Tinnitus: Quieting The Unwanted Orchestra In Your Ears
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Tinnitus—When a “minor” symptom becomes disruptive
Tinnitus (typically: ringing in the ears) is often thought of less as a condition in and of itself, and more a symptom related to other hearing-related conditions. Paradoxically, it can be associated with hearing loss as well as with hyperacusis (hearing supersensitivity, which sounds like a superpower, but can be quite a problem too).
More than just ringing
Tinnitus can manifest not just as ringing, but also as whistling, hissing, pulsing, buzzing, hooting, and more.
For those who don’t suffer from this, it can seem very trivial; for those who do… Sometimes it can seem trivial too!
But sometimes it’s hard to carry on a conversation when at random moments it suddenly sounds like someone is playing a slide-whistle directly into your earhole, or like maybe a fly got stuck in there.
It’s distracting, to say the least.
What causes it?
First let’s note, tinnitus can be acute or chronic. So, some of these things may just cause tinnitus for a while, whereas some may give you tinnitus for life. In some cases, it depends on how long the thing in question persisted for.
A lot of things can cause it, but common causes include:
- Noise exposure (e.g. concerts, some kinds of industrial work, war)
- High blood pressure
- Head/neck injuries
- Ear infection
- Autoimmune diseases (e.g. Type 1 Diabetes, Lupus, Multiple Sclerosis)
So what can be done about it?
Different remedies will work (or not) for different people, depending on the cause and type of tinnitus.
Be warned also: some things that will work for one person’s tinnitus will make another person’s worse, so you might need to try a degree of experimentation and some of it might not be fun!
That in mind, here are some things you might want to try if you haven’t already:
- Earplugs or noise-canceling headphones—while tinnitus is an internal sound, not external, it often has to do with some part(s) of your ears being unduly sensitive, so giving them less stimulus may ease the tinnitus that occurs in reaction to external noise.
- A great option (that this writer uses personally and considers a life-changer) is silicon earplugs that live in a little case on a keyring when not in use—no more heart-racing fleeing from supermarket checkout boops or pedestrian crossing bips or traffic noises or babies crying or (etc)
- White noise—if you also have hyperacusis, a lower frequency range will probably not hurt the way a higher range might. If you don’t also have hyperacusis, you have more options here and this is a popular remedy. Either way, white noise outperforms “relaxing” soundscapes.
- Hearing aids—counterintuitively, for some people whose tinnitus has developed in response to hearing loss, hearing aids can help bring things “back to normal” and eliminate tinnitus in the process.
- Customized sound machines—if you have the resources to get fancy, science currently finds this to be best of all. They work like white noise, but are tailored to your specific tinnitus.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
I have a stuffy nose, how can I tell if it’s hay fever, COVID or something else?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hay fever (also called allergic rhinitis) affects 24% of Australians. Symptoms include sneezing, a runny nose (which may feel blocked or stuffy) and itchy eyes. People can also experience an itchy nose, throat or ears.
But COVID is still spreading, and other viruses can cause cold-like symptoms. So how do you know which one you’ve got?
Lysenko Andrii/Shutterstock Remind me, how does hay fever cause symptoms?
Hay fever happens when a person has become “sensitised” to an allergen trigger. This means a person’s body is always primed to react to this trigger.
Triggers can include allergens in the air (such as pollen from trees, grasses and flowers), mould spores, animals or house dust mites which mostly live in people’s mattresses and bedding, and feed on shed skin.
When the body is exposed to the trigger, it produces IgE (immunoglobulin E) antibodies. These cause the release of many of the body’s own chemicals, including histamine, which result in hay fever symptoms.
People who have asthma may find their asthma symptoms (cough, wheeze, tight chest or trouble breathing) worsen when exposed to airborne allergens. Spring and sometimes into summer can be the worst time for people with grass, tree or flower allergies.
However, animal and house dust mite symptoms usually happen year-round.
Ryegrass pollen is a common culprit. bangku ceria/Shutterstock What else might be causing my symptoms?
Hay fever does not cause a fever, sore throat, muscle aches and pains, weakness, loss of taste or smell, nor does it cause you to cough up mucus.
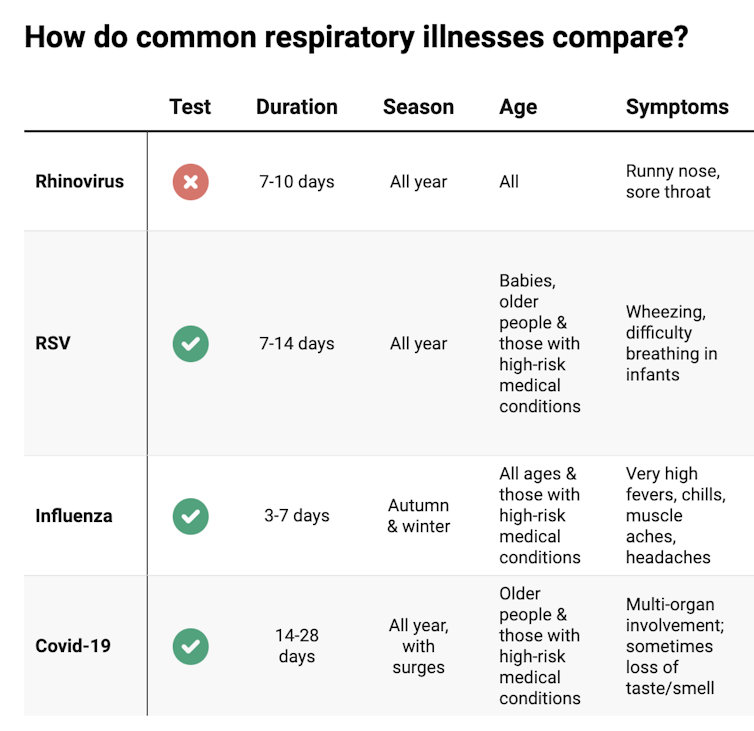
These symptoms are likely to be caused by a virus, such as COVID, influenza, respiratory syncytial virus (RSV) or a “cold” (often caused by rhinoviruses). These conditions can occur all year round, with some overlap of symptoms:
Natasha Yates/The Conversation COVID still surrounds us. RSV and influenza rates appear higher than before the COVID pandemic, but it may be due to more testing.
So if you have a fever, sore throat, muscle aches/pains, weakness, fatigue, or are coughing up mucus, stay home and avoid mixing with others to limit transmission.
People with COVID symptoms can take a rapid antigen test (RAT), ideally when symptoms start, then isolate until symptoms disappear. One negative RAT alone can’t rule out COVID if symptoms are still present, so test again 24–48 hours after your initial test if symptoms persist.
You can now test yourself for COVID, RSV and influenza in a combined RAT. But again, a negative test doesn’t rule out the virus. If your symptoms continue, test again 24–48 hours after the previous test.
If it’s hay fever, how do I treat it?
Treatment involves blocking the body’s histamine release, by taking antihistamine medication which helps reduce the symptoms.
Doctors, nurse practitioners and pharmacists can develop a hay fever care plan. This may include using a nasal spray containing a topical corticosteroid to help reduce the swelling inside the nose, which causes stuffiness or blockage.
Nasal sprays need to delivered using correct technique and used over several weeks to work properly. Often these sprays can also help lessen the itchy eyes of hay fever.
Drying bed linen and pyjamas inside during spring can lessen symptoms, as can putting a smear of Vaseline in the nostrils when going outside. Pollen sticks to the Vaseline, and gently blowing your nose later removes it.
People with asthma should also have an asthma plan, created by their doctor or nurse practitioner, explaining how to adjust their asthma reliever and preventer medications in hay fever seasons or on allergen exposure.
People with asthma also need to be alert for thunderstorms, where pollens can burst into tinier particles, be inhaled deeper in the lungs and cause a severe asthma attack, and even death.
What if it’s COVID, RSV or the flu?
Australians aged 70 and over and others with underlying health conditions who test positive for COVID are eligible for antivirals to reduce their chance of severe illness.
Most other people with COVID, RSV and influenza will recover at home with rest, fluids and paracetamol to relieve symptoms. However some groups are at greater risk of serious illness and may require additional treatment or hospitalisation.
For RSV, this includes premature infants, babies 12 months and younger, children under two who have other medical conditions, adults over 75, people with heart and lung conditions, or health conditions that lessens the immune system response.
For influenza, people at higher risk of severe illness are pregnant women, Aboriginal people, people under five or over 65 years, or people with long-term medical conditions, such as kidney, heart, lung or liver disease, diabetes and decreased immunity.
If you’re concerned about severe symptoms of COVID, RSV or influenza, consult your doctor or call 000 in an emergency.
If your symptoms are mild but persist, and you’re not sure what’s causing them, book an appointment with your doctor or nurse practitioner. Although hay fever season is here, we need to avoid spreading other serious infectious.
For more information, you can call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria); use the online Symptom Checker; or visit healthdirect.gov.au or the Australian Society of Clinical Immunology and Allergy.
Deryn Thompson, Eczema and Allergy Nurse; Lecturer, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Hungry? How To Beat Cravings
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Science of Hunger, And How To Sate It
This is Dr. David Ludwig. That’s not a typo; he’s a doctor both ways—MD and PhD.
Henceforth we’ll just say “Dr. Ludwig”, though! He’s a professor in the Department of Nutrition at Harvard T.H. Chan School of Public Health, and director of the New Balance Foundation Obesity Prevention Center.
His research focuses on the effects of diet on hormones, metabolism, and body weight, and he’s one of the foremost experts when it comes to carbohydrates, glycemic load, and obesity.
Why are we putting on weight? What are we getting wrong?
Contrary to popular belief, Dr. Ludwig says, weight gain is not caused by a lack of exercise. In fact, people tend to overestimate how many calories are burned by exercise.
A spoonful of sugar may make the medicine go down, but it also contains 60 calories, and that’d take about 1,500 steps for the average person to burn off. Let’s put this another way:
If you walk 10,000 steps per day, that will burn off 400 calories. Still think you can exercise away that ice cream sundae or plate of fries?
Wait, this is interesting and all, but what does this have to do with hunger?
Why we get hungry
Two important things:
- All that exercise makes us hungry, because the more we exercise, the more the body speeds up our metabolism accordingly.
- Empty calories don’t just add weight themselves, they also make us hungrier
What are empty calories, and why do they make us hungrier?
Empty calories are calories that are relatively devoid of other nutrition. This especially means simple sugars (especially refined sugar), white flour and white flour products (quick-release starches), and processed seed oils (e.g. canola, sunflower, and friends).
They zip straight into our bloodstream, and our body sends out an army of insulin to deal with the blood sugar spike. And… that backfires.
Imagine a person whose house is a terrible mess, and they have a date coming over in half an hour.
They’re going to zoom around tidying, but they’re going to stuff things out of sight as quickly and easily as possible, rather than, say, sit down and Marie Kondo the place.
But superficially, they got the job done really quickly!
Insulin does similarly when overwhelmed by a blood sugar spike like that.
So, it stores everything as fat as quickly as possible, and whew, the pancreas needs a break now after all that exertion, and the blood is nice and free from blood sugars.
Wait, the blood is what now?
The body notices the low blood sugar levels, and it also knows you just stored fat so you must be preparing for starvation, and now the low blood sugar levels indicate starvation is upon us. Quick, we must find food if we want to survive! So it sends a hunger signal to make sure you don’t let the body starve.
You make a quick snack, and the cycle repeats.
Dr. Ludwig’s solution:
First, we need to break out of that cycle, and that includes calming down our insulin response (and thus rebuilding our insulin sensitivity, as our bodies will have become desensitized, after the equivalent of an air-raid siren every 40 minutes or so).
How to do that?
First, cut out the really bad things that we mentioned above.
Next: cut healthy carbs too—we’re talking unprocessed grains here, legumes as well, and also starchy vegetables (root vegetables etc). Don’t worry, this will be just for a short while.
The trick here is that we are resensitizing our bodies to insulin.
Keep this up for even just a week, and then gradually reintroduce the healthier carbs. Unprocessed grains are better than root vegetables, as are legumes.
You’re not going to reintroduce the sugars, white flour, canola oil, etc. You don’t have to be a puritan, and if you go to a restaurant you won’t undo all your work if you have a small portion of fries. But it’s not going to be a part of your general diet.
Other tips from Dr. Ludwig:
- Get plenty of high-quality protein—it’s good for you and suppresses your appetite
- Shop for success—make sure you keep your kitchen stocked with healthy easy snack food
- Nuts, cacao nibs, and healthy seeds will be your best friends and allies here
- Make things easy—buy pre-chopped vegetables, for example, so when you’re hungry, you don’t have to wait longer (and work more) to eat something healthy
- Do what you can to reduce stress, and also eat mindfully (that means paying attention to each mouthful, rather than wolfing something down while multitasking)
If you’d like to know more about Dr. Ludwig and his work, you can check out his website for coaching, recipes, meal plans, his blog, and other resources!
Share This Post
-
You can’t reverse the ageing process but these 5 things can help you live longer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At this time of year many of us resolve to prioritise our health. So it is no surprise there’s a roaring trade of products purporting to guarantee you live longer, be healthier and look more youthful.
While an estimated 25% of longevity is determined by our genes, the rest is determined by what we do, day to day.
There are no quick fixes or short cuts to living longer and healthier lives, but the science is clear on the key principles. Here are five things you can do to extend your lifespan and improve your health.
1. Eat a predominantly plant-based diet
What you eat has a huge impact on your health. The evidence overwhelmingly shows eating a diet high in plant-based foods is associated with health and longevity.
If you eat more plant-based foods and less meat, processed foods, sugar and salt, you reduce your risk of a range of illnesses that shorten our lives, including heart disease and cancer.
Plant-based foods are rich in nutrients, phytochemicals, antioxidants and fibre. They’re also anti-inflammatory. All of this protects against damage to our cells as we age, which helps prevent disease.
No particular diet is right for everyone but one of the most studied and healthiest is the Mediterranean diet. It’s based on the eating patterns of people who live in countries around the Mediterranean Sea and emphases vegetables, fruits, wholegrains, legumes, nuts and seeds, fish and seafood, and olive oil.
2. Aim for a healthy weight
Another important way you can be healthier is to try and achieve a healthy weight, as obesity increases the risk of a number of health problems that shorten our lives.
Obesity puts strain on all of our body systems and has a whole myriad of physiological effects including causing inflammation and hormonal disturbances. These increase your chances of a number of diseases, including heart disease, stroke, high blood pressure, diabetes and a number of cancers.
In addition to affecting us physically, obesity is also associated with poorer psychological health. It’s linked to depression, low self-esteem and stress.
One of the biggest challenges we face in the developed world is that we live in an environment that promotes obesity. The ubiquitous marketing and the easy availability of high-calorie foods our bodies are hard-wired to crave mean it’s easy to consume too many calories.
3. Exercise regularly
We all know that exercise is good for us – the most common resolution we make this time of year is to do more exercise and to get fitter. Regular exercise protects against chronic illness, lowers your stress and improves your mental health.
While one of the ways exercising helps you is by supporting you to control your weight and lowering your body fat levels, the effects are broader and include improving your glucose (blood sugar) use, lowering your blood pressure, reducing inflammation and improving blood flow and heart function.
While it’s easy to get caught up in all of the hype about different exercise strategies, the evidence suggests that any way you can include physical activity in your day has health benefits. You don’t have to run marathons or go to the gym for hours every day. Build movement into your day in any way that you can and do things that you enjoy.
4. Don’t smoke
If you want to be healthier and live longer then don’t smoke or vape.
Smoking cigarettes affects almost every organ in the body and is associated with both a shorter and lower quality of life. There is no safe level of smoking – every cigarette increases your chances of developing a range of cancers, heart disease and diabetes.
Even if you have been smoking for years, by giving up smoking at any age you can experience health benefits almost immediately, and you can reverse many of the harmful effects of smoking.
If you’re thinking of switching to vapes as a healthy long term option, think again. The long term health effects of vaping are not fully understood and they come with their own health risks.
5. Prioritise social connection
When we talk about living healthier and longer, we tend to focus on what we do to our physical bodies. But one of the most important discoveries over the past decade has been the recognition of the importance of spiritual and psychological health.
People who are lonely and socially isolated have a much higher risk of dying early and are more likely to suffer from heart disease, stroke, dementia as well as anxiety and depression.
Although we don’t fully understand the mechanisms, it’s likely due to both behavioural and biological factors. While people who are more socially connected are more likely to engage in healthy behaviours, there also seems to be a more direct physiological effect of loneliness on the body.
So if you want to be healthier and live longer, build and maintain your connections to others.
Hassan Vally, Associate Professor, Epidemiology, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Ear Today, Gone Tomorrow
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Have just had microsuction to remove wax from my ears. A not unpleasant experience but would appreciate your guidance on how best to discourage the buildup of wax in the first place.❞
Well, certainly do not prod or poke it, and that includes with cotton buds (Q-Tips, for the Americans amongst us). That pushes more down than that it extracts, and creates a denser base of wax.
There is no evidence that ear candles help, and they can cause harm.
Further reading: Experts update best practices for diagnosis and treatment of earwax (cerumen impaction)
Ear drops can help, and if you want a home-remedy edition, olive oil or almond oil can be used; these oils dissolve the wax quite quickly (in fancier words: they are cerumenolytic agents); washing with water (e.g. in the shower or bath) is then all that’s needed. However, to avoid infection, ensure you are using a high-purity oil, and get one to use just for that; don’t just grab a bottle from the kitchen.
For your convenience, here is an example of medical grade almond oil (with dropper!) on Amazon
❝Every article had relevance to me. I ❤️ whole fruit, it’s my go to treat. I use ice packs to ease my arthritic knee pain, works well. I’ve read and loved Dr Gawande’s books. Great handful of almonds today❞
While this wasn’t a question, and we don’t usually publish feedback here, I (your writer here, hi) misread that as “ice picks” in the first instance, an implement we’ve probably all wanted to use to relieve pain at some point, but certainly not recommendable! Anyway, the momentary confusion made me smile, so I thought I’d share the silly thought. Smiling is infectious, and all that… And it’s certainly good for the health!
More seriously, glad you enjoyed!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Sweet Truth About Glycine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Make Your Collagen Work Better
This is Dr. James Nicolantonio. He’s a doctor of pharmacy, and a research scientist. He has a passion for evidence-based nutrition, and has written numerous books on the subject.
Controversy! Dr. DiNicolatonio’s work has included cardiovascular research, in which field he has made the case for increasing (rather than decreasing) the recommended amount of salt in our diet. This, of course, goes very much against the popular status quo.
We haven’t reviewed that research so we won’t comment on it here, but we thought it worth a mention as a point of interest. We’ll investigate his claims in that regard another time, though!
Today, however, we’ll be looking at his incisive, yet not controversial, work pertaining to collagen and glycine.
A quick recap on collagen
We’ve written about collagen before, and its importance for maintaining… Well, pretty much most of our body, really, buta deficiency in collagen can particularly weaken bones and joints.
On a more surface level, collagen’s also important for healthy elastic skin, and many people take it for that reason alone,
Since collagen is found only in animals, even collagen supplements are animal-based (often marine collagen or bovine collagen). However, if we don’t want to consume those, we can (like most animals) synthesize it ourselves from the relevant amino acids, which we can get from plants (and also laboratories, in some cases).
You can read our previous article about this, here:
We Are Such Stuff As Fish Are Made Of
What does he want us to know about collagen?
We’ll save time and space here: first, he’d like us to know the same as what we said in our article above
However, there is also more:
Let’s assume that your body has collagen to process. You either consumed it, or your body has synthesized it. We’ll skip describing the many steps of collagen synthesis, fascinating as that is, and get to the point:
When our body weaves together collagen fibrils out of the (triple-helical) collagen molecules…
- the cross-linking of the collagen requires lysyl oxidase
- the lysyl oxidase (which we make inside us) deanimates some other amino acids yielding aldehydes that allow the stable cross-links important for the high tensile strength of collagen, but to do that, it requires copper
- in order to use the copper it needs to be in its reduced cuprous form and that requires vitamin C
- but moving it around the body requires vitamin A
So in other words: if you are taking (or synthesizing) collagen, you also need copper and vitamins A and C.
However! Just to make things harder, if you take copper and vitamin C together, it’ll reduce the copper too soon in the wrong place.
Dr. DiNicolantonio therefore advises taking vitamin C after copper, with a 75 minutes gap between them.
What does he want us to know about glycine?
Glycine is one of the amino acids that makes up collagen. Specifically, it makes up every third amino acid in collagen, and even more specifically, it’s also the rate-limiting factor in the formation of glutathione, which is a potent endogenous (i.e., we make it inside us) antioxidant that works hard to fight inflammation inside the body.
What this means: if your joints are prone to inflammation, being glycine-deficient means a double-whammy of woe.
As well as being one of the amino acids most key to collagen production, glycine has another collagen-related role:
First, the problem: as we age, glycated collagen accumulates in the skin and cartilage (that’s bad; there is supposed to be collagen there, but not glycated).
More on glycation and what it is and why it is so bad:
Are You Eating Advanced Glycation End-Products? The Trouble Of The AGEs
Now, the solution: glycine suppresses advanced glycation end products, including the glycation of collagen.
See for example:
With these three important functions of glycine in mind…
Dr. DiNicolantonio therefore advises getting glycine at a dose of 100mg/kg/day. So, if you’re the same size as this rather medium-sized writer, that means 7.2g/day.
Where can I get it?
Glycine is found in many foods, including gelatin for those who eat that, eggs for the vegetarians, and spinach for vegans.
However, if you’d like to simply take it as a supplement, here’s an example product on Amazon
(the above product is not clear whether it’s animal-derived or not, so if that’s important to you, shop around. This writer got some locally that is certified vegan, but is in Europe rather than N. America, which won’t help most of our subscribers)
Note: pure glycine is a white crystalline powder that has the same sweetness as glucose. Indeed, that is how it got its name, from the Greek “γλυκύς”, pronounced /ɡly.kýs/, meaning “sweet”. Yes, same etymology as glucose.
So don’t worry that you’ve been conned if you order it and think “this is sugar!”; it just looks and tastes the same.
That does mean you should buy from a reputable source though, as a con would be very easy!
this does also mean that if you like a little sugar/sweetener in your tea or coffee, glycine can be used as a healthy substitute.
If you don’t like sweet tastes, then, condolences. This writer pours two espresso coffees (love this decaffeinated coffee that actually tastes good), puts the glycine in the first, and then uses the second to get rid of the sweet taste of the first. So that’s one way to do it.
Enjoy (if you can!)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Severe Complications for Pregnant Veterans Nearly Doubled in the Last Decade, a GAO Report Finds
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
Series: Post-Roe America:Abortion Access Divides the Nation
After the Supreme Court overturned Roe v. Wade, ending nearly 50 years of federal protection for abortion, some states began enforcing strict abortion bans while others became new havens for the procedure. ProPublica is investigating how sweeping changes to reproductive health care access in America are affecting people, institutions and governments.
Over the past decade, the rate of veterans suffering severe pregnancy complications has risen dramatically, a new federal report found.
Veterans have raced to the hospital with dangerous infections, kidney failure, aneurysms or blood loss. They’ve required hysterectomies, breathing machines and blood transfusions to save their lives. Between 2011 and 2020, 13 veterans died after such complications.
The report found that among people getting health care benefits through the Department of Veterans Affairs, the rate of severe complications nearly doubled during that time, from about 93 per 10,000 hospitalizations in 2011 to just over 184 per 10,000 hospitalizations in 2020. Black veterans had the highest rates.
The report, which was put together by the Government Accountability Office, also made recommendations for reducing the problem, which focus on conducting more routine screenings throughout pregnancy and in the postpartum period.
“It is imperative that the VA help ensure veterans have the healthiest pregnancy outcomes possible,” the report said, highlighting the increasing number of veterans using the agency’s maternity benefits as well as the troublesome complication rates faced by Black women.
The report’s findings are an unfortunate trend, said Alyssa Hundrup, director of health care at the GAO. The office analyzed data on 40,000 hospitalizations related to deliveries paid for by the VA. It captures a time period before 21 states banned or greatly restricted abortion and the military was thrust into a political battle over whether it would pay for active service members to travel for abortion care if a pregnancy was a risk to their health.
Hundrup, who led the review, said the analysis included hospital records from days after delivery to a year postpartum. The report was mandated after Congress passed a law in 2021 that aimed to address the maternal health crisis among veterans. The law led to a $15 million investment in maternity care coordination programs for veterans.
The report recommended that the VA analyze and collect more data on severe complications as well as data on the mental health, race and ethnicity of veterans who experience complications to understand the causes behind the increase and the reasons for the disparity. The report also states that oversight is needed to ensure screenings are being completed.
Studies show there’s a connection between mental health conditions and pregnancy-related complications, VA officials said.
The report recommended expanding the screening questions that providers ask patients at appointments to glean more information about their mental health, including anxiety and PTSD symptoms. It urged the VA to review the data more regularly.
“You don’t know what you don’t measure,” Hundrup said in an interview with ProPublica.
The VA health system, which historically served a male population, does not provide maternity care at its facilities. Instead, the agency has outsourced maternity care. But when patients were treated by those providers, the VA failed to track whether they were getting screened for other health issues and mental health problems.
Officials hope the improved data collection will help the VA study underlying issues that may lead to complications. For example, do higher rates of anxiety have a connection to rates of high blood pressure in pregnant people?
VA officials are working with a maternal health review committee to monitor the data as it is gathered. The agency recently conducted its first review of data going back five years about pregnancy-related complications, said Dr. Amanda Johnson, acting head of the VA’s Office of Women’s Health, who is overseeing the implementation of the report’s recommendations.
The VA has created a dashboard to monitor pregnant veterans’ health outcomes. The VA’s data analysis team will also examine the impact of veterans’ ages on complications and whether they differ for people who live in urban and rural areas.
VA officials will begin to review mental health screenings conducted by maternal care coordinators in March. The coordinators advocate for veterans, helping them between health care visits, whether their providers are inside or outside the VA.
Johnson said that reducing racial and ethnic disparities is a priority for the agency. In 2018, ProPublica published “Lost Mothers,” a series that shed light on the country’s maternal health crisis. Studies have shown that in the general population, Black women are three times more likely than white women to die from pregnancy-related complications. While deaths made up only a small portion of the bad outcomes for Black veterans cited in the report, VA care could not spare them from elevated rates of severe complications. Johnson said the maternal health crisis also persists within the VA.
“There is a disparity,” Johnson said. “We are not immune to that.”
Research shows pregnant people who have used the VA’s coverage have higher rates of trauma and mental conditions that can increase their risks of complications and bad outcomes.
This may be because many people who join the military enter it having already faced trauma, said Dr. Laura Miller, a psychiatrist and the medical director of reproductive mental health at the VA.
She said veterans with PTSD have higher rates of complications such as preeclampsia, a potentially fatal condition related to high blood pressure, gestational diabetes and postpartum depression. If untreated during pregnancy, depression also increases the likelihood of preterm birth and lingering problems for babies.
Hundrup said she hopes this proactive work will improve maternal health.
“We want these numbers trending in the other direction,” Hundrup said.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: