Loaded Mocha Chocolate Parfait
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Packed with nutrients, including a healthy dose of protein and fiber, these parfait pots can be a healthy dessert, snack, or even breakfast!
You will need (for 4 servings)
For the mocha cream:
- ½ cup almond milk
- ½ cup raw cashews
- ⅓ cup espresso
- 2 tbsp maple syrup
- 1 tsp vanilla extract
For the chocolate sauce:
- 4 tbsp coconut oil, melted
- 2 tbsp unsweetened cocoa powder
- 1 tbsp maple syrup
- 1 tsp vanilla extract
For the other layers:
- 1 banana, sliced
- 1 cup granola, no added sugar
Garnish (optional): 3 coffee beans per serving
Note about the maple syrup: since its viscosity is similar to the overall viscosity of the mocha cream and chocolate sauce, you can adjust this per your tastes, without affecting the composition of the dish much besides sweetness (and sugar content). If you don’t like sweetness, the maple syrup be reduced or even omitted entirely (your writer here is known for her enjoyment of very strong bitter flavors and rarely wants anything sweeter than a banana); if you prefer more sweetness than the recipe called for, that’s your choice too.
Method
(we suggest you read everything at least once before doing anything)
1) Blend all the mocha cream ingredients. If you have time, doing this in advance and keeping it in the fridge for a few hours (or even up to a week) will make the flavor richer. But if you don’t have time, that’s fine too.
2) Stir all the chocolate sauce ingredients together in a small bowl, and set it aside. This one should definitely not be refrigerated, or else the coconut oil will solidify and separate itself.
3) Gently swirl the the mocha cream and chocolate sauce together. You want a marble effect, not a full mixing. Omit this step if you want clearer layers.
4) Assemble in dessert glasses, alternating layers of banana, mocha chocolate marble mixture (or the two parts, if you didn’t swirl them together), and granola.
5) Add the coffee-bean garnish, if using, and serve!

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Enjoy Bitter Foods For Your Heart & Brain
- The Bitter Truth About Coffee (Or Is It?)
- Which Sugars Are Healthier, And Which Are Just The Same?
- Cashew Nuts vs Coconut – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What To Leave Off Your Table (To Stay Off This Surgeon’s)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Why we eat too much (and how we can fix that)
This is Dr. Andrew Jenkinson. He’s a Consultant Surgeon specializing in the treatment of obesity, gallstones, hernias, heartburn and abdominal pain. He runs regular clinics in both London and Dubai. What he has to offer us today, though, is insight as to what’s on our table that puts us on his table, and how we can quite easily change that up.
So, why do we eat too much?
First things first: some metabolic calculations. No, we’re not going to require you to grab a calculator here… Your body does it for you!
Our body’s amazing homeostatic system (the system that does its best to keep us in the “Goldilocks Zone” of all our bodily systems; not too hot or too cold, not dehydrated or overhydrated, not hyperglycemic or hypoglycemic, blood pressure not too high or too low, etc, etc) keeps track of our metabolic input and output.
What this means: if we increase or decrease our caloric consumption, our body will do its best to increase or decrease our metabolism accordingly:
- If we don’t give it enough energy, it will try to conserve energy (first by slowing our activities; eventually by shutting down organs in a last-ditch attempt to save the rest of us)
- If we give it too much energy, it will try to burn it off, and what it can’t burn, it will store
In short: if we eat 10% or 20% more or less than usual, our body will try to use 10% to 20% more or less than usual, accordingly.
So… How does this get out of balance?
The problem is in how our system does that, and how we inadvertently trick it, to our detriment.
For a system to function, it needs at its most base level two things—a sensor and a switch:
- A sensor: to know what’s going on
- A switch: to change what it’s doing accordingly
Now, if we eat the way we’re evolved to—as hunter-gatherers, eating mostly fruit and vegetables, supplemented by animal products when we can get them—then our body knows exactly what it’s eating, and how to respond accordingly.
Furthermore, that kind of food takes some eating! Most fruit these days is mostly water and fiber; in those days it often had denser fiber (before agricultural science made things easier to eat), but either way, our body knows when we are eating fruit and how to handle that. Vegetables, similarly. Unprocessed animal products, again, the gut goes “we know what this is” and responds accordingly.
But modern ultra-processed foods with trans-fatty acids, processed sugar and flour?
These foods zip calories straight into our bloodstream like greased lightning. We get them so quickly so easily and in such great caloric density, that our body doesn’t have the chance to count them on the way in!
What this means is: the body has no idea what it’s just consumed or how much or what to do with it, and doesn’t adjust our metabolism accordingly.
Bottom line:
Evolutionarily speaking, your body has no idea what ultra-processed food is. If you skip it and go for whole foods, you can, within the bounds of reason, eat what you like and your body will handle it by adjusting your metabolism accordingly.
Now, advising you “avoid ultra-processed foods and eat whole foods” was probably not a revelation in and of itself.
But: sometimes knowing a little more about the “why” makes the difference when it comes to motivation.
Want to know more about Dr. Jenkinson’s expert insights on this topic?
If you like, you can check out his website here—he has a book too
Why We Eat (Too Much) – Dr. Andrew Jenkinson on the Science of Appetite
Share This Post
-
Are You Making This Alcohol Mistake?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The famous “small glass of red per day” is, as is quite well-established now in science, but not so much in popular culture, known to be not a good idea.
What most people don’t know
Rethinking “One Drink a Day”:
- Outdated beliefs and flawed studies:
- The idea that “one drink a day is healthy” stems from flawed associative studies that included…
- unhealthy former heavy drinkers in the zero-drinks category, and
- healthy older individuals who continued light drinking due to good health, not because alcohol contributed to it, in the drinkers category
- In other words, they looked at former alcoholics whose health was ruined by drinking and said “aha, non-drinkers have bad health”, and looked at the survivors of survivorship bias and said “aha, light drinking is the key to good health”. Which of course is terrible science propped up by terrible abuse of statistics propped up by shoddy methodology.
- The idea that “one drink a day is healthy” stems from flawed associative studies that included…
- New research findings:
- A 2022 UK Biobank Study showed that even one drink a day leads to brain shrinkage, neuron death, and cognitive decline.
- Another study on CVD disproved the notion that light drinking benefits heart health once confounding variables were removed.
- There are plenty more, and at 10almonds we’ve done a main feature about it, but for now, you get the idea.
Some other things you should know:
Ethanol and acetaldehyde damage neurons responsible for impulse control, judgment, motor coordination, and memory formation, leading to cognitive decline. The feeling of being drunk results from the suppression and damage of these neurons. But while the drunk feeling wears off, the damage to neurons does not.
Alcohol causes cumulative DNA damage in neurons, accelerates brain aging, and prevents the formation of new neurons, similar to a slow, gradual stroke.
Broader Health Impacts of Alcohol
We’ve said it before, and we’ll say it again: alcohol is bad for pretty much everything.
Here are some examples mentioned in the video:
- Neurodegenerative diseases: heavy drinking increases the risk of Alzheimer’s, particularly in those genetically predisposed.
- Sleep disruption: alcohol reduces deep, restful sleep and hampers the brain’s natural detox process overnight, contributing to morning grogginess.
- Inflammation and immune suppression: alcohol increases inflammation, exacerbates autoimmune diseases (like psoriasis and arthritis), and weakens immune function.
- Cancer risk: alcohol is classified as a Group 1 carcinogen by the International Agency for Research on Cancer, linked to various cancers, especially breast cancer. Even light drinking increases breast cancer risk.
- Hormonal imbalances: in women, alcohol heightens PMS symptoms, reduces fertility, and increases testosterone. In men, it lowers sperm quality and disrupts hormones.
For more on all of these and more, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Can We Drink To Good Health? ← this is mostly about red wine and heart health
- How To Reduce Or Quit Alcohol ← this is about the more general reasons to quit, and how to do so
- What Happens To Your Body When You Stop Drinking Alcohol ← a realistic timeline of recovery
Take care!
Share This Post
- Outdated beliefs and flawed studies:
-
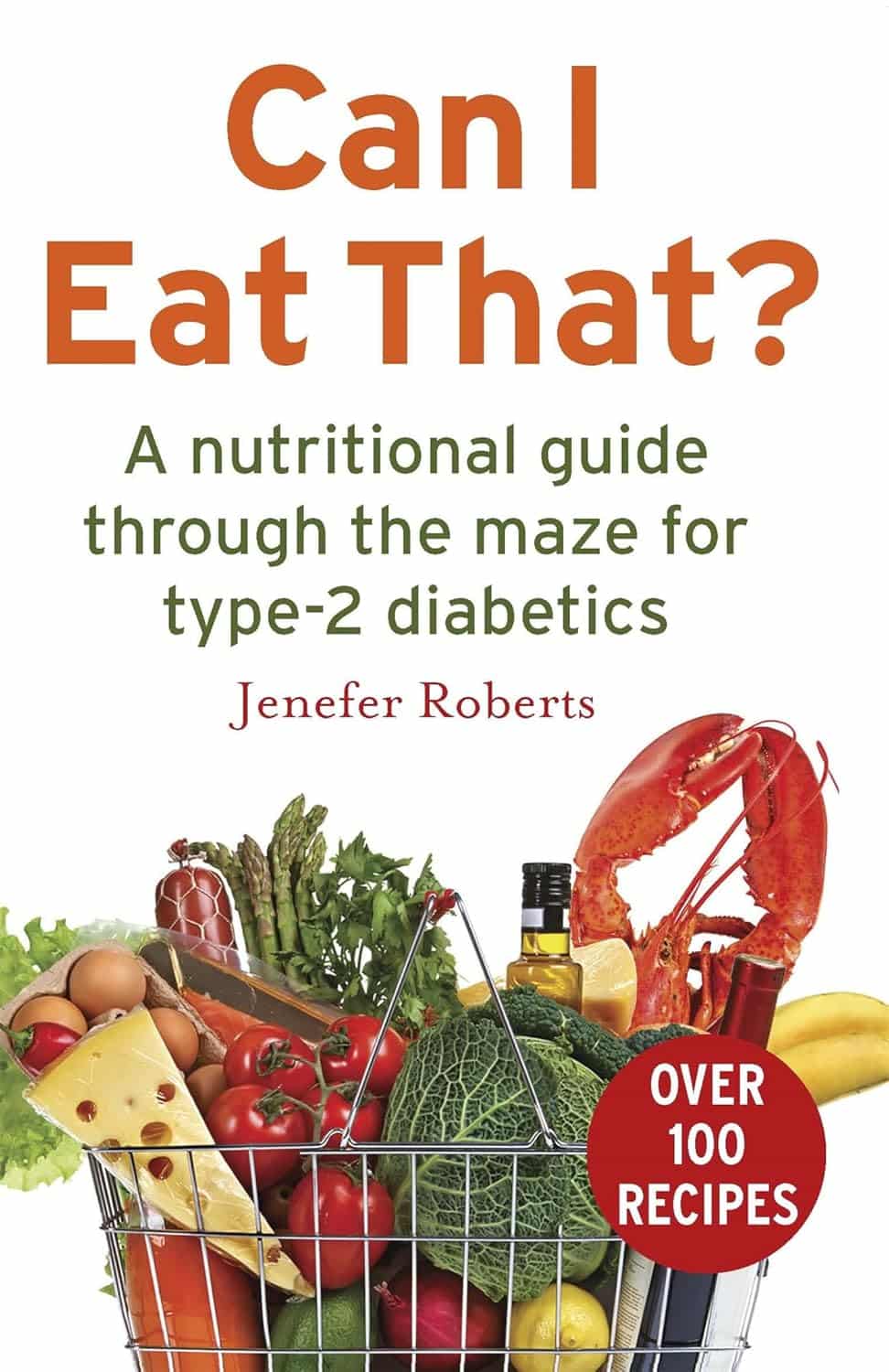
Can I Eat That? – by Jenefer Roberts
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The answer to the question in the title is: you can eat pretty much anything, if you’re prepared for the consequences!
This book looks to give you the information to make your own decisions in that regard. There’s a large section on the science of glucose metabolism in the context of food (other aspects of glucose metabolism aren’t covered), so you will not simply be told “raw carrots are good; mashed potatoes are bad”, you’ll understand many factors that affect it, e.g:
- Macronutrient profiles of food and resultant base glycemic indices
- How the glycemic index changes if you cut something, crush it, mash it, juice it, etc
- How the glycemic index changes if you chill something, heat it, fry it, boil it, etc
- The many “this food works differently in the presence of this other food” factors
- How your relative level of insulin resistance affects things itself
…and much more.
The style is simple and explanatory, without deep science, but with good science and comprehensive advice.
There are also the promised recipes; they’re in an appendix at the back and aren’t the main meat of the book, though.
Bottom line: if you’ve ever found it confusing working out what works how in the mysterious world of diabetes nutrition, this book is a top tier demystifier.
Click here to check out Can I Eat That?, and gain confidence in your food choices!
Share This Post
Related Posts
-
Hormones & Health, Beyond The Obvious
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Wholesome Health
This is Dr. Sara Gottfried, who some decades ago got her MD from Harvard and specialized as an OB/GYN at MIT. She’s since then spent the more recent part of her career educating people (mostly: women) about hormonal health, precision, functional, & integrative medicine, and the importance of lifestyle medicine in general.
What does she want us to know?
Beyond “bikini zone health”
Dr. Gottfried urges us to pay attention to our whole health, in context.
“Women’s health” is often thought of as what lies beneath a bikini, and if it’s not in those places, then we can basically treat a woman like a man.
And that’s often not actually true—because hormones affect every living cell in our body, and as a result, while prepubescent girls and postmenopausal women (specifically, those who are not on HRT) may share a few more similarities with boys and men of similar respective ages, for most people at most ages, men and women are by default quite different metabolically—which is what counts for a lot of diseases! And note, that difference is not just “faster” or “slower””, but is often very different in manner also.
That’s why, even in cases where incidence of disease is approximately similar in men and women when other factors are controlled for (age, lifestyle, medical history, etc), the disease course and response to treatment may vary considerable. For a strong example of this, see for example:
- The well-known: Heart Attack: His & Hers ← most people know these differences exist, but it’s always good to brush up on what they actually are
- The less-known: Statins: His & Hers ← most people don’t know these differences exist, and it pays to know, especially if you are a woman or care about one
Nor are brains exempt from his…
The female brain (kinda)
While the notion of an anatomically different brain for men and women has long since been thrown out as unscientific phrenology, and the idea of a genetically different brain is… Well, it’s an unreliable indicator, because technically the cells will have DNA and that DNA will usually (but not always; there are other options) have XX or XY chromosomes, which will usually (but again, not always) match apparent sex (in about 1/2000 cases there’s a mismatch, which is more common than, say, red hair; sometimes people find out about a chromosomal mismatch only later in life when getting a DNA test for some unrelated reason), and in any case, even for most of us, the chromosomal differences don’t count for much outside of antenatal development (telling the default genital materials which genitals to develop into, though this too can get diverted, per many intersex possibilities, which is also a lot more common than people think) or chromosome-specific conditions like colorblindness…
The notion of a hormonally different brain is, in contrast to all of the above, a reliable and easily verifiable thing.
See for example:
Alzheimer’s Sex Differences May Not Be What They Appear
Dr. Gottfried urges us to take the above seriously!
Because, if women get Alzheimer’s much more commonly than men, and the disease progresses much more quickly in women than men, but that’s based on postmenopausal women not on HRT, then that’s saying “Women, without women’s usual hormones, don’t do so well as men with men’s usual hormones”.
She does, by the way, advocate for bioidentical HRT for menopausal women, unless contraindicated for some important reason that your doctor/endocrinologist knows about. See also:
Menopausal HRT: A Tale Of Two Approaches (Bioidentical vs Animal)
The other very relevant hormone
…that Dr. Gottfried wants us to pay attention to is insulin.
Or rather, its scrubbing enzyme, the prosaically-named “insulin-degrading enzyme”, but it doesn’t only scrub insulin. It also scrubs amyloid beta—yes, the same that produces the amyloid beta plaques in the brain associated with Alzheimer’s. And, there’s only so much insulin-degrading enzyme to go around, and if it’s all busy breaking down excess insulin, there’s not enough left to do the other job too, and thus can’t break down amyloid beta.
In other words: to fight neurodegeneration, keep your blood sugars healthy.
This may actually work by multiple mechanisms besides the amyloid hypothesis, by the way:
The Surprising Link Between Type 2 Diabetes & Alzheimer’s
Want more from Dr. Gottfried?
You might like this interview with Dr. Gottfried by Dr. Benson at the IMCJ:
Integrative Medicine: A Clinician’s Journal | Conversations with Sara Gottfried, MD
…in which she discusses some of the things we talked about today, and also about her shift from a pharmaceutical-heavy approach to a predominantly lifestyle medicine approach.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
25 Healthy Habits That Will Change Your Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cori Lefkowith, of “Redefining Strength” and “Strong At Every Age” fame, has compiled a list of the simple habits that make a big difference, and here they are!
The Tips
Her recommendations include…
- The healthy activities you’re most prone to skipping? Do those first
- Create staple meals… Consciously! This means: instead of getting into a rut of cooking the same few things in rotation because it’s what you have the ingredients in for, consciously and deliberately make a list of at least 7 meals that, between them, constitute a healthy balanced diet, and choose to make them your staples. That doesn’t mean don’t eat anything else (indeed, variety is good!) but having a robust collection of healthy staples to fall back on will help you avoid falling into unhealthy eating traps.
- Schedule time for healthy activities that you love. Instead of thinking “it would be nice to…”, actually figure out a timeslot, plan in advance, making it recurring, and do it!
- Have (healthy!) no-spoil food options always available. No-spoil doesn’t have to mean “won’t spoil ever”, but does mean at least that it has a long shelf-life. Nuts are a good example, assuming you’re not allergic. Sundried fruits are good too; not nearly as good as fresh fruit, but a lot better than some random processed snack because it’s what in. If you eat fish, then see if you can get dried fish in; it’s high in protein and keeps for a very long time indeed.
- Stock up on spices! Not only do they all have great health-giving properties (at least, we can’t think of a refutation by counterexample, Arrakis be damned), but also, they literally spice up our culinary repertoire, and bring joy to cooking and eating healthy food.
If you like these, check out the rest:
Click Here If The Embedded Video Doesn’t Load Automatically
Further reading
For more about actually making habits stick quickly and reliably,enjoy:
How To Really Pick Up (And Keep!) Those Habits
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Viruses aren’t always harmful. 6 ways they’re used in health care and pest control
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We tend to just think of viruses in terms of their damaging impacts on human health and lives. The 1918 flu pandemic killed around 50 million people. Smallpox claimed 30% of those who caught it, and survivors were often scarred and blinded. More recently, we’re all too familiar with the health and economic impacts of COVID.
But viruses can also be used to benefit human health, agriculture and the environment.
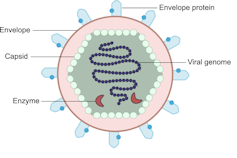
Viruses are comparatively simple in structure, consisting of a piece of genetic material (RNA or DNA) enclosed in a protein coat (the capsid). Some also have an outer envelope.
Viruses get into your cells and use your cell machinery to copy themselves.
Here are six ways we’ve harnessed this for health care and pest control.1. To correct genes
Viruses are used in some gene therapies to correct malfunctioning genes. Genes are DNA sequences that code for a particular protein required for cell function.
If we remove viral genetic material from the capsid (protein coat) we can use the space to transport a “cargo” into cells. These modified viruses are called “viral vectors”.
Viruses consist of a piece of RNA or DNA enclosed in a protein coat called the capsid.
DEXiViral vectors can deliver a functional gene into someone with a genetic disorder whose own gene is not working properly.
Some genetic diseases treated this way include haemophilia, sickle cell disease and beta thalassaemia.
2. Treat cancer
Viral vectors can be used to treat cancer.
Healthy people have p53, a tumour-suppressor gene. About half of cancers are associated with the loss of p53.
Replacing the damaged p53 gene using a viral vector stops the cancerous cell from replicating and tells it to suicide (apoptosis).
Viral vectors can also be used to deliver an inactive drug to a tumour, where it is then activated to kill the tumour cell.
This targeted therapy reduces the side effects otherwise seen with cytotoxic (cell-killing) drugs.
We can also use oncolytic (cancer cell-destroying) viruses to treat some types of cancer.
Tumour cells have often lost their antiviral defences. In the case of melanoma, a modified herpes simplex virus can kill rapidly dividing melanoma cells while largely leaving non-tumour cells alone.
3. Create immune responses
Viral vectors can create a protective immune response to a particular viral antigen.
One COVID vaccine uses a modified chimp adenovirus (adenoviruses cause the common cold in humans) to transport RNA coding for the SARS-CoV-2 spike protein into human cells.
The RNA is then used to make spike protein copies, which stimulate our immune cells to replicate and “remember” the spike protein.
Then, when you are exposed to SARS-CoV-2 for real, your immune system can churn out lots of antibodies and virus-killing cells very quickly to prevent or reduce the severity of infection.
4. Act as vaccines
Viruses can be modified to act directly as vaccines themselves in several ways.
We can weaken a virus (for an attenuated virus vaccine) so it doesn’t cause infection in a healthy host but can still replicate to stimulate the immune response. The chickenpox vaccine works like this.
The Salk vaccine for polio uses a whole virus that has been inactivated (so it can’t cause disease).
Others use a small part of the virus such as a capsid protein to stimulate an immune response (subunit vaccines).
An mRNA vaccine packages up viral RNA for a specific protein that will stimulate an immune response.
5. Kill bacteria
Viruses can – in limited situations in Australia – be used to treat antibiotic-resistant bacterial infections.
Bacteriophages are viruses that kill bacteria. Each type of phage usually infects a particular species of bacteria.
Unlike antibiotics – which often kill “good” bacteria along with the disease-causing ones – phage therapy leaves your normal flora (useful microbes) intact.
Bacteriophages (red) are viruses that kill bacteria (green).
Shutterstock6. Target plant, fungal or animal pests
Viruses can be species-specific (infecting one species only) and even cell-specific (infecting one type of cell only).
This occurs because the proteins viruses use to attach to cells have a shape that binds to a specific type of cell receptor or molecule, like a specific key fits a lock.
The virus can enter the cells of all species with this receptor/molecule. For example, rabies virus can infect all mammals because we share the right receptor, and mammals have other characteristics that allow infection to occur whereas other non-mammal species don’t.
When the receptor is only found on one cell type, then the virus will infect that cell type, which may only be found in one or a limited number of species. Hepatitis B virus successfully infects liver cells primarily in humans and chimps.
We can use that property of specificity to target invasive plant species (reducing the need for chemical herbicides) and pest insects (reducing the need for chemical insecticides). Baculoviruses, for example, are used to control caterpillars.
Similarly, bacteriophages can be used to control bacterial tomato and grapevine diseases.
Other viruses reduce plant damage from fungal pests.
Myxoma virus and calicivirus reduce rabbit populations and their environmental impacts and improve agricultural production.
Just like humans can be protected against by vaccination, plants can be “immunised” against a disease-causing virus by being exposed to a milder version.
Thea van de Mortel, Professor, Nursing, School of Nursing and Midwifery, Griffith University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: