Is thunderstorm asthma becoming more common?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When spring arrives, so do warnings about thunderstorm asthma. But a decade ago, most of us hadn’t heard of it.
So where did thunderstorm asthma come from? Is it a new phenomenon?
In 2016, the world’s most catastrophic thunderstorm asthma event took Melbourne by surprise. An increase in warnings and monitoring is partly a response to this.
But there are also signs climate change may be exacerbating the likelihood of thunderstorm asthma, with more extreme weather, extended pollen seasons and a rise in Australians reporting hay fever.
A landmark catastrophe
The first time many Australians heard of thunderstorm asthma was in November 2016, when a major event rocked Melbourne.
During a late night storm, an estimated 10,000 people were rushed to hospitals with severe asthma attacks. With thousands of calls on emergency lines, ambulances and emergency departments were unprepared to handle the rapid increase in people needing urgent medical care. Tragically, ten of those people died.
This was the most catastrophic thunderstorm asthma event in recorded history and the first time deaths have ever occurred anywhere in the world.
In response, the Victorian Department of Health implemented initiatives, including public awareness campaigns and improvements to health and emergency services, to be ready for future thunderstorm asthma events.
A network of pollen monitoring stations was also set up across the state to gather data that helps to predict future events.
A problem for decades
While this event was unexpected, it wasn’t the first time we’d had thunderstorm asthma in Australia – we’ve actually known about it for decades.
Melbourne reported its first instance of thunderstorm asthma back in 1984, only a year after this phenomenon was first discovered in Birmingham in the United Kingdom.
Thunderstorm asthma has since been reported in other parts of Australia, including Canberra and New South Wales. But it is still most common in Melbourne. Compared to any other city (or country) the gap is significant: over a quarter of all known events worldwide have occurred in Melbourne.
Why Melbourne?
Melbourne’s location makes it a hotspot for these kinds of events. Winds coming from the north of Melbourne tend to be dry and hot as they come from deserts in the centre of Australia, while winds from the south are cooler as they come from the ocean.
When hot and cool air mix above Melbourne, it creates the perfect conditions for thunderstorms to form.
Northern winds also blow a lot of pollen from farmlands into the city, in particular grass pollen. This is not only the most common cause of seasonal hay fever in Melbourne but also a major trigger of thunderstorm asthma.
Why grass pollen?
There’s a particular reason grass pollen is the main culprit behind thunderstorm asthma in Australia. During storms there is a lot of moisture in the air. Grass pollen will absorb this moisture, making it swell up like a water balloon.
If pollen absorbs too much water whilst airborne, it can burst or “rupture,” releasing hundreds of microscopic particles into the air that can be swept by powerful winds.
Normally, when you breathe in pollen it gets stuck in your upper airway – for example, your nose and throat. This is what causes typical hay fever symptoms such as sneezing or runny nose.
But the microscopic particles released from ruptured grass pollen are much smaller and don’t get stuck as easily in the upper airway. Instead, they can travel deep into your airways until they reach your lungs. This may trigger more severe symptoms, such as wheezing or difficulty breathing, even in people with no prior history of asthma.
So who is at risk?
You might think asthma is the biggest risk factor for thunderstorm asthma. In fact, the biggest risk factor is hay fever.
Up to 99% of patients who went to the emergency department during the Melbourne 2016 event had hay fever, while a majority (60%) had no prior diagnosis of asthma.
Every single person hospitalised was allergic to at least one type of grass pollen. All had a sensitivity to ryegrass.
Is thunderstorm asthma becoming more common?
Thunderstorm asthma events are rare, with just 26 events officially recorded worldwide.
However there is evidence these events could become more frequent and severe in coming years, due to climate change. Higher temperatures and pollution could be making plants produce more pollen and pollen seasons last much longer.
Extreme weather events, including thunderstorms, are also expected to become more common and severe.
In addition, there are signs rates that hay fever may be increasing. The number of Australians reporting allergy symptoms have risen from 15% in 2008 to 24% in 2022. Similar trends in other countries has been linked to climate change.
How can I prepare?
Here are three ways you can reduce your risk of thunderstorm asthma:
- stock up on allergy medication and set up an asthma action plan with your GP
- check daily pollen forecasts for the estimated pollen level and risk of a thunderstorm asthma event in your local area
- on days with high pollen or a high risk of thunderstorm asthma, spend less time outside or wear a surgical face mask to reduce your symptoms.
Kira Morgan Hughes, PhD Candidate in Allergy and Asthma, School of Life and Environmental Sciences, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Mythbusting Cookware Materials
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
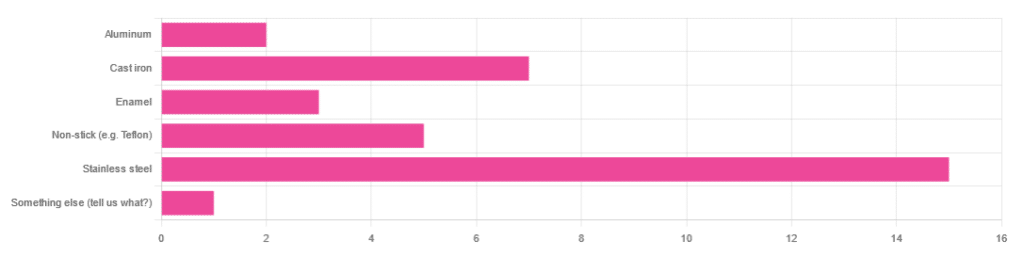
In Wednesday’s newsletter, we asked you what kind of cookware you mostly use, and got the above-depicted, below-described, set of responses:
- About 45% said stainless steel
- About 21% said cast iron
- About 15% said non-stick (e.g. Teflon)
- About 9% said enamel
- About 6% said aluminum
- And 1 person selected “something else”, but then commented to the contrary, writing “I use all of the above”
So, what does the science say about these options?
Stainless steel cookware is safe: True or False?
True! Assuming good quality and normal use, anyway. There really isn’t a lot to say about this, because it’s very unexciting. So long as it is what it is labelled as: there’s nothing coating it, nothing comes out of it unless you go to extremes*, and it’s easy to clean.
*If you cook for long durations at very high temperatures, it can leach nickel and chromium into food. What this means in practical terms: if you are using stainless steel to do deep-frying, then maybe stop that, and also consider going easy on deep-frying in general anyway, because obviously deep-frying is unhealthy for other reasons.
Per normal use, however: pretty much the only way (good quality) stainless steel cookware will harm you is if you touch it while it’s hot, or if it falls off a shelf onto your head.
That said, do watch out for cheap stainless steel cookware that can contain a lot of impurities, including heavy metals. Since you probably don’t have a mass spectrometer and/or chemistry lab at home to check for those impurities, your best guard here is simply to buy from a reputable brand with credible certifications.
Ceramic cookware is safe: True or False?
True… Most of the time! Ceramic pans usually have metal parts and a ceramic cooking surface coated with a very thin layer of silicon. Those metal parts will be as safe as the metals used, so if that’s stainless steel, you’re just as safe as the above. As for the silicon, it is famously inert and body-safe (which is why it’s used in body implants).
However: ceramic cookware that doesn’t have an obvious metal part and is marketed as being pure ceramic, will generally be sealed with some kind of glaze that can leach heavy metals contaminants into the food; here’s an example:
Lead toxicity from glazed ceramic cookware
Copper cookware is safe: True or False?
False! This is one we forgot to mention in the poll, as one doesn’t see a lot of it nowadays. The copper from copper pans can leach into food. Now, of course copper is an important mineral that we must get from our diet, but the amount of copper that that can leach into food from copper pans is far too much, and can induce copper toxicity.
In addition, copper cookware has been found to be, on average, highly contaminated with lead:
Non-stick cookware contaminates the food with microplastics: True or False?
True! If we were to discuss all the common non-stick contaminants here, this email would no longer fit (there’s a size limit before it gets clipped by most email services).
Suffice it to say: the non-stick coating, polytetrafluoroethylene, is itself a PFAS, that is to say, part of the category of chemicals considered environmental pollutants, and associated with a long list of health issues in humans (wherein the level of PFAS in our bloodstream is associated with higher incidence of many illnesses):
You may have noticed, of course, that the “non-stick” coating doesn’t stick very well to the pan, either, and will tend to come off over time, even if used carefully.
Also, any kind of wet cooking (e.g. saucepans, skillets, rice cooker inserts) will leach PFAS into the food. In contrast, a non-stick baking tray lined with baking paper (thus: a barrier between the tray and your food) is really not such an issue.
We wrote about PFAS before, so if you’d like a more readable pop-science article than the scientific paper above, then check out:
PFAS Exposure & Cancer: The Numbers Are High
Aluminum cookware contaminates the food with aluminum: True or False?
True! But not usually in sufficient quantities to induce aluminum toxicity, unless you are aluminum pans Georg who eats half a gram of aluminum per day, who is a statistical outlier and should not be counted.
That’s a silly example, but an actual number; the dose required for aluminum toxicity in blood is 100mg/L, and you have about 5 liters of blood.
Unless you are on kidney dialysis (because 95% of aluminum is excreted by the kidneys, and kidney dialysis solution can itself contain aluminum), you will excrete aluminum a lot faster than you can possibly absorb it from cookware. On the other hand, you can get too much of it from it being a permitted additive in foods and medications, for example if you are taking antacids they often have a lot of aluminum oxide in them—but that is outside the scope of today’s article.
However, aluminum may not be the real problem in aluminum pans:
❝In addition, aluminum (3.2 ± 0.25 to 4.64 ± 0.20 g/kg) and copper cookware (2.90 ± 0.12 g/kg) were highly contaminated with lead.
The time and pH-dependent study revealed that leaching of metals (Al, Pb, Ni, Cr, Cd, Cu, and Fe, etc.) into food was predominantly from anodized and non-anodized aluminum cookware.
More metal leaching was observed from new aluminum cookware compared to old. Acidic food was found to cause more metals to leach during cooking.❞
~ the same paper we cited when talking about copper
Cast iron cookware contaminates the food with iron: True or False?
True, but unlike with the other metals discussed, this is purely a positive, and indeed, it’s even recommended as a good way to fortify one’s diet with iron:
The only notable counterpoint we could find for this is if you have hemochromatosis, a disorder in which the body is too good at absorbing iron and holding onto it.
Thinking of getting some new cookware?
Here are some example products of high-quality safe materials on Amazon, but of course feel free to shop around:
Stainless Steel | Ceramic* | Cast Iron
*it says “non-stick” in the description, but don’t worry, it’s ceramic, not Teflon etc, and is safe
Bonus: rice cooker with stainless steel inner pot
Take care!
Share This Post
-
How To Reduce Chronic Stress
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sunday Stress-Buster
First, an important distinction:
- Acute stress (for example, when stepping out of your comfort zone, engaging in competition, or otherwise focusing on something that requires your full attention for best performance) is generally a good thing. It helps you do you your best. It’s sometimes been called “eustress”, “good stress”.
- Chronic stress (for example, when snowed under at work and you do not love it, when dealing with a serious illness, and/or faced with financial problems) is unequivocally a bad thing. Our body is simply not made to handle that much cortisol (the stress hormone) all the time.
Know the dangers of too much cortisol
We covered this as a main feature last month: Lower Your Cortisol! (Here’s Why & How)
…but it bears mentioning again and for those who’ve joined us since then:
A little spike of cortisol now and again can be helpful. Having it spiking all the time, or even a perpetual background low-to-moderate level, can be ruinous to the health in so many ways.
The good news is, the physiological impact of stress on the body (which ranges from face-and-stomach fat deposits, to rapid aging), can be reversed—even the biological aging!
Read: Biological age is increased by stress and restored upon recovery ← this study is so hot-of-the-press that it was published literally two days ago
Focus on what you can control
A lot of things that cause you stress may be outside of your control. Focus on what is within your control. Oftentimes, we are so preoccupied with the stress, that we employ coping strategies that don’t actually deal with the problem.
That’s a maladaptive response to an evolutionary quirk—our bodies haven’t caught up with modern life, and on an evolutionary scale, are still priming us to deal with sabre-toothed tigers, not financial disputes, for example.
But, how to deal with the body’s “wrong” response?
First, deal with the tiger. There isn’t one, but your body doesn’t know that. Do some vigorous exercise, or if that’s not your thing, tense up your muscles strongly for a few seconds and then relax them, doing each part of your body. This is called progressive relaxation, and how it works is basically tricking your body into thinking you successfully fled the tiger, or fought the tiger and won.
Next, examine what the actual problem is, that’s causing you stress. You’re probably heavily emotionally attached to the problem, or else it wouldn’t be stressing you. So, imagine what advice you would give to help a friend deal with the same problem, and then do that.
Better yet: enlist an actual friend (or partner, family member, etc) to help you. We are evolved to live in a community, engaged in mutual support. That’s how we do well; that’s how we thrive best.
By dealing with the problem—or sometimes even just having support and/or something like a plan—your stress will evaporate soon enough.
The power of “…and then what?”
Sometimes, things are entirely out of your control. Sometimes, bad things are entirely possible; perhaps even probable. Sometimes, they’re so bad, that it’s difficult to avoid stressing about the possible outcomes.
If something seems entirely out of your control and/or inevitable, ask yourself:
“…and then what?”
Writer’s storytime: when I was a teenager, sometimes I would go out without a coat, and my mother would ask, pointedly, “But what will you do if it rains?!”
I’d reply “I’ll get wet, of course”
This attitude can go just the same for much more serious outcomes, up to and including death.
So when you find yourself stressing about some possible bad outcome, ask yourself, “…and then what?”.
- What if this is cancer? Well, it might be. And then what? You might seek cancer treatment.
- What if I can’t get treatment, or it doesn’t work? Well, you might die. And then what?
In Dialectic Behavior Therapy (DBT), this is called “radical acceptance” and acknowledges bad possible/probable/known outcomes, allows one to explore the feelings, and come up with a plan for managing the situation, or even just coming to terms with the fact that sometimes, suffering is inevitable and is part of the human condition.
It’ll still be bad—but you won’t have added extra suffering in the form of stress.
Breathe.
Don’t underestimate the power of relaxed deep breathing to calm the rest of your body, including your brain.
Also: we’ve shared this before, a few months ago, but this 8 minute soundscape was developed by sound technicians working with a team of psychologists and neurologists. It’s been clinically tested, and found to have a much more relaxing effect(in objective measures of lowering heart rate and lowering cortisol levels, as well as in subjective self-reports) than merely “relaxing music”.
Try it and see for yourself:
! Share This Post
-
Tempeh vs Tofu – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing tempeh to tofu, we picked the tempeh.
Why?
Per 100g, tempeh has about 1.5x as many calories, about 2x as much protein, about 3x as much fiber, and about 4x the carbohydrates.
Which latter sounds like a lot, but really, the amounts here are small—tempeh is under 12% carbohydrates, and most of that is treated by the body as fiber (e.g. it’s a resistant starch).
Both have no sugar, and both have more or less the same (tiny) amount of fat.
Micronutrients, you ask? As they’re both made from soybeans, the micronutrient profiles are similar, but exact amounts will depend on the method used, so by all means check labels if comparing products in store. By and large, there’s usually not much difference, though.
You can see sample stats here:
In summary
Both are great, and/but tempeh is the more nutrient-dense of the two.
Therefore, tempeh is the healthier option, unless you are on a very strictly calorie-controlled diet, in which case, tofu will give you more quantity per calorie.
Enjoy!
Share This Post
Related Posts
-
The Insomnia Breakthrough – by Katherine Coleman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, a massage therapist, knows plenty about relaxation. But how to put that to use when it comes to getting good quality sleep?
She takes a holistic approach, and yes, does start by covering all the things you’d expect to find in any guide to better sleep (aim for regular schedule, have darkness when you sleep, cool room, clean sheets, no alcohol or caffeine before bed, etc).
What she offers in particular beyond that, is the integration of calming routines, building in mindfulness for sleep (when very often people will go for the opposite!), and small cumulative lifestyle adjustments that are conducive to getting a better night’s rest every night.
The style is very light pop-science (as one might expect from someone who is not, in fact, a scientist), and while we do get a bibliography at the back, it’s a meagre 4 pages. Nevertheless, there’s a lot of interdisciplinary knowledge here, explained well.
Bottom line: if improving your sleep is something you’d like to do, this book can almost certainly get you on the right track.
Click here to check out The Insomnia Breakthrough, and don’t stay up too late reading it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why You Don’t Need 8 Glasses Of Water Per Day
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The idea that you need to drink eight glasses of water daily is a myth. For most people most of the time, this practice will not make your skin brighter, improve mental clarity, or boost energy levels. All that will happen as a result of drinking beyond your thirst, is that you’ll pee more.
A self-regulating system
Our kidneys regulate hydration by monitoring blood volume and salt levels. When blood becomes slightly saltier or its volume drops, such as through sweating, the kidneys absorb more water into the bloodstream. If needed, the body triggers thirst signals to encourage fluid intake.
In most cases, you can rely on your body’s natural thirst cues to manage hydration. Thirst is a reliable indicator of when you need to drink water, making constant monitoring of water intake unnecessary for most people.
There are some exceptions, though! Some people, such as those with kidney stones, especially older adults, or those with specific medical considerations and resultant advice from your doctor, may need to pay closer attention to their water intake.
Nor does hydration have to be a matter of “drinking water”: many foods and drinks, such as fruit, coffee, soups, etc, contribute to your daily water intake and (because the body processes it more slowly) are often more hydrating than plain water (which can just pass straight through if you take more than a certain amount at once). If you listen to your body’s thirst signals, there’s no need to rigidly count eight glasses of water each day.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Hydration Mythbusting ← this also covers why urine color is not as good a guide as your thirst
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
7 Essential Devices For Hand Arthritis: Regain Control of Your Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Diana Girnita is a double board-certified physician in rheumatology and internal medicine. With a PhD in immunology (on top of her MD), and training at Harvard and top universities, she founded Rheumatologist OnCall, offering integrative medicine to broaden rheumatology access. Here’s what she has to say about things that make life easier:
Get your hands on these…
The seven devices that Dr. Girnita recommends are:
- Hand grip strengthener: helps build grip strength with a spring-loaded mechanism. Regular use can improve strength and reduce pain.
- Finger exerciser: different device; similar principle: it strengthens hand and finger muscles using resistance, enhancing hand function.
- Moisturizing paraffin bath: a heated paraffin wax bath that soothes hands, providing heat therapy and moisturizing the skin.
- Weighted silverware: weighted utensils (knives, forks, spoons) make gripping easier and provide stability for eating.
- Foam tubing grips: foam covers to make kitchen tools, toothbrushes, and hairbrushes easier to grip.
- Electric can-opener: reduces strain in opening cans, making meal preparation more accessible.
- Compression gloves: provide gentle compression to reduce swelling and pain, improving hand flexibility and circulation.
- Door knob cover grips: make it easier to turn doorknobs by providing a larger surface to grip.
- Wider-grip pens: ergonomically designed pens with a larger diameter and softer grip reduce hand strain while writing.
This writer, who does not have arthritis but also does not have anything like the grip strength she used to, also recommends a jar opener like this one.
As a bonus, if you spend a lot of time writing at a computer, an ergonomic split keyboard like this one goes a long way to avoiding carpal tunnel syndrome, and logically must be better for arthritis than a regular keyboard; another excellent thing to have (that again this writer uses and swears by) is an ergonomic vertical mouse like this one (aligns the wrist bones correctly; the “normal” horizontal version is woeful for the carpal bones). These things are both also excellent to help avoid worsening peripheral neuropathy (something that troubles this writer’s wrists if she’s not careful, due to old injuries there).
For more on the seven things otherwise listed above, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Avoiding/Managing Rheumatoid Arthritis
- Avoiding/Managing Osteoarthritis
- Managing Chronic Pain (Realistically!)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: