Cold Weather Health Risks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many Are Cold; Few Are Frozen
Many of those of us in the Northern Hemisphere are getting hit with a cold spell around now. How severe that may be depends on more precisely where we are, but it’s affecting a lot of people. So, with apologies to our readers in Australia, we’re going to do a special on that today.
Acute cold is, for most people, good for the health:
A Cold Shower A Day Keeps The Doctor Away?
Persistent cold, not so much. Let’s look at the risks, and what can be done about them…
Hypothermia
It kills. Don’t let it kill you or your loved ones.
And, this is really important: it doesn’t care whether you’re on a mountain or not.
In other words: a lot of people understand (correctly!) that hypothermia is a big risk to hikers, climbers, and the like. But if the heating goes out in your house and the temperature drops for long enough before the heating is fixed, you can get hypothermia there too just the same if you’re not careful.
How cold is too cold? It doesn’t even have to be sub-zero. According to the CDC, temperatures of 4℃ (40℉) can be low enough to cause hypothermia if other factors combine:
CDC | Prevent Hypothermia & Frostbite ← you can also see the list of symptoms to watch out for, there!
Skin health
Not generally an existential risk, but we may as well stay healthy as not!
Cold air often means dry air, so use a moisturizer with an oil base (if you don’t care for fancy beauty products, ordinary coconut oil is top-tier).
Bonus if you do it after a warming bath/shower!
Heart health
Cold has a vasconstricting effect; that is to say, it causes the body’s vasculature to shrink, increasing localized blood pressure. If it’s a cold shower as above, that can be very invigorating. If it’s a week of sub-zero temperatures, it can become a problem.
❝Shoveling a little snow off your sidewalk may not seem like hard work. However, […] combined with the fact that the exposure to cold air can constrict blood vessels throughout the body, you’re asking your heart to do a lot more work in conditions that are diminishing the heart’s ability to function at its best.❞
Source: Snow shoveling, cold temperatures combine for perfect storm of heart health hazards
If you have a heart condition, please do not shovel snow. Let someone else do it, or stay put.
And if you are normally able to exercise safely? Unless you’re sure your heart is in good order, exercising in the warmth, not the cold, seems to be the best bet.
See also: Heart Attack: His & Hers (Be Prepared!) ← can you remember which symptoms are for which sex? If not, now’s a good time to refresh that knowledge.
Immune health
We recently discussed how cold weather indirectly increases the risk of respiratory viral infection:
The Cold Truth About Respiratory Infections
So, now’s the time to be extra on-guard about that.
See also: Beyond Supplements: The Real Immune-Boosters!
Balance
Icy weather increases the risk of falling. If you think “having a fall” is something that happens to other/older people, please remember that there’s a first time for everything. Some tips:
- Walk across icy patches with small steps in a flat-footed fashion like a penguin.
- It may not be glamorous, but neither is going A-over-T and breaking (or even just spraining) things.
- Use a handrail if available, even if you don’t think you need to.
You can also check out our previous article about falling (avoiding falling, minimizing the damage of falling, etc):
Fall Special: Some Fall-Themed Advice
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Mammography AI Can Cost Patients Extra. Is It Worth It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As I checked in at a Manhattan radiology clinic for my annual mammogram in November, the front desk staffer reviewing my paperwork asked an unexpected question: Would I like to spend $40 for an artificial intelligence analysis of my mammogram? It’s not covered by insurance, she added.
I had no idea how to evaluate that offer. Feeling upsold, I said no. But it got me thinking: Is this something I should add to my regular screening routine? Is my regular mammogram not accurate enough? If this AI analysis is so great, why doesn’t insurance cover it?
I’m not the only person posing such questions. The mother of a colleague had a similar experience when she went for a mammogram recently at a suburban Baltimore clinic. She was given a pink pamphlet that said: “You Deserve More. More Accuracy. More Confidence. More power with artificial intelligence behind your mammogram.” The price tag was the same: $40. She also declined.
In recent years, AI software that helps radiologists detect problems or diagnose cancer using mammography has been moving into clinical use. The software can store and evaluate large datasets of images and identify patterns and abnormalities that human radiologists might miss. It typically highlights potential problem areas in an image and assesses any likely malignancies. This extra review has enormous potential to improve the detection of suspicious breast masses and lead to earlier diagnoses of breast cancer.
While studies showing better detection rates are extremely encouraging, some radiologists say, more research and evaluation are needed before drawing conclusions about the value of the routine use of these tools in regular clinical practice.
“I see the promise and I hope it will help us,” said Etta Pisano, a radiologist who is chief research officer at the American College of Radiology, a professional group for radiologists. However, “it really is ambiguous at this point whether it will benefit an individual woman,” she said. “We do need more information.”
The radiology clinics that my colleague’s mother and I visited are both part of RadNet, a company with a network of more than 350 imaging centers around the country. RadNet introduced its AI product for mammography in New York and New Jersey last February and has since rolled it out in several other states, according to Gregory Sorensen, the company’s chief science officer.
Sorensen pointed to research the company conducted with 18 radiologists, some of whom were specialists in breast mammography and some of whom were generalists who spent less than 75% of their time reading mammograms. The doctors were asked to find the cancers in 240 images, with and without AI. Every doctor’s performance improved using AI, Sorensen said.
Among all radiologists, “not every doctor is equally good,” Sorensen said. With RadNet’s AI tool, “it’s as if all patients get the benefit of our very top performer.”
But is the tech analysis worth the extra cost to patients? There’s no easy answer.
“Some people are always going to be more anxious about their mammograms, and using AI may give them more reassurance,” said Laura Heacock, a breast imaging specialist at NYU Langone Health’s Perlmutter Cancer Center in New York. The health system has developed AI models and is testing the technology with mammograms but doesn’t yet offer it to patients, she said.
Still, Heacock said, women shouldn’t worry that they need to get an additional AI analysis if it’s offered.
“At the end of the day, you still have an expert breast imager interpreting your mammogram, and that is the standard of care,” she said.
About 1 in 8 women will be diagnosed with breast cancer during their lifetime, and regular screening mammograms are recommended to help identify cancerous tumors early. But mammograms are hardly foolproof: They miss about 20% of breast cancers, according to the National Cancer Institute.
The FDA has authorized roughly two dozen AI products to help detect and diagnose cancer from mammograms. However, there are currently no billing codes radiologists can use to charge health plans for the use of AI to interpret mammograms. Typically, the federal Centers for Medicare & Medicaid Services would introduce new billing codes and private health plans would follow their lead for payment. But that hasn’t happened in this field yet and it’s unclear when or if it will.
CMS didn’t respond to requests for comment.
Thirty-five percent of women who visit a RadNet facility for mammograms pay for the additional AI review, Sorensen said.
Radiology practices don’t handle payment for AI mammography all in the same way.
The practices affiliated with Boston-based Massachusetts General Hospital don’t charge patients for the AI analysis, said Constance Lehman, a professor of radiology at Harvard Medical School who is co-director of the Breast Imaging Research Center at Mass General.
Asking patients to pay “isn’t a model that will support equity,” Lehman said, since only patients who can afford the extra charge will get the enhanced analysis. She said she believes many radiologists would never agree to post a sign listing a charge for AI analysis because it would be off-putting to low-income patients.
Sorensen said RadNet’s goal is to stop charging patients once health plans realize the value of the screening and start paying for it.
Some large trials are underway in the United States, though much of the published research on AI and mammography to date has been done in Europe. There, the standard practice is for two radiologists to read a mammogram, whereas in the States only one radiologist typically evaluates a screening test.
Interim results from the highly regarded MASAI randomized controlled trial of 80,000 women in Sweden found that cancer detection rates were 20% higher in women whose mammograms were read by a radiologist using AI compared with women whose mammograms were read by two radiologists without any AI intervention, which is the standard of care there.
“The MASAI trial was great, but will that generalize to the U.S.? We can’t say,” Lehman said.
In addition, there is a need for “more diverse training and testing sets for AI algorithm development and refinement” across different races and ethnicities, said Christoph Lee, director of the Northwest Screening and Cancer Outcomes Research Enterprise at the University of Washington School of Medicine.
The long shadow of an earlier and largely unsuccessful type of computer-assisted mammography hangs over the adoption of newer AI tools. In the late 1980s and early 1990s, “computer-assisted detection” software promised to improve breast cancer detection. Then the studies started coming in, and the results were often far from encouraging. Using CAD at best provided no benefit, and at worst reduced the accuracy of radiologists’ interpretations, resulting in higher rates of recalls and biopsies.
“CAD was not that sophisticated,” said Robert Smith, senior vice president of early cancer detection science at the American Cancer Society. Artificial intelligence tools today are a whole different ballgame, he said. “You can train the algorithm to pick up things, or it learns on its own.”
Smith said he found it “troubling” that radiologists would charge for the AI analysis.
“There are too many women who can’t afford any out-of-pocket cost” for a mammogram, Smith said. “If we’re not going to increase the number of radiologists we use for mammograms, then these new AI tools are going to be very useful, and I don’t think we can defend charging women extra for them.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
Tips For Avoiding/Managing Rheumatoid Arthritis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Avoiding/Managing Rheumatoid Arthritis
Arthritis is the umbrella term for a cluster of joint diseases involving inflammation of the joints, hence “arthr-” (joint) “-itis” (suffix used to denote inflammation). These are mostly, but not all, autoimmune diseases, in which the body’s immune system mistakenly attacks our own joints.
Inflammatory vs Non-Inflammatory Arthritis
Arthritis is broadly divided into inflammatory arthritis and non-inflammatory arthritis.
You may be wondering: how does one get non-inflammatory inflammation of the joints?
The answer is, in “non-inflammatory” arthritis, such as osteoarthritis, the damage comes first (by general wear-and-tear) and inflammation generally follows as part of the symptoms, rather than the cause. So the name can be a little confusing. In the case of osteo- and other “non-inflammatory” forms of arthritis, you definitely still want to keep your inflammation at bay as best you can, but it’s not as absolutely critical a deal as it is for “inflammatory” forms of arthritis.
We’ll tackle the beast that is osteoarthritis another day, however.
Today we’re going to focus on…
Rheumatoid Arthritis
This is the most common of the autoimmune forms of arthritis. Some quick facts:
- It affects a little under 1% of the global population, but the older we get, the more likely it becomes
- Early onset of rheumatoid arthritis is most likely to show up around the age of 50 (but it can show up at any age)
- However, incidence (not onset) of rheumatoid arthritis peaks in the 70s age bracket
- It is 2–4 times more common in women than in men
- Approximately one third of people stop work within two years of its onset, and this increases thereafter.
Well, that sounds gloomy.
Indeed it’s not fun. There’s a lot of stiffness and aching of joints (often with swelling too), loss of joint function can be common, and then there are knock-on effects like fatigue, weakness, and loss of appetite.
Beyond that it’s an autoimmune disorder, its cause is not known, and there is no known cure.
Is there any good news?
If you don’t have rheumatoid arthritis at the present time, you can reduce your risk factors in several ways:
- Having an anti-inflammatory diet. Get plenty of fiber, greens, and berries. Fatty fish is great too, as are oily nuts. On the other side of things, high consumption of salt, sugar, alcohol, and red meat are associated with a greater risk of developing rheumatoid arthritis.
- Not smoking. Smoking is bad for pretty much everything, including your chances of developing rheumatoid arthritis.
- Not being obese. This one may be more a matter of correlation than causation, because of the dietary factors (if one eats an anti-inflammatory diet, obesity is less likely), but the association is there.
There are other risk factors that are harder to control, such as genetics, age, sex, and having a mother who smoked.
See: Genetic and environmental risk factors for rheumatoid arthritis
What if I already have rheumatoid arthritis?
If you already have rheumatoid arthritis, it becomes a matter of symptom management.
First, reduce inflammation any (reasonable) way you can. We did a main feature on this before, so we’ll just drop that again here:
Next, consider the available medications. Your doctor may or may not have discussed all of the options with you, so be aware that there are more things available than just pain relief. To talk about them all would require a whole main feature, so instead, here’s a really well-compiled list, along with explanations about each of them, up to date as of this year:
Rheumatoid Arthritis Medication List (And What They Do, And How)
Finally, consider other lifestyle adjustments to manage your symptoms. These include:
- Exercise—gently, though! You do not want to provoke a flare-up, but you do want to maintain your mobility as best you can. There’s a use-it-or-lose-it factor here. Swimming and yoga are great options, as is tai chi. You may want to avoid exercises that involve repetitive impacts to your joints, like running.
- Rest—while keeping mobility going. Get good sleep at night (this is important), but don’t make your bed your new home, or your mobility will quickly deteriorate.
- Hot & cold—both can help, and alternating them can reduce inflammation and stiffness by improving your body’s ability to respond appropriately to these stimuli rather than getting stuck in an inappropriate-response state of inflammation.
- Mobility aids—if it helps, it helps. Maybe you only need something during a flare-up, but when that’s the case, you want to be as gentle on your body as possible while keeping moving, so if crutches, handrails etc help, then by all means get them and use them.
- Go easy on the use of braces, splints, etc—these can offer short-term relief, but at a long term cost of loss of mobility. Only you can decide where to draw the line when it comes to that trade-off.
You can also check out our previous article:
Managing Chronic Pain (Realistically!)
Take good care of yourself!
Share This Post
-
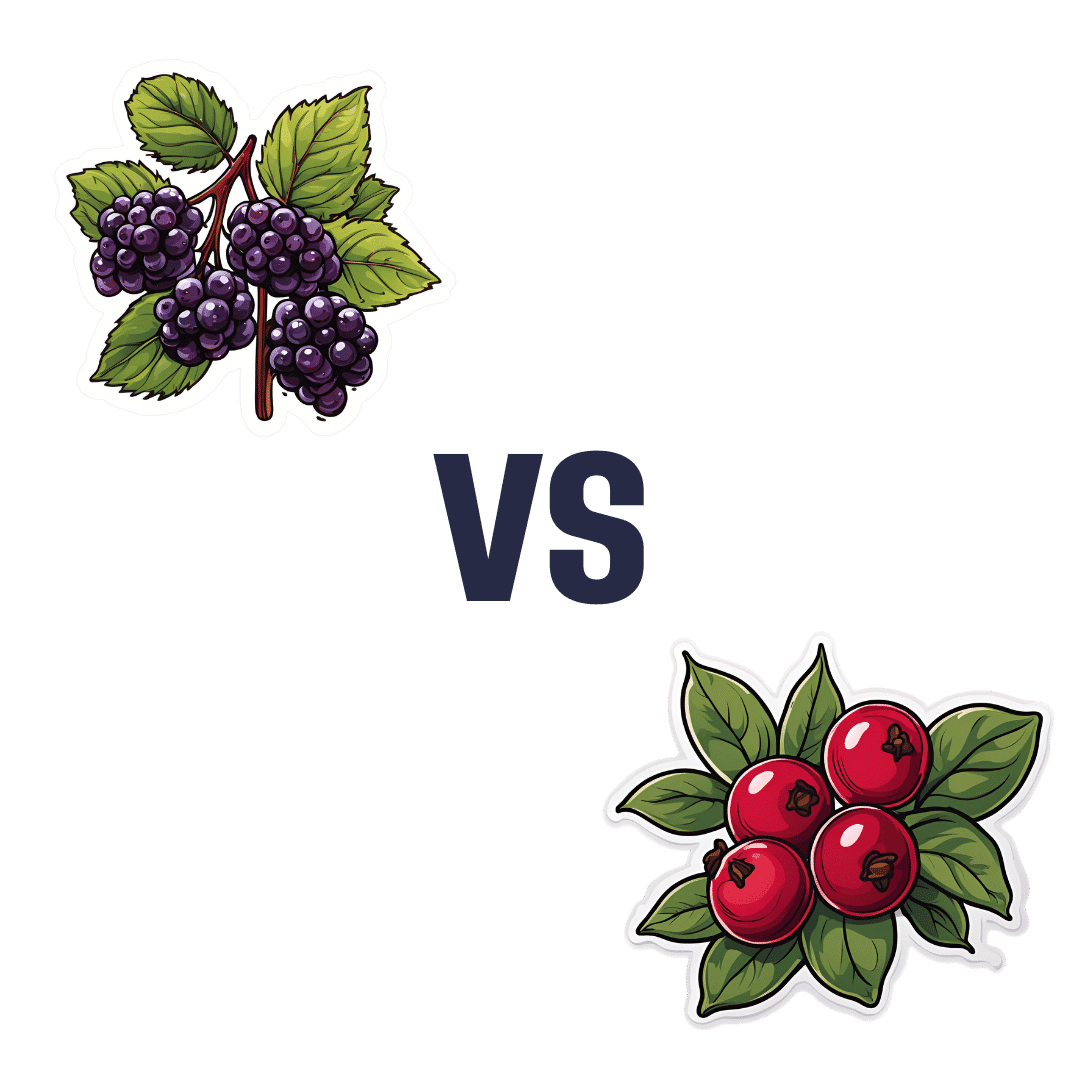
Elderberries vs Cranberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing elderberries to cranberries, we picked the elderberries.
Why?
In terms of macros, elderberry has slightly more carbs and 2x the fiber, the ratio of which gives elderberries the lower glycemic index also. A win for elderberries, then.
Looking at the vitamins, elderberries have more of vitamins A, B1, B2, B3, B6, B9, and C, while cranberries have more vitamin B5. An easy win for elderberries in this category.
In the category of minerals, we see a similar story: elderberries have more calcium, copper, iron, phosphorus, potassium, selenium, and zinc, while cranberries have (barely) more magnesium. Another clear win for elderberries.
Both of these fruits have additional “special” properties, and it’s worth noting that:
- elderberries’ bonus properties include that they significantly hasten recovery from upper respiratory tract viral infections.
- cranberries’ bonus properties (including: famously very good at reducing UTI risk) come with some warnings, including that they may increase the risk of kidney stones if you are prone to such, and also that cranberries have anti-clotting effects, which are great for heart health but can be a risk of you’re on blood thinners or have a bleeding disorder.
You can read about both of these fruits’ special properties in more detail below:
Want to learn more?
You might like to read:
- Herbs for Evidence-Based Health & Healing ← elderberry is in the list. We haven’t, at time of writing, done a main feature just on elderberry. Maybe soon!
- Health Benefits Of Cranberries (But: You’d Better Watch Out)
Enjoy!
Share This Post
Related Posts
-
Pumpkin Seeds vs Watermelon Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pumpkin seeds to watermelon seeds, we picked the watermelon.
Why?
Starting with the macros: pumpkin seeds have a lot more carbs, while watermelon seeds have a lot more protein, despite pumpkin seeds being famous for such. They’re about equal on fiber. In terms of fats, watermelon seeds are higher in fats, and yes, these are healthy fats, mostly polyunsaturated.
When it comes to vitamins, pumpkin seeds are marginally higher in vitamins A and C, while watermelon seeds are a lot higher in vitamins B1, B2, B3, B5, B6, and B9. An easy win for watermelon seeds here.
In the category of minerals, despite being famous for zinc, pumpkin seeds are higher only in potassium, while watermelon seeds are higher in iron, magnesium, manganese, and phosphorus; the two seeds are equal on calcium, copper, and zinc. Another win for watermelon seeds.
In short, enjoy both, but watermelon has more to offer. Of course, if buying just the seeds and not the whole fruit, it’s generally easier to find pumpkin seeds than watermelon seeds, so do bear in mind that pumpkin seeds’ second place isn’t that bad here—it’s just a case of a very nutritious food looking bad by standing next to an even better one.
Want to learn more?
You might like to read:
Seed Saving Secrets – by Alice Mirren
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Gut Renovation – by Dr. Roshini Raj, with Sheila Buff
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Unless we actually feel something going on down there, gut health is an oft-neglected part of overall health—which is unfortunate, because invisible as it may often be, it affects so much.
Gastroenterologist Dr. Roshini Raj gives us all the need-to-know information, explanations of why things happen the way they do with regard to the gut, and tips, tricks, and hacks to improve matters.
She also does some mythbusting along the way, and advises about what things don’t make a huge difference, including what medications don’t have a lot of evidence for their usefulness.
The style is easy-reading pop-science, with plenty of high-quality medical content.
Reading between the lines, a lot of the book as it stands was probably written by the co-author, Sheila Buff, who is a professional ghostwriter and specializes in working closely with doctors to produce works that are readable and informative to the layperson while still being full of the doctor’s knowledge and expertise. So a reasonable scenario is that Dr. Raj gave her extensive notes, she took it from there, passed it back to her for medical corrections, and they had a little back and forth until it was done. Whatever their setup, the end result was definitely good!
Bottom line: if you’d like a guide to gut health that’s practical and easy to read, while being quite comprehensive and certainly a lot more than “eat probiotics and fiber”, then this book is a fine choice.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Do HIIT (Without Wrecking Your Body)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Do HIIT (Without Wrecking Your Body)
High-Intensity Interval Training, henceforth “HIIT”, is a well-researched and well-evidenced approach to exercise that gives powerful health benefits.
Specifically, health benefits that we don’t get from moderate exercise (as important as that is too) or endurance training.
Super-quick overview of the benefits first:
- Burns more calories than other forms of exercise
- Boosts your metabolic rate for hours afterwards
- …which means it actually works* for fat loss
- Reduces blood pressure (unless already healthy)
- Can promote muscle growth (depends on other factors)
*remember that most forms of exercise aren’t very good for fat loss, because our metabolism will slow afterwards to compensate. So HIIT flipping this one is quite a big deal.
What actually is it?
HIIT means exercise sessions in which one alternates between high intensity “maximum effort” bursts, and short recovery periods during which more moderate exercise is performed.
An example for runners could be switching between sprinting or jogging, changing mode each time one passes a street light.
❝A total of only two minutes of sprint interval exercise was sufficient to elicit similar responses as 30 minutes of continuous moderate intensity aerobic exercise❞
What did you mean about not wrecking your body? Is that… Likely?
Hopefully not, but it’s a barrier to some! We are not all twenty-something college athletes, after all, and our bodies aren’t always as durable as they used to be.
HIIT relies on intense exercise and short recovery periods, but what if our bodies are not accustomed to intense exercise, and need longer recovery periods? Can we still get the same benefits?
The trick is not to change the intensity or the recovery periods, but the exercise itself.
For HIIT to work the “intense” part has to be best-effort or approaching such. That part’s not negotiable. The recovery periods can be stretched a bit if you need to, but with the right tweaks, you ideally won’t have to do that.
Great! How?
First, note that you can do resistance interval training without impact. For example, if you crank up the resistance on an exercise bike or similar machine, you will be doing resistance training along with your cardio, and you’ll be doing it without the impact on your joints that you would if out pounding the pavement on foot.
(Running is fine if your body is used to it, but please don’t make HIIT your first running exercise in a decade)
Second, consider your environment. That exercise bike? You can get off it any time and you’re already at home (or perhaps your gym, with your car outside). Not so if you took up mountain biking or road racing.
Third, go for what is gentle in motion, even if it’s not resistance work per se. Swimming is a fabulous option for most people, and can absolutely be done with HIIT principles. Since vision is often obscured while swimming, counting strokes can be a good way to do HIIT. For example, ten strokes max effort, ten strokes normal, repeat. Do make sure you are aware of where the end of the pool is, though!
Fourth, make it fun! Ok, this one’s not about the safety quite so much, but it is about sustainability, and that’s critical for practical purposes too. You will only continue an exercise routine that you enjoy, after all.
- Could you curate a musical playlist that shifts tempo to cue your exercise mode intervals?
- Could you train with an exercise partner? Extra fun if this has a “relay race” feel to it, i.e. when one person completes a high intensity interval, the other person must now begin theirs.
Need some pointers getting started?
There are a lot of HIIT apps out there, so you can just search for that on your device of choice.
But!
We at 10almonds have recommended 7-Minute Workout before, which is available for iOS and for Android, and we stand by that as a great starting choice.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: