Lower Cholesterol Naturally
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Lower Cholesterol, Without Statins
We’ll start this off by saying that lowering cholesterol might not, in fact, be critical or even especially helpful for everyone, especially in the case of women. We covered this more in our article about statins:
…which was largely informed by the wealth of data in this book:
The Truth About Statins – by Dr. Barbara H. Roberts
…which in turn, may in fact put a lot of people off statins. We’re not here to tell you don’t use them—they may indeed be useful or even critical for some people, as Dr. Roberts herself also makes makes clear. But rather, we always recommend learning as much as possible about what’s going on, to be able to make the most informed choices when it comes to what often might be literally life-and-death decisions.
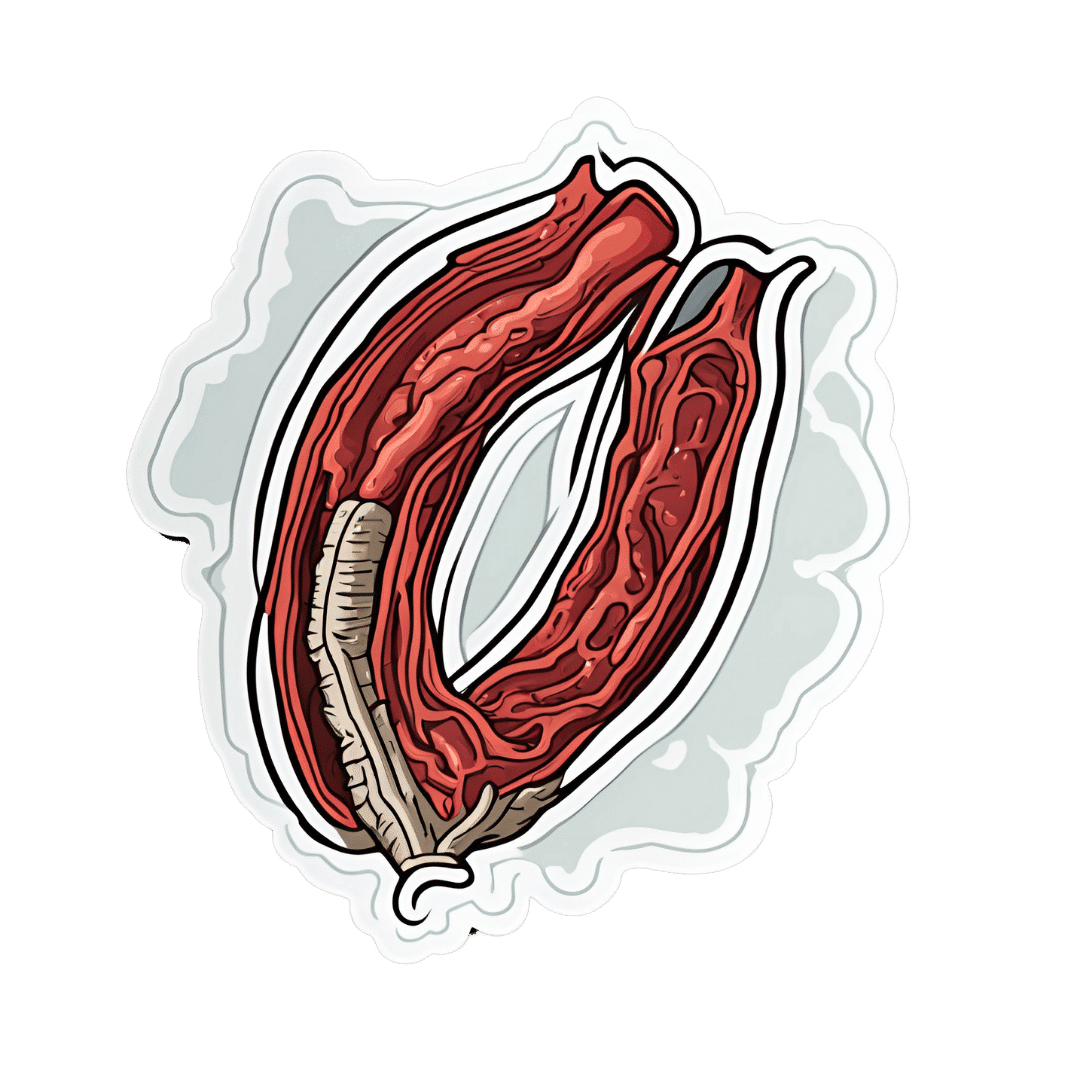
On which note, if anyone would like a quick refresher on cholesterol, what it actually is (in its various forms) and what it does, why we need it, the problems it can cause anyway, then here you go:
Now, with all that in mind, we’re going to assume that you, dear reader, would like to know:
- how to lower your LDL cholesterol, and/or
- how to maintain a safe LDL cholesterol level
Because, while the jury’s out on the dangers of high LDL levels for women in particular, it’s clear that for pretty much everyone, maintaining them within well-established safe zones won’t hurt.
Here’s how:
Relax
Or rather, manage your stress. This doesn’t just reduce your acute risk of a heart attack, it also improves your blood metrics along the way, and yes, that includes not just blood pressure and blood sugars, but even triglycerides! Here’s the science for that, complete with numbers:
What are the effects of psychological stress and physical work on blood lipid profiles?
With that in mind, here’s…
How To Manage Chronic Stress (Even While Chronically Stressed)
Not chemically “relaxed”, though
While relaxing is important, drinking alcohol and smoking are unequivocally bad for pretty much everything, and this includes cholesterol levels:
Can We Drink To Good Health? ← this also covers popular beliefs about red wine and heart health, and the answer is no, we cannot
As for smoking, it is good to quit as soon as possible, unless your doctor specifically advises you otherwise (there are occasional situations where something else needs to be dealt with first, but not as many some might like to believe):
Addiction Myths That Are Hard To Quit
If you’re wondering about cannabis (CBD and/or THC), then we’d love to tell you about the effect these things have on heart health in general and cholesterol levels in particular, but the science is far too young (mostly because of the historic, and in some places contemporary, illegality cramping the research), and we could only find small, dubious, mutually contradictory studies so far. So the honest answer is: science doesn’t know this one, yet.
Exercise… But don’t worry, you can still stay relaxed
When it comes to heart health, the most important thing is keeping moving, so getting in those famous 150 minutes per week of moderate exercise is critical, and getting more is ideal.
240 minutes per week is a neat 40 minutes per day, by the way and is very attainable (this writer lives a 20-minute walk away from where she does her daily grocery shopping, thus making for a daily 40-minute round trip, not counting the actual shopping).
See: The Doctor Who Wants Us To Exercise Less, And Move More
If walking is for some reason not practical for you, here’s a whole list of fun options that don’t feel like exercise but are:
Manage your hormones
This one is mostly for menopausal women, though some people with atypical hormonal situations may find it applicable too.
Estrogen protects the heart… Until it doesn’t:
See also: World Menopause Day: Menopause & Cardiovascular Disease Risk
Here’s a great introduction to sorting it out, if necessary:
Dr. Jen Gunter: What You Should Have Been Told About Menopause Beforehand
Eat a heart-healthy diet
Shocking nobody, but it has to be said, for the sake of being methodical. So, what does that look like?
What Matters Most For Your Heart? Eat More (Of This) For Lower Blood Pressure
(it’s fiber in the #1 spot, but there’s a list of most important things there, that’s worth checking out and comparing it to what you habitually eat)
You can also check out the DASH (Dietary Approaches to Stop Hypertension) edition of the Mediterranean diet, here:
Four Ways To Upgrade The Mediterranean Diet
As for saturated fat (and especially trans-fats), the basic answer is to keep them to minimal, but there is room for nuance with saturated fats at least:
Can Saturated Fats Be Healthy?
And lastly, do make sure to get enough omega 3 fatty-acids:
What Omega-3s Really Do For Us
And enjoy plant sterols and stanols! This would need a whole list of their own, so here you go:
Take These To Lower Cholesterol! (Statin Alternatives)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eyes for Alzheimer’s Diagnosis: New?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Time!
This is the bit whereby each week, we respond to subscriber questions/requests/etc
Have something you’d like to ask us, or ask us to look into? Hit reply to any of our emails, or use the feedback widget at the bottom, and a Real Human™ will be glad to read it!
Q: As I am a retired nurse, I am always interested in new medical technology and new ways of diagnosing. I have recently heard of using the eyes to diagnose Alzheimer’s. When I did some research I didn’t find too much. I am thinking the information may be too new or I wasn’t on the right sites.
(this is in response to last week’s piece on lutein, eyes, and brain health)
We’d readily bet that the diagnostic criteria has to do with recording low levels of lutein in the eye (discernible by a visual examination of macular pigment optical density), and relying on the correlation between this and incidence of Alzheimer’s, but we’ve not seen it as a hard diagnostic tool as yet either—we’ll do some digging and let you know what we find! In the meantime, we note that the Journal of Alzheimer’s Disease (which may be of interest to you, if you’re not already subscribed) is onto this:
See also:
- Journal of Alzheimer’s Disease (mixture of free and paid content)
- Journal of Alzheimer’s Disease Reports (open access—all content is free)
Share This Post
-
What families should know about whooping cough
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- Whooping cough is a bacterial respiratory illness that can cause long-term symptoms and even death.
- Two types of vaccines protect against it: The DTap vaccine is given to babies and children up to 6 years old, while the Tdap vaccine is given to children 7 years and older and adults.
- If you or your child has symptoms of whooping cough, isolate them from vulnerable family members and seek treatment early to reduce the risk of serious illness.
Whooping cough, also called pertussis, is a highly contagious respiratory illness that’s particularly dangerous for babies. Cases are now at least four times as high as they were at this time last year. Fortunately, vaccines are extremely effective at preventing the disease across age groups.
Read on to learn about the symptoms and risks of whooping cough, who should get vaccinated, and what to do when symptoms appear.What are the symptoms of whooping cough?
Early symptoms of whooping cough typically appear five to 10 days after exposure and may include a runny or stuffy nose, a low fever, and a mild cough. One to two weeks later, some people may experience extreme coughing fits that can cause shortness of breath, trouble sleeping, vomiting, fatigue, and rib fractures. These fits usually last one to six weeks, but they can last up to 10 weeks after infection.
About one in three babies under 1 year old who contract whooping cough require hospitalization, as they may experience life-threatening pauses in breathing (called apnea), pneumonia, and other complications. Children and adults who have asthma or are immunocompromised are also more likely to develop severe symptoms.
Which vaccines protect against whooping cough, and who is eligible?
Two types of vaccines protect against whooping cough: The DTap vaccine is given to babies and children up to 6 years old, while the Tdap vaccine is given to children 7 years and older and adults. Both vaccines protect against infections from diptheria, tetanus, and pertussis.
The Centers for Disease Control and Prevention recommends that pregnant people receive a single dose of the Tdap vaccine between 27 and 36 weeks of pregnancy, as this lowers the risk of whooping cough in babies younger than 2 months old by 78 percent.
Multiple doses are required for the best protection. Learn more about DTaP and Tdap vaccine schedules from the CDC, and talk to your health care provider about how many doses you and your children need.
What should families do when whooping cough symptoms appear?
If you or your child has symptoms of whooping cough, isolate the infected person from vulnerable family members. It’s also important to seek treatment early to reduce the risk of serious illness. Health care providers typically prescribe antibiotics to those recovering at home.
Over-the-counter cough and cold medicine is not recommended for children under 4 years old. However, limiting smoke, dust, and chemical fumes at home and using a humidifier can reduce coughing. If you are caring for someone with whooping cough who exhibits pauses in breathing or develops gray or blue skin, call 911 immediately.
For more information, talk to your health care provider.Share This Post
-
The Good, The Bad, & The Vigorously Debated
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This week in health news sees some pretty varied topics:
One more reason to care about the gut-brain axis
Stroke is a top killer in much of the industrialized world, usually making it into the top-few list on a per-country basis. And, it’s rising in prevalence, too. This is partly because our longevity is increasing so age-related things kill us more often, statistically, than age-unrelated things. But that’s only part of the reason; another is that our lifestyle (on the national level) is becoming more conducive to stroke. Diet is a large contributor to that, and gut health has now been identified as a key factor.
What recent research has shown is that minutes after a stroke occurs, normal gut anatomy is disrupted, and cells responsible for gut barrier integrity are eroded, and bugs from the gut get into the blood, and arrive at the (newly damaged) brain vasculature, where the blood-brain barrier is often also compromised on account of the stroke.
Because of this, critical to reducing post-stroke neuroinflammation (something that makes stroke damage more severe and recovery a lot harder) is improving the gut’s ability to heal itself quickly.
This can be helped with a dose of Insulin-like Growth Factor (IGF-1), but there are other things that can help or hinder, and those other things are modifiable by us as individuals in our lifestyle choices (e.g. a gut-healthy diet with plenty of fiber, and avoiding gut-unhealthy things like sugar and alcohol that feed C. albicans growths that will put roots through your intestines and make holes as they do), because the better/worse your gut barrier integrity is to start with, the easier/harder it will be for your gut to repair itself quickly:
Read in full: Healing the gut can reduce long-term impact of stroke
Related: Stop Sabotaging Your Gut
How about that seasonal lead-spiced hot drink?
Lead contamination in ground spices has become a bit of an issue, ground turmeric has had quite some flak in this regard, and now the spotlight is on cinnamon.
These reports, by the way, do not specify what kind of cinnamon (i.e. cassia vs Ceylon), however, clicking through to assorted sources and then doing our own digging finds that all cinnamon products we found listed as contaminated, were cassia cinnamon. This is unsurprising, as a) it’s cheaper b) it’s the kind most readily found on shelves in the US. That said, when it comes to Ceylon (sweet) cinnamon, absence of evidence is not evidence of absence, so that doesn’t mean they got the all-clear on lead contamination, but rather, that they haven’t received the same scrutiny as yet.
It’s worth noting that cinnamon sticks have been found to have less contamination than ground cinnamon, though.
It’s also worth noting that since some adulterated products have had lead added deliberately in increase the weight and darken the color, this is more likely to happen to cassia cinnamon than sweet cinnamon because cassia cinnamon is visibly darker, so adding a darkening agent to sweet cinnamon would just make it look like cassia (which no seller would want to do since cassia is the cheaper of the two).
Read in full: Why lead-tainted cinnamon products have turned up on shelves, and what questions consumers should ask
Related: Sweet Cinnamon vs Regular Cinnamon – Which is Healthier? ← this also covers toxicity issues, by the way
A matter of life and death
Assisted dying is currently legal in 10/40 US states, and Canada. Over in the UK, it’s being debated (and voted on) in Parliament today, at time of writing.
While bodily autonomy discussions are usually quite straightforward arguments between the very separate camps of
- “my body, my choice” vs
- “they shouldn’t be allowed to do that”,
…this one comes with a considerable middleground, because
- “people should have to right to end things without extra suffering and on their own terms”, and
- “many disabled people fear being placed in a position of having justify why they are not exercising their right to die when it might be cheaper and easier for others if they did”
…are positions with a lot of potential overlap.
In any case, we know most of our readers are in the US, but with a 10/40 split in US states (and some recent controversies in Canada), it’s likely a topic that’ll come up for most people at some point, so it’s good to understand it, and this is as good an opportunity as any:
Read in full: How would the assisted dying bill work and what issues might it create?
Related: Managing Your Mortality ← this talks about psychological/social considerations, as well as end-of-life care, palliative care (which is not quite the same thing!) and euthanasia in various forms, including the unofficial kind that you might want to be aware of if you want to avoid that happening.
Take care!
Share This Post
Related Posts
-
The Vitamin Solution – by Dr. Romy Block & Dr. Arielle Levitan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A quick note: it would be remiss of us not to mention that the authors of this book are also the founders of a vitamin company, thus presenting a potential conflict of interest.
That said… In this reviewer’s opinion, the book does seem balanced and objective, regardless.
We talk a lot about supplements here at 10almonds, especially in our Monday Research Review editions. And yesterday, we featured a book by a doctor who hates supplements. Today, we feature a book by two doctors who have made them their business.
The authors cover all the most common vitamins and minerals popularly enjoyed as supplements, and examine:
- why people take them
- factors affecting whether they help
- problems that can arise
- complicating factors
The “complicating factors” include, for example, the way many vitamins and/or minerals interplay with each other, either by requiring the presence of another, or else competing for resources for absorption, or needing to be delicately balanced on pain of diverse woes.
This is the greatest value of the book, perhaps; it’s where most people go wrong with supplementation, if they go wrong.
While both authors are medical doctors, Dr. Romy Block is an endocrinologist specifically, and she clearly brought a lot of extra attention to relevant metabolic/thyroid issues, and how vitamins and minerals (such as thiamin and iron) can improve or sabotage such, depending on various factors that she explains. Informative, and so far as this reviewer could see, objective and well-balanced.
Bottom line: supplementation is a vast and complex topic, but this book does a fine job of demystifying and simplifying it in a clear and objective fashion, without resorting to either scaremongering or hype.
Click here to check out The Vitamin Solution, and upgrade your knowledge!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Your Diet May Be Causing Chronic Tightness (& How To Fix It)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There is often more to hamstring flexibility than just stretching:
Three steps
The method focuses on three areas: diet, mindset, and movement.
Why diet? Poor gut health and inflammation, often caused by processed and fast foods, contribute to chronic hamstring tightness. The video suggests nutrient-dense meals like Greek yogurt with poached eggs. As for collagen, that is found most abundantly in the bones and skin of fish and other animals, but if you are vegan/vegetarian, fear not, you can just make sure to eat plenty of its constituent parts instead, and synthesize it yourself like any other animal. See also: The Best Foods For Collagen Production
Why mindset? Addressing pain and other somatic (bodily) concerns involves understanding the body as a single interconnected system. So, it’s necessary to also take care of any emotional stress or other underlying conditions, as well as ensuring your hormones are all in order.
Why movement? Machine-based training, which isolates muscles, can cause imbalances. Instead, consider functional movements like hanging and compound exercises such as Pilates or other calisthenics systems. These improve core strength, enhance flexibility, and prevent stiffness, ensuring better overall function.
Some example exercises:
- Bent knee hamstring stretch: hold for 2 seconds; do 10–12 reps (2 sets per leg).
- Straight leg active isolation: focus on quad engagement with assistance from a band; 10–12 reps (2 sets per leg).
- Active hip abductors: target IT band and glute medius; 1 set of 12 reps per leg.
- Active lunge stretch: incorporate a band to intensify the stretch; 2 seconds at the top range.
For more on all of this plus visual demonstrations of the exercises, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Fix Tight Hamstrings In Just 3 Steps
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
With Medical Debt Burdening Millions, a Financial Regulator Steps In to Help
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When President Barack Obama signed legislation in 2010 to create the Consumer Financial Protection Bureau, he said the new agency had one priority: “looking out for people, not big banks, not lenders, not investment houses.”
Since then, the CFPB has done its share of policing mortgage brokers, student loan companies, and banks. But as the U.S. health care system turns tens of millions of Americans into debtors, this financial watchdog is increasingly working to protect beleaguered patients, adding hospitals, nursing homes, and patient financing companies to the list of institutions that regulators are probing.
In the past two years, the CFPB has penalized medical debt collectors, issued stern warnings to health care providers and lenders that target patients, and published reams of reports on how the health care system is undermining the financial security of Americans.
In its most ambitious move to date, the agency is developing rules to bar medical debt from consumer credit reports, a sweeping change that could make it easier for Americans burdened by medical debt to rent a home, buy a car, even get a job. Those rules are expected to be unveiled later this year.
“Everywhere we travel, we hear about individuals who are just trying to get by when it comes to medical bills,” said Rohit Chopra, the director of the CFPB whom President Joe Biden tapped to head the watchdog agency in 2021.
“American families should not have their financial lives ruined by medical bills,” Chopra continued.
The CFPB’s turn toward medical debt has stirred opposition from collection industry officials, who say the agency’s efforts are misguided. “There’s some concern with a financial regulator coming in and saying, ‘Oh, we’re going to sweep this problem under the rug so that people can’t see that there’s this medical debt out there,’” said Jack Brown III, a longtime collector and member of the industry trade group ACA International.
Brown and others question whether the agency has gone too far on medical billing. ACA International has suggested collectors could go to court to fight any rules barring medical debt from credit reports.
At the same time, the U.S. Supreme Court is considering a broader legal challenge to the agency’s funding that some conservative critics and financial industry officials hope will lead to the dissolution of the agency.
But CFPB’s defenders say its move to address medical debt simply reflects the scale of a crisis that now touches some 100 million Americans and that a divided Congress seems unlikely to address soon.
“The fact that the CFPB is involved in what seems like a health care issue is because our system is so dysfunctional that when people get sick and they can’t afford all their medical bills, even with insurance, it ends up affecting every aspect of their financial lives,” said Chi Chi Wu, a senior attorney at the National Consumer Law Center.
CFPB researchers documented that unpaid medical bills were historically the most common form of debt on consumers’ credit reports, representing more than half of all debts on these reports. But the agency found that medical debt is typically a poor predictor of whether someone is likely to pay off other bills and loans.
Medical debts on credit reports are also frequently riddled with errors, according to CFPB analyses of consumer complaints, which the agency found most often cite issues with bills that are the wrong amount, have already been paid, or should be billed to someone else.
“There really is such high levels of inaccuracy,” Chopra said in an interview with KFF Health News. “We do not want to see the credit reporting system being weaponized to get people to pay bills they may not even owe.”
The aggressive posture reflects Chopra, who cut his teeth helping to stand up the CFPB almost 15 years ago and made a name for himself going after the student loan industry.
Targeting for-profit colleges and lenders, Chopra said he was troubled by an increasingly corporate higher-education system that was turning millions of students into debtors. Now, he said, he sees the health care system doing the same thing, shuttling patients into loans and credit cards and reporting them to credit bureaus. “If we were to rewind decades ago,” Chopra said, “we saw a lot less reliance on tools that banks used to get people to pay.”
The push to remove medical bills from consumer credit reports culminates two years of intensive work by the CFPB on the medical debt issue.
The agency warned nursing homes against forcing residents’ friends and family to assume responsibility for residents’ debts. An investigation by KFF Health News and NPR documented widespread use of lawsuits by nursing homes in communities to pursue friends and relatives of nursing home residents.
The CFPB also has highlighted problems with how hospitals provide financial assistance to low-income patients. Regulators last year flagged the dangers of loans and credit cards that health care providers push on patients, often saddling them with more debt.
And regulators have gone after medical debt collectors. In December, the CFPB shut down a Pennsylvania company for pursuing patients without ensuring the debts were accurate.
A few months before that, the agency fined an Indiana company working with medical debt for violating collection laws. Regulators said the company had “risked harming consumers by pressuring or inducing them to pay debts they did not owe.”
With their business in the crosshairs, debt collectors are warning that cracking down on credit reporting and other collection tools may prompt more hospitals and doctors to demand patients pay upfront for care.
There are some indications this is happening already, as hospitals and clinics push patients to enroll in loans or credit cards to pay their medical bills.
Scott Purcell, CEO of ACA International, said it would be wiser for the federal government to focus on making medical care more affordable. “Here we’re coming up with a solution that only takes money away from providers,” Purcell said. “If Congress was involved, there could be more robust solutions.”
Chopra doesn’t dispute the need for bigger efforts to tackle health care costs.
“Of course, there are broader things that we would probably want to fix about our health care system,” he said, “but this is having a direct financial impact on so many Americans.”
The CFPB can’t do much about the price of a prescription or a hospital bill, Chopra continued. What the federal agency can do, he said, is protect patients if they can’t pay their bills.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: