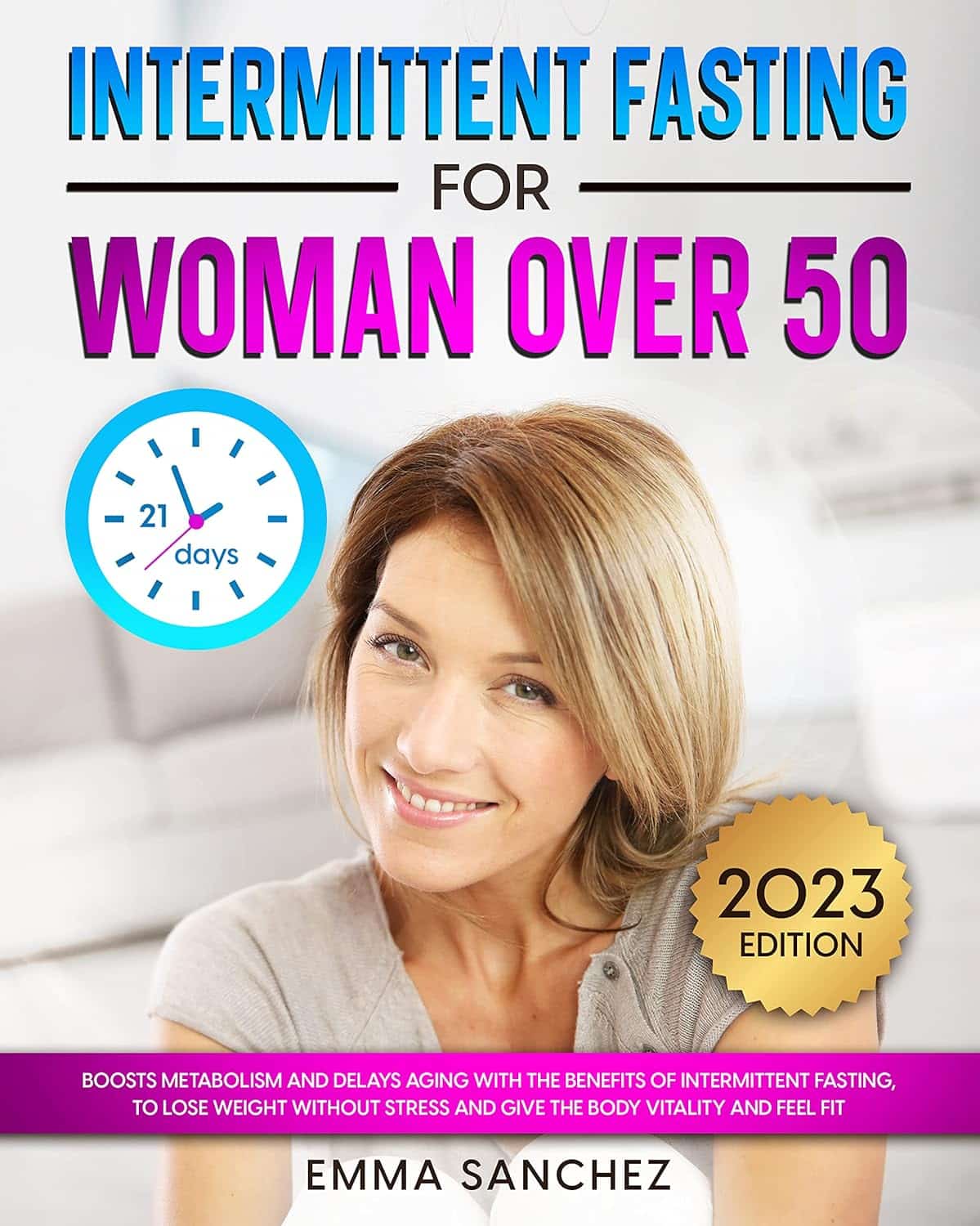
Intermittent Fasting for Women Over 50 – by Emma Sanchez
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Intermittent fasting is promoted as a very healthful (evidence-based!) way to trim the fat and slow aging, along with other health benefits. But, physiologically and especially metabolically, the average woman is quite different from the average man! And most resources are aimed at men. So, what’s the difference?
Emma Sanchez gives an overview not just of intermittent fasting, but also, how it goes with specifically female physiology. From hormonal cycles, to different body composition and fat distribution, to how we simply retain energy better—which can be a mixed blessing!
We’re given advice about how to optimize all those things and more.
She also covers issues that many writers on the topic of intermittent fasting will tend to shy away from, such as:
- mood swings
- risk of eating disorder
- impact on cognitive thinking
…and she does this evenly and fairly, making the case for intermittent fasting while acknowledging potential pitfalls that need to be recognized in order to be managed.
Lastly, the “over 50” thing. This is covered in detail quite late in the book, but there are a lot of changes that occur (beyond the obvious!), and once again, Sanchez has tips and tricks for holding back the clock where possible, and working with it rather than against it, when appropriate.
All in all, a great book for any woman over 50, or really also for women under 50, especially if that particular milestone is on the horizon.
Get your copy of Intermittent Fasting for Women over 50 from Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Obesity Code – by Dr. Jason Fung
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Firstly, if you have already read Dr. Fung’s other book, The Diabetes Code, which we reviewed a little while ago, you can probably skip this one. It has mostly the same information, presented with a different focus.
While The Diabetes Code assumes you are diabetic, or prediabetic, or concerned about avoiding/reversing those conditions, The Obesity Code assumes you are obese, or heading in that direction, or otherwise are concerned about avoiding/reversing obesity.
What it’s not, though, is a weight loss book. Will it help if you want to lose weight? Yes, absolutely. But there is no talk here of weight loss goals, nor any motivational coaching, nor week-by-week plans, etc.
Instead, it’s more an informative textbook. With exactly the sort of philosophy we like here at 10almonds: putting information into people’s hands, so everyone can make the best decisions for themselves, rather than blindly following someone else’s program.
Dr. Fung explains why various dieting approaches don’t work, and how we can work around such things as our genetics, as well as most external factors except for poverty. He also talks us through how to change our body’s insulin response, and get our body working more like a lean machine and less like a larder for hard times.
Bottom line: this is a no-frills explanation of why your body does what it does when it comes to fat storage, and how to make it behave differently about that.
Share This Post
-
Seasonal Affective Disorder (Beyond Sunlight!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For those of us in the Northern Hemisphere, the time of increasing darkness is upon us again. Depending on our latitude, the sun barely rises before it skitters off again. And depending on other factors of our geography, we might not get much sun during that time (writer’s example: the ancient bog from which I write has been surrounded by fog for two weeks now).
So, what to do about it?
Firstly, we can make the most of whatever sun we do get (especially in the morning, if possible), and we can of course make some use of artificial sunlight. To save doubling up, we’ll link to what we previously wrote about optimizing both of those things:
‘Tis To Season To Be SAD-Savvy
More ways to get serotonin
Sunlight, of course, triggers our bodies to make serotonin, and hence we often make less of it during winter. But, there are other ways to get serotonin too, and one of the best ways is spending time in nature. Yes, even if the weather is gloomy, provided there are still visible green things and you are seeing them, it will promote serotonin production.
Of course, it may not be the season for picnics, but a morning walk through a local park or other green space is ideal.
On which note, gardening remains a good activity. Not a lot of people do so much gardening after a certain point in the year, but in one way, it’s more important than ever to get some soil under your fingernails:
There are bacteria in soil (specifically: Mycobacterium vaccae) that work similarly to antidepressants.
When something is described as having an effect similar to antidepressants, it’s usually hyperbole. In this case, it’s medicine, and literally works directly on the serotonergic system (as do many, but not all, antidepressants).
See also: Antidepressants: Personalization Is Key!
While many antidepressants are selective serotonin uptake inhibitors (i.e., they slow the rate at which your brain loses serotonin), Mycobacterium vaccae increases the rate at which you produce serotonin. So, you feel happier, more relaxed, while also feeling more energized.
^this one’s a mouse study, but we’re including it because it covers exactly how it works in the brain, which is something that the ethics board wouldn’t let them do on humans, due to the need for slicing the brains up for examination.
As to how to benefit: touching soil will get you “infected” by the bacteria, yes, even if you wash your hands later. Growing food in the soil and eating the good (including if you wash and cook it) is even better.
Boost the other “happiness chemicals”
Serotonin is just one “happiness hormone”, other feel-good neurotransmitters that are just as important include dopamine and oxytocin.
Dopamine is most associated with being the “reward chemical”, so it pays to do things that you find rewarding. If you’re stuck for ideas, engaging in small acts of kindness is a sure-fire way to get dopamine flowing and lift your own mood as well as theirs.
See also: 10 Ways To Naturally Boost Dopamine
Oxytocin, meanwhile is the “cuddle chemical”, and can be triggered even if you have nobody to cuddle*. If you do, by the way, make it at least 20–30 seconds, as that’s generally how long it takes to get oxytocin flowing.
*Vividly imagining it has much the same effect, since the brain can’t tell the difference. Alternatively, looking at pictures/videos (your choice) of small cute animals tends to work for most people also.
For more on these things, check out: Neurotransmitter Cheatsheet
Take care!
Share This Post
-
A Peek Behind The 10almonds Curtain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At 10almonds we give a lot of health information, so you may wonder: how much do we (the 10almonds team) put into practice? Is it even possible to do all these things? Do we have an 80:20 rule going on?
So, here’s what someone who thinks, reads, and writes about health all day, does for her health—and how it ties in with what you read here at 10almonds.
Hi, it’s me, a member of the 10almonds team and regular writer here, and I’m going to do the rest of this article in the first-person, since it’s using me as an example!
(PS: yes, the thumbnail is a digital impression of my appearance, though I would correct it that my hair is much longer, and my eyes are more gray; I must admit though it captured my smile, not to mention my collarbones-that-you-could-sit-on)
Dietary habits
Before we get to foods, let’s talk intermittent fasting. I practise 16:8 intermittent fasting… Approximately. That is to say, I’m mostly not religious about it, but I will generally breakfast around 12 noon, and have finished eating dinner before 8pm, with no food outside of those hours.
See also: Intermittent Fasting: What’s the truth?
Importantly, while I feel free to be a little flexible around start and finish times, I do very consciously decide “I am now fasting” and “I will now break the fast”.
Note my imperfection: it would be ideal to have the eating period earlier in the day, and have a bigger breakfast and small dinner. However, that doesn’t really work for me (leisurely evening meal is an important daily event in this household), so this is how I do it instead.
Foods!
It gets an exclamation mark because a thing about me is that I do love foods.
Breakfast: a typical breakfast for me these past months is a couple of ounces of mixed nuts with about 1oz of goji berries.
The mixed nuts are in equal proportions: almonds, walnuts, hazelnuts, cashews. Why those four? Simple, it’s because that’s what Aldi sells as “mixed nuts” and they are the cheapest nuts around, as well as containing absolute nutritional heavyweights almonds and walnuts in generous portions.
Often, but not always, I’ll have some dates with it, or dried apricots, or prunes.
I go through phases; sometimes I’ll enjoy overnight oats as my breakfast for a month or two at a time. I really just follow my gut in this regard.
See for example: Spiced Pear & Pecan Polyphenol Porridge
Lunch: I don’t really lunch per se, but between breakfast and dinner I’ll usually snack on a 3–5 organic carrots (I literally just cut the tops off and otherwise eat them like Bugs Bunny—peeling them would be extra work just to lose fiber). Note my imperfection: I don’t buy all of my vegetables organic, but I do for the ones where it makes the biggest difference.
If I’m feeling like it, I may lunch on a selection of herbs sabzi khordan style (see: Invigorating Sabzi Khordan), though I’m vegan so for simplicity I just skip the cheeses that are also traditional with that dish. On the other hand, for protein and fat I’ll usually add a cup of beans (usually black beans or kidney beans), seasoned with garlic and black pepper in an olive oil and balsamic vinegar dressing (that I make myself, so it’s just those ingredients). See also: Kidney Beans vs Black Beans – Which Is Healthier?
Dinner: this is my main sit-down meal of the day, and it’s enjoyed in a leisurely fashion (say, 40 minutes average with a normal distribution bell curve running between 20 and 60 minutes) with my son who lives with me. I mention all of this, because of the importance of relaxed mindful eating. In the instances of it being nearer the 20 minutes end, it’s not because of rushing, but rather because of a lighter meal some days.
See also: How To Get More Nutrition From The Same Food
Regular recurrences in the menu include:
I’ll often snack on something probiotic (e.g. kimchi) while I’m cooking.
See also: Make Friends With Your Gut! (You Can Thank Us Later)
In terms of what’s not in my diet: as mentioned, I’m vegan, so animal products are out. I don’t drink alcohol or use other recreational drugs, and I mostly drink decaffeinated coffee, but I’ll have a caffeinated one if I’m out somewhere. I’m not a puritan when it comes to sugar, but also, I simply don’t like it and I know well its health effects, so it doesn’t really form part of my diet except insofar as it’s in some ready-made condiments I may sometimes use (e.g. sriracha, teriyaki sauce). I’m also not a puritan when it comes to wheat, but it’s not something I consume daily. Usually on a weekly basis I’ll have a wholegrain pasta dish, and a dish with some kind of wholegrain flatbread.
See also:
Exercise!
First, some things that are lifestyle factors:
- I do not own a car, and I dislike riding in cars, buses, etc. So, I walk everywhere, unless it’s far enough that I must take the train, and even then I usually stand between carriages rather than sitting down.
- I have a standing desk setup, that hasn’t been lowered even once since I got it. I highly recommend it, as someone who spends a lot of time at my desk.
- You may imagine that I spend a lot of time reading; if it’s books (as opposed to scientific papers etc, which I read at my desk), then I’ll most of the time read them while perched like a gargoyle in a sitting squat (Slav squat, Asian squat, resting squat, deep squat, etc) on a balance ball. Yes, it is comfortable once you’re used to it!
About that latter, see also: The Most Anti Aging Exercise
In terms of “actual” exercise, I get 150–300 minutes “moderate exercise” per week, which is mostly composed of:
- Most days I walk into town to get groceries; it’s a 40-minute round trip on foot
- On days I don’t do that, even if I do walk to a more local shop, I spend at least 20 minutes on my treadmill.
See also: The Doctor Who Wants Us To Exercise Less, & Move More
Strength and mobility training, for me, comes mostly in what has been called “exercise snacking”, that is to say, I intersperse my working day with brief breaks to do Pilates exercises. I have theme days (lower body, core, upper body) and on average one rest day (from Pilates exercises) per week, though honestly, that’s usually more likely because of time constraints than anything else, because a deadline is looming.
See also: Four Habits That Drastically Improve Mobility
You may be wondering about HIIT: when I’m feeling extra-serious about it, I use my exercise bike for this, but I’ll be honest, I don’t love the bike, so on a daily basis, I’m much more likely to do HIIT by blasting out a hundred or so Hindu squats, resting, and repeating.
See also: How To Do HIIT (Without Wrecking Your Body)
Supplements
First I’ll mention, I do have HRT, of which the hormones I have are bioidentical estradiol gel in the morning, and a progesterone pessary in the evening. They may not be for everybody, but they’ve made a world of difference to me.
See also: HRT: A Tale Of Two Approaches
In terms of what one usually means when one says supplements, many I use intermittently (which is good in some cases, as otherwise the body may stop using them so well, or other problems can arise), but regular features include:
- Magnesium glycinate, malate, & citrate (See: Which Magnesium? (And: When?))
- Active vitamers of vitamins B9 and B12 (See: Which B Vitamins? It Makes A Difference!)
- Liposomal vitamin C (I actually get enough for general purposes in my diet, but as a vegan I don’t get dietary collagen, so this helps collagen synthesis)
- L-theanine (bedtime only) (See: L-Theanine: What’s The Tea?)
- Lion’s mane mushroom (See: What does lion’s mane mushroom actually do, anyway?)
- Quercetin (See: Fight Inflammation & Protect Your Brain, With Quercetin)
- Fisetin (weekends only) (See: Fisetin: The Anti-Aging Assassin)
Why weekends only for Fisetin? See: The Drug & Supplement Combo That Reverses Aging ← the supplement is fisetin, which outperforms quercetin in this role, and/but it only needs be taken for two days every two weeks, as a sort of “clearing out” of senescent cells. There is no need to take it every day, because if you just cleared out your senescent cells, then guess what, they’re not there now. Also, while sensescent cells are a major cause of aging, on a lower level they do have some anti-tumor effects, so it can be good to let some live a least for a while now and again. In short, cellular sensescence can help prevent tumors on a daily level, but it doesn’t hurt that capacity to have a clearing-out every couple of weeks; so says the science (linked above). Note my imperfection: I take it at weekends instead of for two days every two weeks (as is standard in studies, like those linked above), because it is simpler than remembering to count the weeks.
Cognitive exercise
Lest we forget, exercising our mind is also important! In my case:
- I’m blessed to have work that’s quite cognitively stimulating; our topics here at 10almonds are interesting. If it weren’t for that, I’d still be reading and writing a lot.
- I play chess, though these days I don’t play competitively anymore, and play rather for the social aspect, but this too is important in avoiding cognitive decline.
- I am one of those people who compulsively learns languages, and uses them a lot. This is very beneficial, as language ability is maintained in a few small areas of the brain, and it’s very much “use it or lose it”. Now, while I may not need my French or Russian or Arabic to keep the lights on in this part of the brain or that, the fact that I am pushing my limits every day is the important part. It’s not about how much I know—it’s about how much I engage those parts of my brain on a daily basis. Thus, even if you speak only one language right now, learning even just one more, and learning even only a little bit, you will gain the brain benefits—because you’re engaging it regularly in a new way, and that forces the brain to wire new synapses and also to maintain volume in those parts.
See also: How To Reduce Your Alzheimer’s Risk
And about language-learning specifically: An Underrated Tool Against Alzheimer’s ←this also shows how you don’t have to be extreme about language learning like I admittedly am.
How’s all this working out for me?
I can say: it works! My general health is better now than it was decades ago. I’ve personally focused a lot on reducing inflammation, and that really pays dividends when it comes to the rest of health. I didn’t talk about it above, but focusing on my sleep regularity and quality has helped a lot too.
In terms of measurable results, I recently had a general wellness checkup done by means of a comprehensive panel of 14 blood tests, and various physical metrics (BMI, body fat %, blood pressure, etc), and per those, I could not be in better health; it was as though I had cheated and written in all the best answers. I say this not to brag (you don’t know me, after all), but rather to say: it can be done!
Even without extreme resources, and without an abundance of free time, etc, it can be done!
Caveat: if you have some currently incurable chronic disease, there may be some limits. For example, if you have Type 1 Diabetes, probably your HbA1c* is going to be a little off even if you do everything right.
*HbA1c = glycated hemoglobin, a very accurate measure of what your blood glucose has been on average for the past 2–3 months—why 2–3 months? Because that’s the approximate lifespan of a red blood cell, and we’re measuring how much hemoglobin (in the red blood cells) has been glycated (because of blood glucose).
In summary
The stuff we write about at 10almonds can be implemented, on a modest budget and while juggling responsibilities (work, family, classes, etc).
I’m not saying that my lifestyle should be everyone’s template, but it’s at least an example of one that can work.
- Maybe you hate walking and love swimming.
- Maybe you have no wish to give up fish and eggs, say (both of which are fine/good in moderation healthwise).
- Maybe you have different priorities with supplements.
- Maybe you find language-learning uninteresting but take singing lessons.
- And so on.
In the absolute fewest words, the real template is:
- Decide your health priorities (what matters most for you)
- Look them up on 10almonds
- Put the things into action in a way that works for you!
Take care!
Share This Post
Related Posts
-
The Liver Cure – by Dr. Russell Blaylock
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about How To Unfatty A Fatty Liver, but there’s a lot more that can be said in a book that we couldn’t fit into our article.
In this book, Dr. Blaylock looks at the causes and symptoms of liver disease, the mechanisms behind such, and how we can adjust our dietary habits (and other things) to do better for ourselves.
While the book’s primary focus is on diet, he does also look at medications (especially: those that hinder liver health, which are many, including simple/common stuff like Tylenol and similar), and the effects of different lifestyle choices, including ones that aren’t diet-related.
Because most people’s knowledge of liver disease starts and ends at “don’t drink yourself to death”, this book is an important tome of knowledge for actually keeping this critical organ in good order—especially since symptoms of liver disease can initially be subtle, and slow to show, often escaping notice until it’s already far, far worse than it could have been.
Many people find out by experiencing liver failure.
The writing style is… A little repetitive for this reviewer’s preference, but it does make sure that you won’t miss things. Also, when it comes to supplements, he repeatedly recommends a particular company, and it’s not clear whether he has a financial interest there. But the actual medical information is good and important and comprehensive.
Bottom line: if you’d like to keep your liver in good health, this is a book that will help you to do just that.
Click here to check out The Liver Cure, and keep yours working well!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why Some People Get Sick More (And How To Not Be One Of Them)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Some people have never yet had COVID (so far so good, this writer included); others are on their third bout already; others have not been so lucky and are no longer with us to share their stories.
Obviously, even the healthiest and/or most careful person can get sick, and it would be folly to be complacent and think “I’m not a person who gets sick; that happens to other people”.
Nor is COVID the only thing out there to worry about; there’s always the latest outbreak-du-jour of something, and there are always the perennials such as cold and flu—which are also not to be underestimated, because both weaken us to other things, and flu has killed very many, from the 50,000,000+ in the 1918 pandemic, to the 700,000ish that it kills each year nowadays.
And then there are the combination viruses:
Move over, COVID and Flu! We Have “Hybrid Viruses” To Contend With Now
So, why are some people more susceptible?
Firstly, some people are simply immunocompromised. This means for example that:
- perhaps they have an inflammatory/autoimmune disease of some kind (e.g. lupus, rheumatoid arthritis, type 1 diabetes), or…
- perhaps they are taking immunosuppressants for some reason (e.g. because they had an organ transplant), or…
- perhaps they have a primary infection that leaves them vulnerable to secondary infections. Most infections will do this to some degree or another, but some are worse for it than others; untreated HIV is a clear example. The HIV itself may not kill people, but (if untreated) the resultant AIDS will leave a person open to being killed by almost any passing opportunistic pathogen. Pneumonia of various kinds being high on the list, but it could even be something as simple as the common cold, without a working immune system to fight it.
See also: How To Prevent (Or Reduce) Inflammation
And for that matter, since pneumonia is a very common last-nail-in-the-coffin secondary infection (especially: older people going into hospital with one thing, getting a secondary infection and ultimately dying as a result), it’s particularly important to avoid that, so…
See also: Pneumonia: What We Can & Can’t Do About It
Secondly, some people are not immunocompromised per the usual definition of the word, but their immune system is, arguably, compromised.
Cortisol, the stress hormone, is an immunosuppressant. We need cortisol to live, but we only need it in small bursts here and there (such as when we are waking up the morning). When high cortisol levels become chronic, so too does cortisol’s immunosuppressant effect.
Top things that cause elevated cortisol levels include:
- Stress
- Alcohol
- Smoking
Thus, the keys here are to 1) not smoke 2) not drink, ideally, or at least keep consumption low, but honestly even one drink will elevate cortisol levels, so it’s better not to, and 3) manage stress.
See also: Lower Your Cortisol! (Here’s Why & How)
Other modifiable factors
Being aware of infection risk and taking steps to reduce it (e.g. avoiding being with many people in confined indoor places, masking as appropriate, handwashing frequently) is a good preventative strategy, along with of course getting any recommended vaccines as they come available.
What if they fail? How can we boost the immune system?
We talked about not sabotaging the immune system, but what about actively boosting it? The answer is yes, we certainly can (barring serious medical reasons why not), as there are some very important lifestyle factors too:
Beyond Supplements: The Real Immune-Boosters!
One final last-line thing…
Since if we do get an infection, it’s better to know sooner rather than later… A recent study shows that wearable activity trackers can (if we pay attention to the right things) help predict disease, including highlighting COVID status (positive or negative) about as accurately (88% accuracy) as rapid screening tests. Here’s a pop-science article about it:
Wearable activity trackers show promise in detecting early signals of disease
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
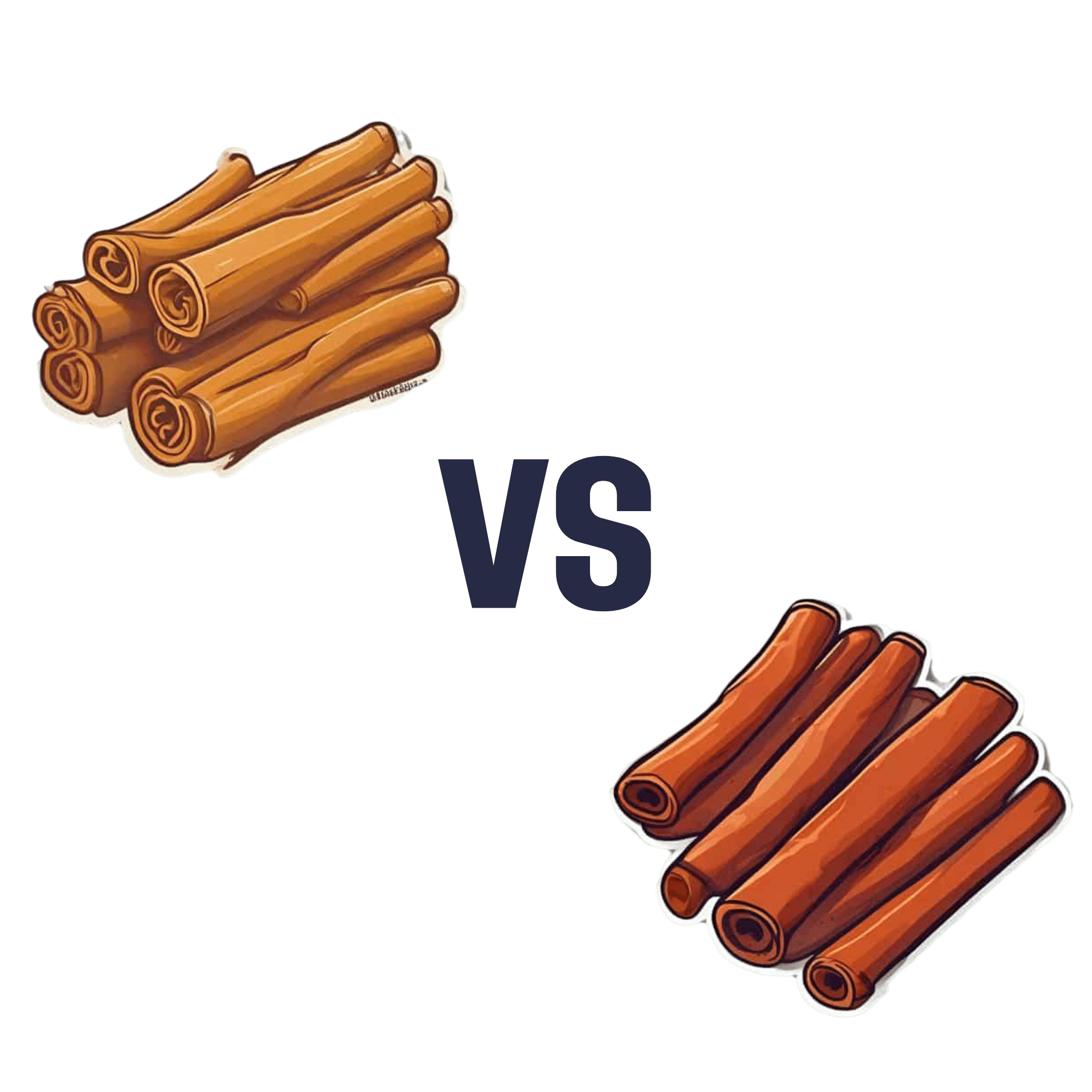
Sweet Cinnamon vs Regular Cinnamon – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sweet cinnamon to regular cinnamon, we picked the sweet.
Why?
In this case, it’s not close. One of them is health-giving and the other is poisonous (but still widely sold in supermarkets, especially in the US and Canada, because it is cheaper).
It’s worth noting that “regular cinnamon” is a bit of a misnomer, since sweet cinnamon is also called “true cinnamon”. The other cinnamon’s name is formally “cassia cinnamon”, but marketers don’t tend to call it that, preferring to calling it simply “cinnamon” and hope consumers won’t ask questions about what kind, because it’s cheaper.
Note: this too is especially true in the US and Canada, where for whatever reason sweet cinnamon seems to be more difficult to obtain than in the rest of the world.
In short, both cinnamons contain cinnamaldehyde and coumarin, but:
- Sweet/True cinnamon contains only trace amounts of coumarin
- Regular/Cassia cinnamon contains about 250x more coumarin
Coumarin is heptatotoxic, meaning it poisons the liver, and the recommended safe amount is 0.1mg/kg, so it’s easy to go over that with just a couple of teaspoons of cassia cinnamon.
You might be wondering: how can they get away with selling something that poisons the liver? In which case, see also: the alcohol aisle. Selling toxic things is very common; it just gets normalized a lot.
Cinnamaldehyde is responsible for cinnamon’s healthier properties, and is found in reasonable amounts in both cinnamons. There is about 50% more of it in the regular/cassia than in the sweet/true, but that doesn’t come close to offsetting the potential harm of its higher coumarin content.
Want to learn more?
You may like to read:
- A Tale Of Two Cinnamons ← this one has more of the science of coumarin toxicity, as well as discussing (and evidencing) cinnamaldehyde’s many healthful properties against inflammation, cancer, heart disease, neurodegeneration, etc
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: