Life Lessons From A Brain Surgeon – by Dr. Rahul Jandial
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the category of surgeons with a “what to put on your table to stay off mine” angle, this book packs an extra punch. As well as being an experienced brain surgeon, Dr. Jandial also does a lot of cutting edge lab research too. What does this mean for us?
This book gives, as the subtitle promises, “practical strategies for peak health and performance”—with a brain-centric bias, of course.
From diet and nootropic supplements, to exercise and brain-training, we get a good science-based view of which ones actually work, and which don’t. The style is also very readable; Dr. Jandial is a great educator, presenting genuine scientific content with very accessible language.
Bottom line: if you’d indeed like to look after your most important organ optimally, this book gives a lot of key pointers, without unnecessary fluff.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Quick Healthy Recipe Ideas
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
“It was superb !! Just loved that healthy recipe !!! I would love to see one of those every day, if possible !! Keep up the fabulous work !!! ”
We’re glad you enjoyed! We can’t promise a recipe every day, but here’s one just for you:
Share This Post
-
The Silent Struggle – by L. William Ross-Child, MLC
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The vast majority of literature out there about ADHD is about children. And fair enough, there are enough popular misunderstandings of ADHD in children so it’s good those works exist… but what about adults?
Adults face different challenges than children, and have different responsibilities. People have different expectations. And even if you say you have ADHD… If you’re not behaving like a squirrel, they will often not accept this, much less understand it, because half the actual symptoms are not what most people think they are.
Ross-Child first lays out the neurobiological underpinnings of ADHD. This is a good place to start, because the physiology of it explains a lot of the other parts of it that can otherwise seem quite mystifying.
Thereafter, he looks one-by-one at the various cognitive and behavioral aspects of ADHD in adults, which will surely help the reader to better understand themself (or perhaps a loved one).
The next part of the book is given over to an exploration of ADHD and the differences it can make in the workplace, relationships (incl. ADHD and sex), as well as parenting, and how these things can all be navigated better by all concerned.
The style throughout is light and very readable, peppered with science made comprehensible. If there’s any flaw, it’s that there are only two pages of references in the bibliography—we’d have liked to have seen more.
All in all though, a really useful guide if you or a loved one has ADHD and you’d like strategies for working with (or around) this condition in a world not made to be kind to such.
Order your copy of “The Silent Struggle: Taking Charge of ADHD in Adults” from Amazon today!
Share This Post
-
Eat To Avoid (Or Beat) PCOS
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Polycystic ovary syndrome, PCOS, affects very many people; around 1 in 5 women. It can show up unexpectedly, and usually the first-identified sign is irregular vaginal bleeding. We say “vaginal” rather than “menstrual” as it’s not technically menses, although it’ll look (and can feel) the same.
Like many “affects mostly women” conditions, science’s general position is “we don’t know what causes it or how to cure it”.
Quick book recommendation before we continue:
Unwell Women: Misdiagnosis and Myth in a Man-Made World – by Dr. Elinor Cleghorn
…is a top-tier book about medical misogyny. We’d say more here, but well, you can read our review there 🙂
What doesn’t work
Since PCOS is characterized by excessive androgen production, it is reasonable to expect that foods containing phytoestrogens (such as soy) may help. They won’t. The human body can’t use those as estrogen, and in fact, consuming unusually large quantities of phytoestrogens can actually get in the way of your own (or bioidentical) estrogen, by competing for the same receptors but not really doing the job.
But, you won’t get that problem from moderate consumption of soy; the warning is more for those tempted to self-medicate with megadoses, or are opting for dubious supplements such as Pueraria mirifica ← will have to do a research review on that one of these days, but suffice it to say meanwhile, it has some serious drawbacks
See also: What Does “Balance Your Hormones” Even Mean?
What can work
There are some supplement-based approaches that actually can help, and those are the ones that rather than trying to manufacture estrogen out of thin air, work to reduce testosterone and/or reduce the conversion of free testosterone to its more potent form, dihydrogen testosterone (DHT); here are two examples:
- Licorice, Digestion, & Hormones
- One Man’s Saw Palmetto Is Another Woman’s Serenoa Repens ← this one has the most evidence of the two
What will work
…or at least, barring additional confounding factors, what the evidence strongly supports working. Here’s where we get into diet properly, and there are three main dietary approaches:
Low-GI diet: focus on high-fiber, low-carb foods (e.g. whole grains, legumes, berries, leafy greens). Eating this way results in improved insulin sensitivity, lower fasting insulin, cholesterol, triglycerides, waist circumference, and (for women) yes, lower testosterone levels.
See: What Do The Different Kinds Of Fiber Do? 30 Foods That Rank Highest
High antioxidant diet: focus on foods rich in antioxidants (e.g. vitamin A, α-tocopherol specifically, vitamins C and D, and polyphenols) as these lower PCOS incidence.
See: 21 Most Beneficial Polyphenols & What Foods Have Them
Ketogenic diet: focus on high-fat, very low-carb foods (e.g. fatty fish, dairy, leafy greens). This significantly reduces androgen levels, improves insulin sensitivity, and regulates hormones. But… It’s recommended for short-term use only due to its negative health impacts from poor (i.e. narrow) nutritional coverage:
See: Ketogenic Diet: Burning Fat, Or Burning Out?
It is also reasonable to supplement, for example:
❝Omega-3 fatty acids and vitamin D have powerful anti-inflammatory and antioxidant properties that significantly improve insulin sensitivity and reduce androgen levels in metabolic syndromes like PCOS. A higher intake of omega-3 and vitamin E also alleviates mental health parameters and gene expression of PPAR-γ, IL-8, and TNF-α in women with PCOS.
Dietary supplements, such as antioxidants like N-acetylcysteine (NAC), vitamin D, inositol, and omega-3 fatty acids, and mineral supplements (zinc, magnesium selenium, and chromium) help in reducing insulin resistance. These supplements also enhance ovulatory function and decrease inflammation in PCOS patients.
Omega-3 fatty acid supplements improve biochemical parameters LH, LH/FSH, lipid profiles, and adiponectin levels and regularize the menstrual cycle in women with PCOS. A recent RCT also indicated that probiotic/symbiotic supplementation significantly improves triglyceride, insulin, and HDL levels in women with PCOS.❞
Source: The Role of Lifestyle Interventions in PCOS Management: A Systematic Review
Want to know more?
You might like this book that we reviewed a little while back:
PCOS Repair Protocol – by Tamika Woods
Take care!
Share This Post
Related Posts
-
The Foot Book – by Dr. Todd Brennan & Dr. Leslie Johnston
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book really is what the subtitle claims it to be: “everything you need to know to take care of your feet”.
Arthritis, bunions, corns, diabetes, eczema, fungus, gout, heel pain, ingrown toenails, joint issues, and that’s just one item for each of the first 10 letters of the alphabet.
There’s a lot in here; the point is that it covers everything from the “serious” to the “cosmetic”, so whether you want to be a foot model for an expensive perfume company or just want to walk without pain, the answer is probably in here.
The goal of this book is to be comprehensive like that, and also with an open agenda to educate the world as to what it actually is that podiatrists do (hint: their years of medical school and further training in residency are not just so that they can trim toenails nicely).
The style is very light and readable, as one might expect from a pair of doctors with many years of experience of explaining exactly these things to patients every day.
Bottom line: if you have feet and would like them to be/remain in good condition, this book is an invaluable resource!
Click here to check out The Foot Book, and take good care of yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Practical Optimism – by Dr. Sue Varma
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about how to get your brain onto a more positive track (without toxic positivity), but there’s a lot more to be said than we can fit into an article, so here’s a whole book packed full with usable advice.
The subtitle claims “the art, science, and practice of…”, but mostly it’s the science of. If there’s art to be found here, then this reviewer missed it, and as for the practice of, well, that’s down to the reader, of course.
However, it is easy to use the contents of this book to translate science into practice without difficulty.
If you’re a fan of acronyms, initialisms, and other mnemonics (such as the rhyming “Name, Claim, Tame, and Reframe”), then you’ll love this book as they come thick and fast throughout, and they contribute to the overall ease of application of the ideas within.
The writing style is conversational but with enough clinical content that one never forgets who is speaking—not in the egotistical way that some authors do, but rather, just, she has a lot of professional experience to share and it shows.
Bottom line: if you’d like to be more optimistic without delving into the delusional, this book can really help a lot with that (in measurable ways, no less!).
Click here to check out Practical Optimism, and brighten up your life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cupping: How It Works (And How It Doesn’t)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Good Health By The Cup?
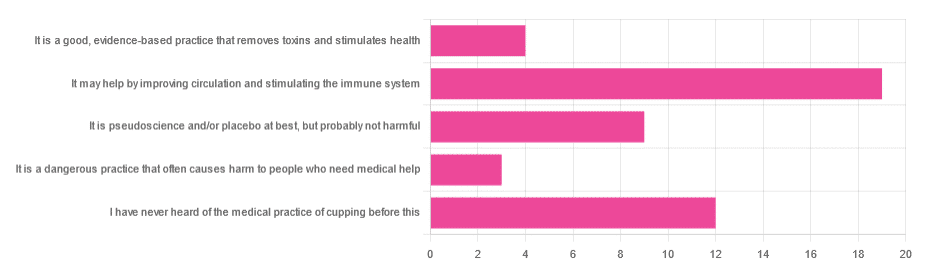
In Tuesday’s newsletter, we asked you for your opinion of cupping (the medical practice), and got the above-depicted, below-described, set of responses:
- About 40% said “It may help by improving circulation and stimulating the immune system”
- About 26% said “I have never heard of the medical practice of cupping before this”
- About 19% said “It is pseudoscience and/or placebo at best, but probably not harmful
- About 9% said “It is a good, evidence-based practice that removes toxins and stimulates health”
- About 6% said “It is a dangerous practice that often causes harm to people who need medical help”
So what does the science say?
First, a quick note for those unfamiliar with cupping: it is the practice of placing a warmed cup on the skin (open side of the cup against the skin). As the warm air inside cools, it reduces the interior air pressure, which means the cup is now (quite literally) a suction cup. This pulls the skin up into the cup a little. The end result is visually, and physiologically, the same process as what happens if someone places the nozzle of a vacuum cleaner against their skin. For that matter, there are alternative versions that simply use a pump-based suction system, instead of heated cups—but the heated cups are most traditional and seem to be most popular. See also:
National Center for Complementary and Integrative Health | Cupping
It is a dangerous practice that often causes harm to people who need medical help: True or False?
False, for any practical purposes.
- Directly, it can (and usually does) cause minor superficial harm, much like many medical treatments, wherein the benefits are considered to outweigh the harm, justifying the treatment. In the case of cupping, the minor harm is usually a little bruising, but there are other risks; see the link we gave just above.
- Indirectly, it could cause harm by emboldening a person to neglect a more impactful treatment for their ailment.
But, there’s nothing for cupping akin to the “the most common cause of death is when someone gets a vertebral artery fatally severed” of chiropractic, for example.
It is a good, evidence-based practice that removes toxins and stimulates health: True or False?
True and False in different parts. This one’s on us; we included four claims in one short line. But let’s look at them individually:
- Is it good? Well, those who like it, like it. It legitimately has some mild health benefits, and its potential for harm is quite small. We’d call this a modest good, but good nonetheless.
- Is it evidence-based? Somewhat, albeit weakly; there are some papers supporting its modest health claims, although the research is mostly only published in journals of alternative medicine, and any we found were in journals that have been described by scientists as pseudoscientific.
- Does it remove toxins? Not directly, at least. There is also a version that involves making a small hole in the skin before applying the cup, the better to draw out the toxins (called “wet cupping”). This might seem a little medieval, but this is because it is from early medieval times (wet cupping’s first recorded use being in the early 7th century). However, the body’s response to being poked, pierced, sucked, etc is to produce antibodies, and they will do their best to remove toxins. So, indirectly, there’s an argument.
- Does it stimulate health? Yes! We’ll come to that shortly. But first…
It is pseudoscience and/or placebo at best, but probably not harmful: True or False?
True in that its traditionally-proposed mechanism of action is a pseudoscience and placebo almost certainly plays a strong part, and also in that it’s generally not harmful.
On it being a pseudoscience: we’ve talked about this before, but it bears repeating; just because something’s proposed mechanism of action is pseudoscience, doesn’t necessarily mean it doesn’t work by some other mechanism of action. If you tell a small child that “eating the rainbow” will improve their health, and they believe this is some sort of magical rainbow power imbuing them with health, then the mechanism of action that they believe in is a pseudoscience, but eating a variety of colorful fruit and vegetables will still be healthy.
In the case of cupping, its proposed mechanism of action has to do withbalancing qi, yin and yang, etc (for which scientific evidence does not exist), in combination with acupuncture lore (for which some limited weak scientific evidence exists). On balancing qi, yin and yang etc, this is a lot like Europe’s historically popular humorism, which was based on the idea of balancing the four humors (blood, yellow bile, black bile, phlegm). Needless to say, humorism was not only a pseudoscience, but also eventually actively disproved with the advent of germ theory and modern medicine. Cupping therapy is not more scientifically based than humorism.
On the placebo side of things, there probably is a little more to it than that; much like with acupuncture, a lot of it may be a combination of placebo and using counter-irritation, a nerve-tricking method to use pain to reduce pain (much like pressing with one’s nail next to an insect bite).
Here’s one of the few studies we found that’s in what looks, at a glance, to be a reputable journal:
Cupping therapy and chronic back pain: systematic review and meta-analysis
It may help by improving circulation and stimulating the immune system: True or False?
True! It will improve local circulation by forcing blood into the area, and stimulate the immune system by giving it a perceived threat to fight.
Again, this can be achieved by many other means; acupuncture (or just “dry needling”, which is similar but without the traditional lore), a cold shower, and/or exercise (and for that matter, sex—which combines exercise, physiological arousal, and usually also foreign bodies to respond to) are all options that can improve circulation and stimulate the immune system.
You can read more about using some of these sorts of tricks for improving health in very well-evidenced, robustly scientific ways here:
The Stress Prescription (Against Aging!)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: