How to Permanently Loosen a Tight Psoas
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What Is Your Psoas?
Your psoas is a deep muscle in your lower back and hip area that connects your spine to your thigh bone. It helps you bend your hips and spine, making it a hip flexor.
In today’s video, Your Wellness Nerd (the YouTube channel behind the video below) has revealed some great tips on loosening said tight hip flexors!
How to loosen them
First off, the big reveal…your tight psoas is likely stemming from an overlooked cause: your lower back! The video kicks off with a simple technique to loosen up that stiff area in your lower back. All you need is a foam roller.
But, before diving into the exercises, it’s essential to gauge your current flexibility. A basic hip flexor stretch serves as a pre-test.
Note: the goal here isn’t to stretch, but rather to feel how tight you are.
After testing, it’s time to roll…literally. Working through the lower back, use your roller or tennis ball to any find stiff spots and loosen them out; those spots are likely increasing the tension on your psoas.
After some rolling, retest with the hip flexor stretch. Chances are, you’ll feel more mobility and less tightness right away.
Note: this video focuses on chronic psoas issues. If you have sore psoas from a muscular workout, you may want to read our piece on speeding up muscle recovery.
Is That All?
But wait, there’s more! The video also covers two more exercises specifically targeting the psoas. This one’s hard to describe, so we recommend watching the video. However, to provide an overview, you’re doing the “classic couch stretch”, but with a few alterations.
Next, the tennis ball technique zeroes in on specific tight spots in the psoas. By lying on the ball and adjusting its position around the hip area, you can likely release some deeply held tension.
Additionally, some of our readers advocate for acupuncture for psoas relief – we’ve done an acupuncture myth-busting article here for reference.
Other Sources
If you’re looking for some more in-depth guides on stretching your psoas, and your body in general, we’ve made a range of 1-minute summaries of books that specifically target stretching:
- 11 Minutes to Pain-Free Hips (perfect for psoas muscles)
- Stretching Scientifically
- Stretching & Mobility
- Stretching to Stay Young
The final takeaway? If you’re constantly battling tight psoas muscles despite trying different exercises and stretches, it might be time to look at your lower back and your daily habits. This video isn’t just a band-aid fix; it’s about addressing the root cause for long-term relief:
How did you find that video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Purple Parsnip’s Bioactive Brain Benefits (& more)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This Root Might Be A Guardian Angel
Sometimes we go searching for supplements to research; sometimes supplements present themselves for examination! In this case, our attention was grabbed by a headline:
Angelica gigas extract emerges as a potential treatment for vascular disease
Angelica who?
Angelica gigas, also called the purple parsnip (amongst other names), is a flowering plant native to Korea. It has assorted medicinal properties, and in this case, it was its heart-healthy benefits that were making news:
❝Ultimately, this study presents clearly evidence that Angelica gigas extract is a promising natural product-based functional food/herbal medicine candidate for preventing or regulating hyperlipidemic cardiovascular complications❞
But it has a lot more to offer…
The root has various bioactive metabolites, but the compounds that most studies are most interested in are decursin and decursinol, for their neuroprotective and cognitive enhancement effects:
❝[C]rude extracts and isolated components from the root of A. gigas exhibited neuroprotective and cognitive enhancement effects.
Neuronal damage or death is the most important factor for many neurodegenerative diseases.
In addition, recent studies have clearly demonstrated the possible mechanisms behind the neuroprotective action of extracts/compounds from the root of A. gigas.❞
That middle paragraph there? That’s one of the main pathogenic processes of Alzheimer’s, Parkinson’s, Huntington’s, and Multiple Sclerosis.
Angelica gigas attenuates (reduces the force of) that process:
❝The published reports revealed that the extracts and isolated components from the root of A. gigas showed neuroprotective and cognitive enhancement properties through various mechanisms such as anti-apoptosis, antioxidative actions, inhibiting mRNA and protein expressions of inflammatory mediators and regulating a number of signaling pathways.
In conclusion, the A. gigas root can serve as an effective neuroprotective agent by modulating various pathophysiological processes❞
Read more: Neuroprotective and Cognitive Enhancement Potentials of Angelica gigas Nakai Root: A Review
Beyond neuroprotection & cognitive enhancement
…and also beyond its protection against vascular disease, which is what got our attention…
Angelica gigas also has antioxidant properties, anti-cancer properties, and general immune-boosting properties.
We’ve only so much room, so: those links above will take you to example studies for those things, but there are plenty more where they came from, so we’re quite confident in this one.
Of course, what has antioxidant properties is usually anti-inflammatory, anti-cancer, and anti-aging, because these things are reliant on many of the same processes as each other, with a lot of overlap.
Where can we get it?
We don’t sell it, but here’s an example product on Amazon, for your convenience
Enjoy!
Share This Post
-
Retrain Your Brain – by Dr. Seth Gillihan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
15-Minute Arabic”, “Sharpen Your Chess Tactics in 24 Hours”, “Change Your Life in 7 Days”, “Cognitive Behavioral Therapy in 7 weeks”—all real books from this reviewer’s shelves.
The thing with books with these sorts of time periods in the titles is that the time period in the title often bears little relation to how long it takes to get through the book. So what’s the case here?
You’ll probably get through it in more like 7 days, but the pacing is more important than the pace. By that we mean:
Dr. Gillihan starts by assuming the reader is at best “in a rut”, and needs to first pick a direction to head in (the first “week”) and then start getting one’s life on track (the second “week”).
He then gives us, one by one, an array of tools and power-ups to do increasingly better. These tools aren’t just CBT, though of course that features prominently. There’s also mindfulness exercises, and holistic / somatic therapy too, for a real “bringing it all together” feel.
And that’s where this book excels—at no point is the reader left adrift with potential stumbling-blocks left unexamined. It’s a “whole course”.
Bottom line: whether it takes you 7 hours or 7 months, “Cognitive Behavioral Therapy in 7 Weeks” is a CBT-and-more course for people who like courses to work through. It’ll get you where you’re going… Wherever you want that to be for you!
Share This Post
-
How we treat catchment water to make it safe to drink
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most of us are fortunate that, when we turn on the tap, clean, safe and high-quality water comes out.
But a senate inquiry into the presence of PFAS or “forever chemicals” is putting the safety of our drinking water back in the spotlight.
Lidia Thorpe, the independent senator leading the inquiry, says Elders in the Aboriginal community of Wreck Bay in New South Wales are “buying bottled water out of their aged care packages” due to concerns about the health impacts of PFAS in their drinking water.
So, how is water deemed safe to drink in Australia? And why does water quality differ in some areas?
Here’s what happens between a water catchment and your tap.
Andriana Syvanych/Shutterstock Human intervention in the water cycle
There is no “new” water on Earth. The water we drink can be up to 4.5 billion years old and is continuously recycled through the hydrological cycle. This transfers water from the ground to the atmosphere through evaporation and back again (for example, through rain).
Humans interfere with this natural cycle by trapping and redirecting water from various sources to use. A lot happens before it reaches your home.
The quality of the water when you turn on the tap depends on a range of factors, including the local geology, what kind of activities happen in catchment areas, and the different treatments used to process it.
Maroondah dam in Healesville, Victoria. doublelee/Shutterstock How do we decide what’s safe?
The Australian Drinking Water Guidelines define what is considered safe, good-quality drinking water.
The guidelines set acceptable water quality values for more than 250 physical, chemical and bacterial contaminants. They take into account any potential health impact of drinking the contaminant over a lifetime as well as aesthetics – the taste and colour of the water.
The guidelines are not mandatory but provide the basis for determining if the quality of water to be supplied to consumers in all parts of Australia is safe to drink. The guidelines undergo rolling revision to ensure they represent the latest scientific evidence.
From water catchment to tap
Australians’ drinking water mainly comes from natural catchments. Sources include surface water, groundwater and seawater (via desalination).
Public access to these areas is typically limited to preserve optimal water quality.
Filtration and purification of water occurs naturally in catchments as it passes through soil, sediments, rocks and vegetation.
But catchment water is subject to further treatment via standard processes that typically focus on:
- removing particulates (for example, soil and sediment)
- filtration (to remove particles and their contaminants)
- disinfection (for example, using chlorine and chloramine to kill bacteria and viruses)
- adding fluoride to prevent tooth decay
- adjusting pH to balance the chemistry of the water and to aid filtration.
This water is delivered to our taps via a reticulated system – a network of underground reservoirs, pipes, pumps and fittings.
In areas where there is no reticulated system, drinking water can also be sourced from rainwater tanks. This means the quality of drinking water can vary.
Sources of contamination can come from roof catchments feeding rainwater tanks as well from the tap due to lead in plumbing fittings and materials.
So, does all water meet these standards?
Some rural and remote areas, especially First Nations communities, rely on poor-quality surface water and groundwater for their drinking water.
Rural and regional water can exceed recommended guidelines for salt, microbial contaminants and trace elements, such as lead, manganese and arsenic.
The federal government and other agencies are trying to address this.
There are many impacts of poor regional water quality. These include its implication in elevated rates of tooth decay in First Nations people. This occurs when access to chilled, sugary drinks is cheaper and easier than access to good quality water.
What about PFAS?
There is also renewed concern about the presence of PFAS or “forever” chemicals in drinking water.
Recent research examining the toxicity of PFAS chemicals along with their presence in some drinking water catchments in Australia and overseas has prompted a recent assessment of water source contamination.
A review by the National Health and Medical Research Council (NHMRC) proposed lowering the limits for four PFAS chemicals in drinking water: PFOA, PFOS, PFHxS and PFBS.
The review used publicly available data and found most drinking water supplies are currently below the proposed new guideline values for PFAS.
However, “hotspots” of PFAS remain where drinking water catchments or other sources (for example, groundwater) have been impacted by activities where PFAS has been used in industrial applications. And some communities have voiced concerns about an association between elevated PFAS levels in their communities and cancer clusters.
While some PFAS has been identified as carcinogenic, it’s not certain that PFAS causes cancer. The link is still being debated.
Importantly, assessment of exposure levels from all sources in the population shows PFAS levels are falling meaning any exposure risk has also reduced over time.
How about removing PFAS from water?
Most sources of drinking water are not associated with industrial contaminants like PFAS. So water sources are generally not subject to expensive treatment processes, like reverse osmosis, that can remove most waterborne pollutants, including PFAS. These treatments are energy-intensive and expensive and based on recent water quality assessments by the NHMRC will not be needed.
While contaminants are everywhere, it is the dose that makes the poison. Ultra-low concentrations of chemicals including PFAS, while not desirable, may not be harmful and total removal is not warranted.
Mark Patrick Taylor, Chief Environmental Scientist, EPA Victoria; Honorary Professor, School of Natural Sciences, Macquarie University; Antti Mikkonen, Principal Health Risk Advisor – Chemicals, EPA Victoria, and PhD graduate, School of Pharmacy and Medical Sciences, University of South Australia, and Minna Saaristo, Research Affiliate in the School of Biological Sciences, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
7 Healthy Gut Habits For Women Over 40 – by Lara West
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
With regard to the titular 7 healthy gut habits for women over 40, a chapter is devoted to each one of those habits, and she goes into quite some detail in each category, more than you might expect.
As for the 7 things, we’ll not keep them a mystery; they are:
- Intermittent fasting
- Prebiotics & probiotics
- Mindful eating
- Understanding ingredients
- Movement
- Sleep
- Stress management
Of course, all of these things are good regardless of one’s age or gender, but West is writing with women over 40 in mind, and as such, she will focus on things that are especially relevant to those of us who are indeed women over 40.
You may be wondering: what if I’m a long way over 40, and menopause is a distant memory? In that case, 90% of this will still be relevant to you; the only parts that won’t be, are those that pertain specifically to the menopausal transitional phase itself, rather than the post-menopause state.
You may also be wondering: what if I’m a man, and menopause is just not in the cards for me? In that case, maybe about 70% of this will still be relevant to you, because of the broad applicability of most of the advice. That said, if it’s just for yourself, you’d probably do better with a book of which 100% is relevant to you, rather than this one.
The style is conversational pop-science, with personal anecdotes mixed in with references to science. It’s definitely on the light/easy-reading end of books that we’ve reviewed on the topic.
Bottom line: if you’re a woman over 40 who would like to improve your gut health, this book was written for you.
Click here to check out 7 Healthy Gut Habits For Women Over 40, and rediscover vitality!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
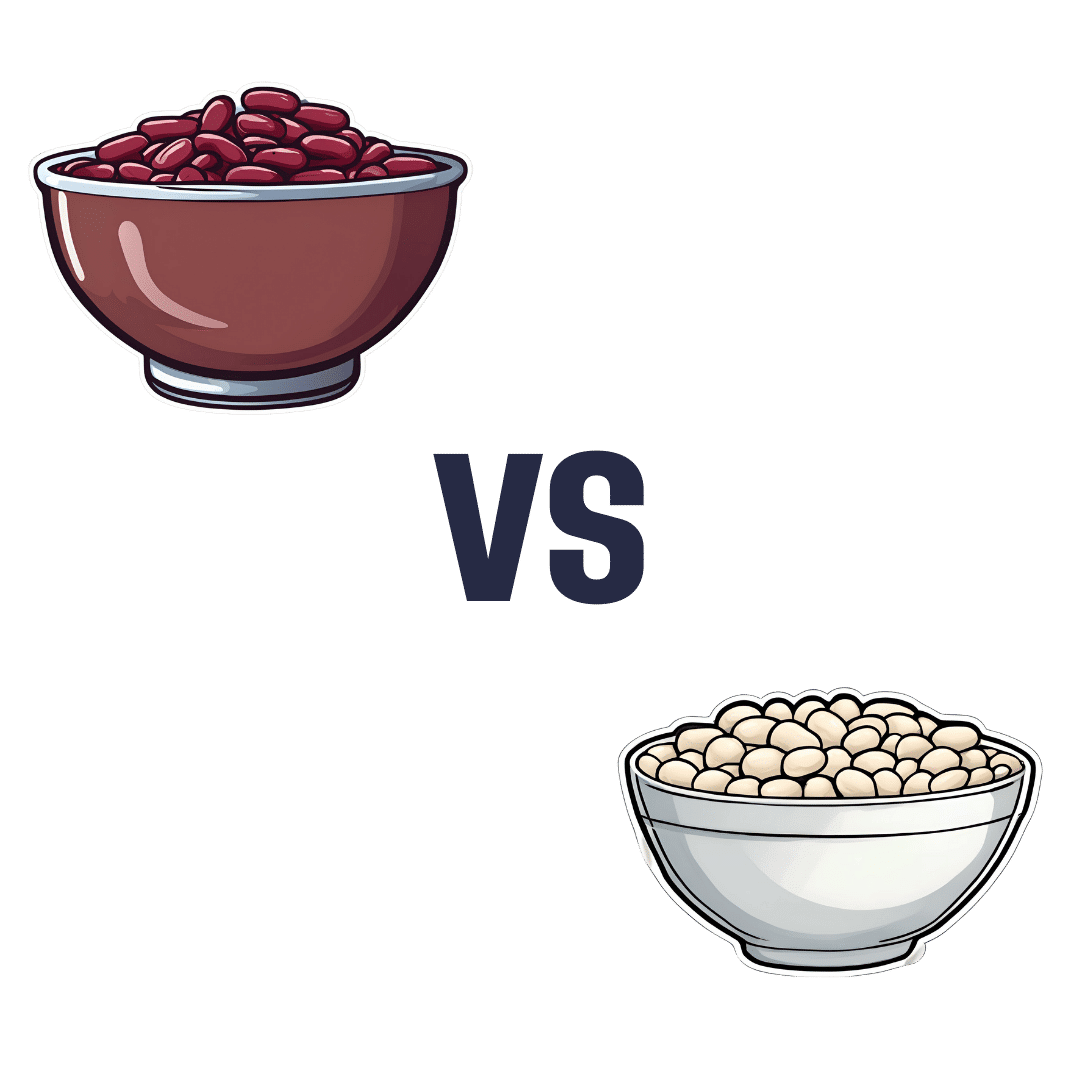
Kidney Beans vs White Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kidney beans to white beans, we picked the white.
Why?
It was close, and each has its strengths! Bear in mind, these are very closely-related beans. But as we say, there are distinguishing factors…
In terms of macros, kidney beans have very slightly more fiber and white beans have very slightly more protein. But both are close enough in both of those things to call this a tie in this category.
When it comes to vitamins, there are two ways of looking at this:
- kidney beans have more of vitamins B1, B2, B3, B6, B9, C, and K, while white beans have more vitamin B5, E, and choline
- kidney beans have slightly more of some vitamins that don’t usually see a deficiency, while white beans have 31x more vitamin E
Nevertheless, we’re sticking by our usual method of noting that this is a 7:3 win for kidney beans in this category; we just wanted to note that in practical health terms, an argument can be made for white beans on the vitamin front too.
In the category of minerals, kidney beans have slightly more phosphorus, while white beans have more calcium, copper, iron, magnesium, manganese, potassium, selenium, and zinc. An easy win for white beans this time.
(In case you’re wondering about the margin on phosphorus, it was 0.2x more, so we’re not seeing a situation like white beans’ 31x more vitamin E)
In short: both are great and both have their strengths. Enjoy both, together if you like! But if we have to pick one, we’re going with white beans.
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Science of Stretch – by Dr. Leada Malek
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is part of a “Science of…” series, of which we’ve reviewed some others before (Yoga | HIIT | Pilates), and needless to say, we like them.
You may be wondering: is this just that thing where a brand releases the same content under multiple names to get more sales, and no, it’s not (long-time 10almonds readers will know: if it were, we’d say so!).
While flexibility and mobility are indeed key benefits in yoga and Pilates, they looked into the science of what was going on in yoga asanas and Pilates exercises, stretchy or otherwise, so the stretching element was not nearly so deep as in this book.
In this one, Dr. Malek takes us on a wonderful tour of (relevant) human anatomy and physiology, far deeper than most pop-science books go into when it comes to stretching, so that the reader can really understand every aspect of what’s going on in there.
This is important, because it means busting a lot of myths (instead of busting tendons and ligaments and things), understanding why certain things work and (critically!) why certain things don’t, how certain stretching practices will sabotage our progress, things like that.
It’s also beautifully clearly illustrated! The cover art is a fair representation of the illustrations inside.
Bottom line: if you want to get serious about stretching, this is a top-tier book and you won’t regret it.
Click here to check out Science of Stretching, and learn what you can do and how!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: