything is much less overwhelming when there’s an end in sight!
- Being only 25 minutes means we are much more likely to stay on track; it’s easier to defer other activities if we know that there will be a 5-minute break for that soon.
- Even without other tasks to distract us, it can be difficult to sustain attention for long periods; making it only 25 minutes at a time allows us to approach it with a (relatively!) fresh mind.
Have you heard that a human brain can sustain attention for only about 40 minutes before focus starts to decline rapidly?
While that’s been a popular rationale for school classroom lesson durations (and perhaps coincidentally ties in with Zoom’s 40-minute limit for free meetings), the truth is that focus starts dropping immediately, to the point that one-minute attention tests are considered sufficient to measure the ability to focus.
So a 25-minute Pomodoro is a more than fair compromise!
Why’s it called the “Pomodoro” technique?
And why is the 25-minute timed work period called a Pomodoro?
It’s because back in the 80s, university student Francesco Cirillo was struggling to focus and made a deal with himself to focus just for a short burst at a time—and he used a (now “retro” style) kitchen timer in the shape of a tomato, or “pomodoro”, in Italian.
If you don’t have a penchant for kitsch kitchenware, you can use this free, simple Online Pomodoro Timer!
(no registration/login/download necessary; it’s all right there on the web page)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Passion Fruit vs Persimmon – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing passion fruit to persimmon, we picked the passion fruit.
Why?
You may be wondering: “what is this fruit passionate about?” and the answer is: delivering nutrients of many kinds!
Looking at the macros first, passion fruit has a little more protein and a lot more fiber, while persimmon has more carbs. This means that while persimmon’s glycemic index isn’t bad, passion fruit’s glycemic index is a lot lower.
In terms of vitamins, passion fruit has a lot more of vitamins A, B2, B3, B6, B9, E, K, and choline, while persimmon has more vitamin C. For the record passion fruit is also a good source of vitamin C, with a cup of passion fruit already giving a day’s daily dose of vitamin C, but persimmon gives twice that. Still, that’s a 8:1 win for passion fruit.
When it comes to minerals, passion fruit has more copper, magnesium, phosphorus, potassium, selenium, and zinc, while persimmon has more calcium and iron, meaning a 6:2 win for passion fruit.
Adding up the three convincing individual victories shows a clear overall win for passion fruit.
Enjoy (passionately, even)!
Want to learn more?
You might like to read:
- Glycemic Index vs Glycemic Load vs Insulin Index
- Which Sugars Are Healthier, And Which Are Just The Same?
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
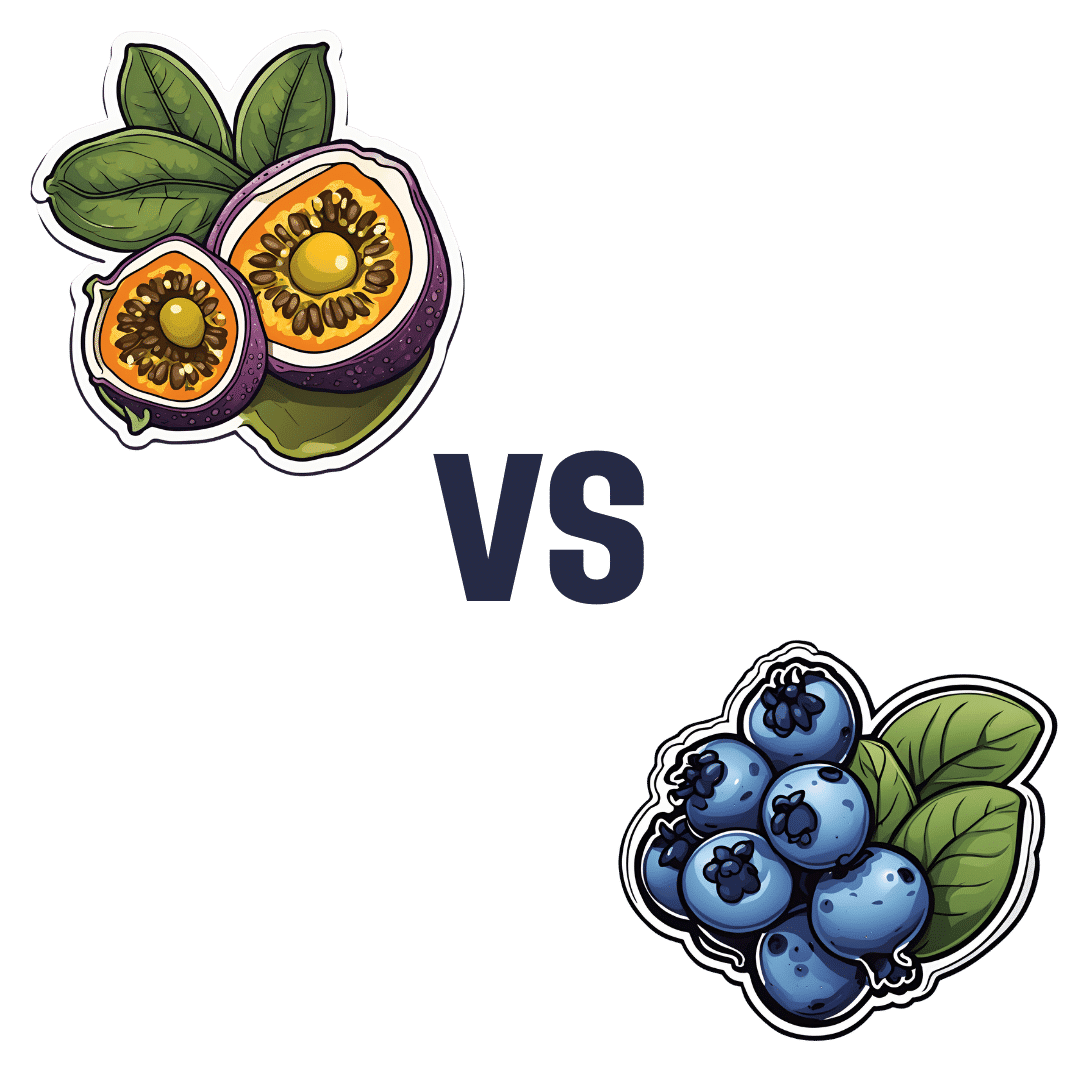
Passion Fruit vs Blueberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing passion fruit to blueberries, we picked the passion fruit.
Why?
It wasn’t close!
In terms of macros, the passion fruit has 3x the protein, 1.5x the carbs, and more than 4x the fiber. An easy win for passion fruit!
In the category of vitamins, passion fruit has more of vitamins A, B2, B3, B5, B6, B7, B9, C, and choline, while blueberries have more of vitamins B1, E, and K. So, blueberries are not without their merits, but all in all, another win for passion fruit here.
When it comes to minerals, passion fruit has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and selenium, while blueberries have slightly more zinc.
Looking at polyphenols, this is one category where blueberry wins, and by a fair margin. We think that’s a great reason to enjoy blueberries, but not enough to reverse the win for passion fruit based on all the other categories!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: