How To Know When You’re Healing Emotionally
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The healing process can be humbling but rewarding, leading to deep fulfillment and inner peace. Discomfort in healing can be part of growth and self-integration. Because of that, progress sometimes looks and/or feels like progress… And sometimes it doesn’t. Here’s how to recognize it, though:
Small but important parts of a bigger process
Nine signs indicating you are healing:
- Allowing emotions: you acknowledge and process both negative and positive emotions instead of suppressing them.
- Improved boundaries: you improve at expressing and maintaining boundaries, overcoming fear of rejection, guilt, and shame.
- Acceptance of past: you accept difficult past experiences and their impact, reducing their hold over you.
- Less reactivity: you become less reactive and more thoughtful in responses, practicing emotional self-regulation.
- Non-linear healing: you understand that healing involves ups and downs and isn’t a straightforward journey.
- Stepping out of your comfort zone: you start taking brave steps that previously induced fear or anxiety.
- Handling disappointments: you accept setbacks and respond to them healthily, without losing motivation.
- Inner peace: you develop a sense of wholeness, and forgiveness for yourself and others, reducing self-sabotage.
- Welcoming support: you become more open to seeking and accepting help, moving beyond pride and shame.
In short: healing (especially the very first part: accepting that something needs healing) can be uncomfortable but lead to much better places in life. It’s okay if healing is slow; everyone’s journey is different, and doing your best is enough.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Why You Can’t Just “Get Over” Trauma
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why We’re Called “10almonds”, And Other Questions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Avid coffee drinker so very interested in the results Also question Is there something that you could take or eat that would prevent the caffeine from stimulating the kidneys? I tried to drink decaf from morning to night not a good result! Thanks❞
That is a good question! The simple answer is “no” (but keep reading, because all is not lost)
There’s no way (that we yet know of) to proof the kidneys against the stimulating effect of caffeine. This is especially relevant because part of caffeine’s stimulating effect is noradrenergic, and that “ren” in the middle there? It’s about the kidneys. This is just because the adrenal gland is situated next to them (actually, it’s pretty much sitting on top of them), hence the name, but it does mean that the kidneys are about the hardest thing in the body to have not affected by caffeine.
However! The effects of caffeine in general can be softened a little with l-theanine (found in tea, or it can be taken as a supplement). It doesn’t stop it from working, but it makes the curve of the effect a little gentler, and so it can reduce some unwanted side effects.
You can read more about l-theanine here:
❝How to jump start a inactive metabolism and keep it going? THANKYOU❞
The good news is, if you’re alive, your metabolism is active (it never stops!). So, it may just need perking up a little.
As for keeping it going, well, that’s what we’re here for! We’re all in favor of healthy longevity.
We’ll do a main feature soon on what we can do to influence our metabolism in either direction, but to give some quick notes here:
- A lot of our metabolism is influenced by genes and is unalterable (without modifying our genes, anyway)
- Metabolism isn’t just one thing—it’s many. And sometimes, parts of our metabolism can be much quicker or slower than others.
- When people talk about wanting a “faster metabolism”, they’re usually referring to fat-burning, and that’s just a small part of the picture, but we understand that it’s a focal point for many.
There really is enough material for a whole main feature on metabolic tweaks, though, so watch this space!
❝Why the name “10 Almonds?” Is this recommended by the Doctor? A daily dosage? And, if so, why? Thanks! Please answer me…I truly want to know!❞
Almonds are very nutritionally dense, and for example 20g of almonds (so, about 20 almonds) would give a 100% daily dose of zinc, amongst other nutrients.
We also do like to think that we give our readers an easily digestible dose of condensed “nutrition” in the form of health information.
However! That’s not actually the reason at all. It’s a reference to a viral Facebook hoax! There was a post going around that claimed:
❝HEADACHE REMEDY. Eat 10–12 almonds, the equivalent of two aspirins, next time you have a headache❞ ← not true!
It made us think about how much health-related disinformation there was circulating online! So, calling ourselves 10almonds was a bit of a nod to that story, but also a reminder to ourselves:
We must always publish information with good scientific evidence behind it!
Share This Post
-
Mental illness, psychiatric disorder or psychological problem. What should we call mental distress?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We talk about mental health more than ever, but the language we should use remains a vexed issue.
Should we call people who seek help patients, clients or consumers? Should we use “person-first” expressions such as person with autism or “identity-first” expressions like autistic person? Should we apply or avoid diagnostic labels?
These questions often stir up strong feelings. Some people feel that patient implies being passive and subordinate. Others think consumer is too transactional, as if seeking help is like buying a new refrigerator.
Advocates of person-first language argue people shouldn’t be defined by their conditions. Proponents of identity-first language counter that these conditions can be sources of meaning and belonging.
Avid users of diagnostic terms see them as useful descriptors. Critics worry that diagnostic labels can box people in and misrepresent their problems as pathologies.
Underlying many of these disagreements are concerns about stigma and the medicalisation of suffering. Ideally the language we use should not cast people who experience distress as defective or shameful, or frame everyday problems of living in psychiatric terms.
Our new research, published in the journal PLOS Mental Health, examines how the language of distress has evolved over nearly 80 years. Here’s what we found.
Engin Akyurt/Pexels Generic terms for the class of conditions
Generic terms – such as mental illness, psychiatric disorder or psychological problem – have largely escaped attention in debates about the language of mental ill health. These terms refer to mental health conditions as a class.
Many terms are currently in circulation, each an adjective followed by a noun. Popular adjectives include mental, mental health, psychiatric and psychological, and common nouns include condition, disease, disorder, disturbance, illness, and problem. Readers can encounter every combination.
These terms and their components differ in their connotations. Disease and illness sound the most medical, whereas condition, disturbance and problem need not relate to health. Mental implies a direct contrast with physical, whereas psychiatric implicates a medical specialty.
Mental health problem, a recently emerging term, is arguably the least pathologising. It implies that something is to be solved rather than treated, makes no direct reference to medicine, and carries the positive connotations of health rather than the negative connotation of illness or disease.
Is ‘mental health problem’ actually less pathologising? Monkey Business Images/Shutterstock Arguably, this development points to what cognitive scientist Steven Pinker calls the “euphemism treadmill”, the tendency for language to evolve new terms to escape (at least temporarily) the offensive connotations of those they replace.
English linguist Hazel Price argues that mental health has increasingly come to replace mental illness to avoid the stigma associated with that term.
How has usage changed over time?
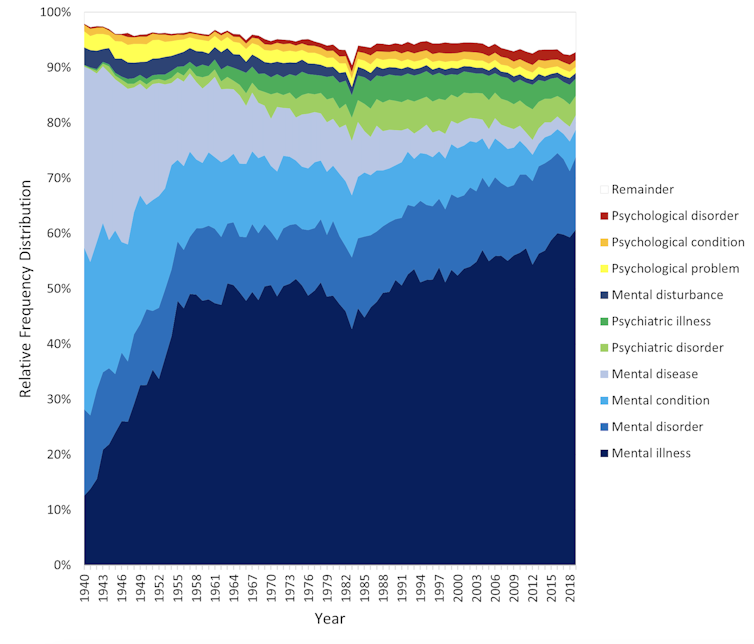
In the PLOS Mental Health paper, we examine historical changes in the popularity of 24 generic terms: every combination of the nouns and adjectives listed above.
We explore the frequency with which each term appears from 1940 to 2019 in two massive text data sets representing books in English and diverse American English sources, respectively. The findings are very similar in both data sets.
The figure presents the relative popularity of the top ten terms in the larger data set (Google Books). The 14 least popular terms are combined into the remainder.
Relative popularity of alternative generic terms in the Google Books corpus. Haslam et al., 2024, PLOS Mental Health. Several trends appear. Mental has consistently been the most popular adjective component of the generic terms. Mental health has become more popular in recent years but is still rarely used.
Among nouns, disease has become less widely used while illness has become dominant. Although disorder is the official term in psychiatric classifications, it has not been broadly adopted in public discourse.
Since 1940, mental illness has clearly become the preferred generic term. Although an assortment of alternatives have emerged, it has steadily risen in popularity.
Does it matter?
Our study documents striking shifts in the popularity of generic terms, but do these changes matter? The answer may be: not much.
One study found people think mental disorder, mental illness and mental health problem refer to essentially identical phenomena.
Other studies indicate that labelling a person as having a mental disease, mental disorder, mental health problem, mental illness or psychological disorder makes no difference to people’s attitudes toward them.
We don’t yet know if there are other implications of using different generic terms, but the evidence to date suggests they are minimal.
The labels we use may not have a big impact on levels of stigma. Pixabay/Pexels Is ‘distress’ any better?
Recently, some writers have promoted distress as an alternative to traditional generic terms. It lacks medical connotations and emphasises the person’s subjective experience rather than whether they fit an official diagnosis.
Distress appears 65 times in the 2022 Victorian Mental Health and Wellbeing Act, usually in the expression “mental illness or psychological distress”. By implication, distress is a broad concept akin to but not synonymous with mental ill health.
But is distress destigmatising, as it was intended to be? Apparently not. According to one study, it was more stigmatising than its alternatives. The term may turn us away from other people’s suffering by amplifying it.
So what should we call it?
Mental illness is easily the most popular generic term and its popularity has been rising. Research indicates different terms have little or no effect on stigma and some terms intended to destigmatise may backfire.
We suggest that mental illness should be embraced and the proliferation of alternative terms such as mental health problem, which breed confusion, should end.
Critics might argue mental illness imposes a medical frame. Philosopher Zsuzsanna Chappell disagrees. Illness, she argues, refers to subjective first-person experience, not to an objective, third-person pathology, like disease.
Properly understood, the concept of illness centres the individual and their connections. “When I identify my suffering as illness-like,” Chappell writes, “I wish to lay claim to a caring interpersonal relationship.”
As generic terms go, mental illness is a healthy option.
Nick Haslam, Professor of Psychology, The University of Melbourne and Naomi Baes, Researcher – Social Psychology/ Natural Language Processing, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
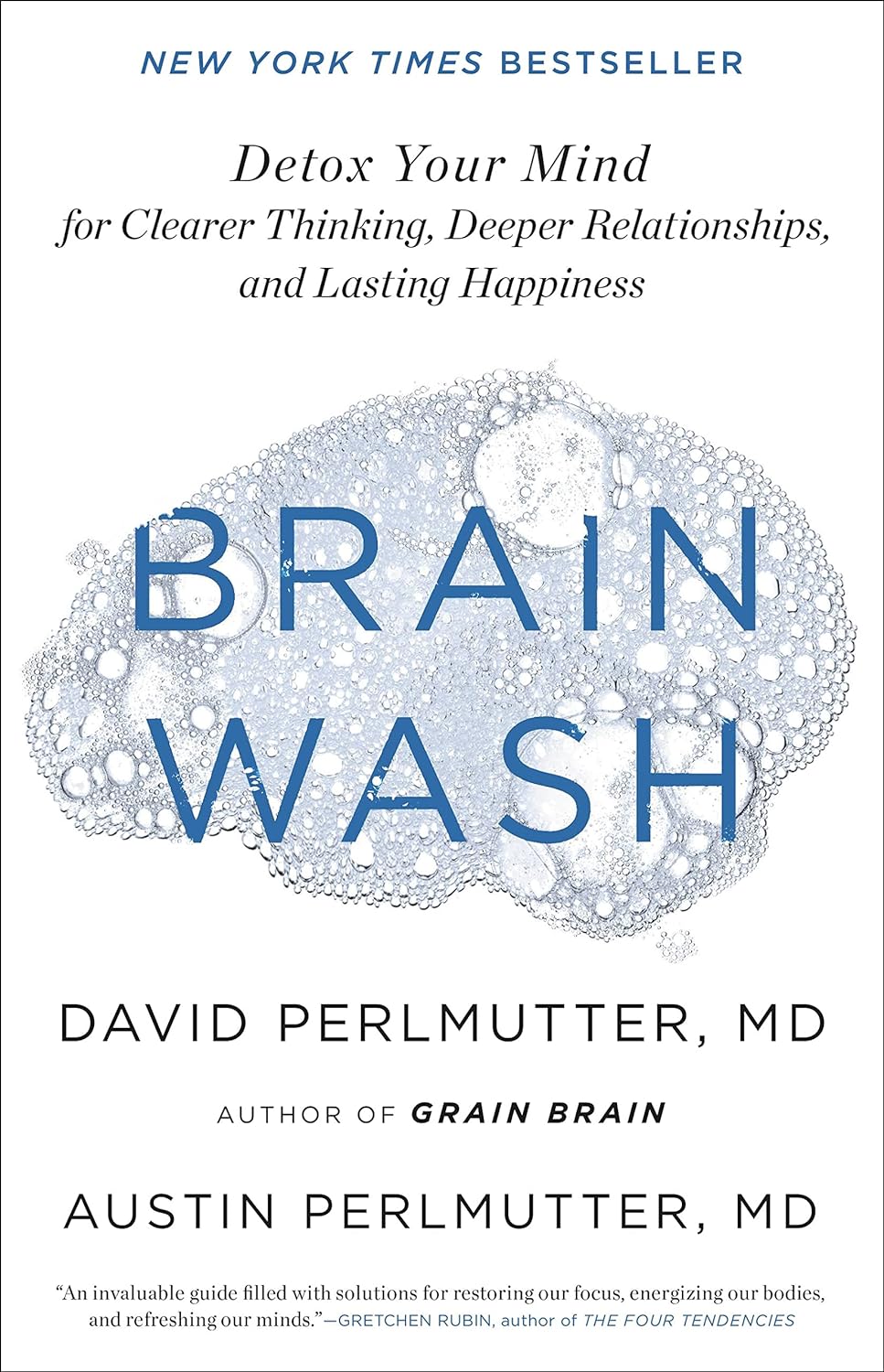
Brain Wash – by Dr. David Perlmutter, Dr. Austin Perlmutter, and Kristen Loberg
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be familiar with the lead author of this book, Dr. David Perlmutter, as a big name in the world of preventative healthcare. A lot of his work has focused specifically on carbohydrate metabolism, and he is as associated with grains and he is with brains. This book focuses on the latter.
Dr. Perlmutter et al. take a methodical look at all that is ailing our brains in this modern world, and systematically lay out a plan for improving each aspect.
The advice is far from just dietary, though the chapter on diet takes a clear stance:
❝The food you eat and the beverages you drink change your emotions, your thoughts, and the way you perceive the world❞
The style is explanatory, and the book can be read comfortably as a “sit down and read it cover to cover” book; it’s an enjoyable, informative, and useful read.
Bottom line: if you’d like to give your brain a gentle overhaul, this is the one-stop-shop book to give you the tools to do just that.
Share This Post
Related Posts
-
Cherries’ Very Healthy Wealth Of Benefits!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cherries’ Health Benefits Simply Pop
First, be aware, there are different kinds:
Sweet & Sour
Cherries can be divided into sweet vs sour. These are mostly nutritionally similar, though sour ones do have some extra benefits.
Sweet and sour cherries are closely related but botanically different plants; it’s not simply a matter of ripeness (or preparation).
These can mostly be sorted into varieties of Prunus avium and Prunus cerasus, respectively:
Cherry Antioxidants: From Farm to Table
Sour cherry varieties include morello and montmorency, so look out for those names in particular when doing your grocery-shopping.
You may remember that it’s a good rule of thumb that foods that are more “bitter, astringent, or pungent” will tend to have a higher polyphenol content (that’s good):
Enjoy Bitter Foods For Your Heart & Brain
Juiced up
Almost certainly for reasons of budget and convenience, as much as for standardization, most studies into the benefits of cherries have been conducted using concentrated cherry juice as a supplement.
At home, we need not worry so much about standardization, and our budget and convenience are ours to manage. To this end, as a general rule of thumb, whole fruits are pretty much always better than juice:
Which Sugars Are Healthier, And Which Are Just The Same?
Antioxidant & anti-inflammatory!
Cherries are a very good source of antioxidants, and as such they also reduce inflammation, which in turn means ameliorating autoimmune diseases, from common things like arthritis…
…to less common things like gout:
Cherry Consumption and the Risk of Recurrent Gout Attacks
This can also be measured by monitoring uric acid metabolites:
Consumption of cherries lowers plasma urate in healthy women
Anti-diabetic effect
Most of the studies on this have been rat studies, and the human studies have been less “the effect of cherry consumption on diabetes” and more a matter of separate studies adding up to this conclusion in, the manner of “cherries have this substance, this substance has this effect, therefore cherries will have this effect”. You can see an example of this discussed over the course of 15 studies, here:
A Review of the Health Benefits of Cherries ← skip to section 2.2.1: “Cherry Intake And Diabetes”
In short, the jury is out on cherry juice, but eating cherries themselves (much like getting plenty of fruit in general) is considered good against diabetes.
Good for healthy sleep
For this one, the juice suffices (actual cherries are still recommended, but the juice gave clear significant positive results):
Pilot Study of the Tart Cherry Juice for the Treatment of Insomnia and Investigation of Mechanisms ← this was specifically in people over the age of 50
Importantly, it’s not that cherries have a sedative effect, but rather they support the body’s ability to produce melatonin adequately when the time comes:
Effect of tart cherry juice (Prunus cerasus) on melatonin levels and enhanced sleep quality
Post-exercise recovery
Cherries are well-known for boosting post-exercise recovery, though they may actually improve performance during exercise too, if eaten beforehand/
For example, these marathon-runners who averaged 13% compared to placebo control:
As for its recovery benefits, we wrote about this before:
How To Speed Up Recovery After A Workout (According To Actual Science)
Want to get some?
We recommend your local supermarket (or farmer’s market!), but if for any reason you prefer to take a supplement, here’s an example product on Amazon
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Having dense breasts is linked to cancer. But advice about breast density can depend on where you live
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Having dense breasts is a clear risk factor for breast cancer. It can also make cancers hard to spot on mammograms.
Yet you might not be aware you have dense breasts, even after mammographic screening.
In Australia, advice for women with dense breasts and their health-care professionals can be inconsistent and confusing.
This is because there’s not currently consensus on whether women who have dense breasts, but no symptoms, benefit from further imaging such as ultrasounds. Concerns include potential cost of these tests and the risk they can produce false positives.
Gorodenkoff/Shutterstock What is breast density?
Breasts are made up of fatty tissue and fibroglandular tissue (including glands that make milk, held together by fibrous tissue).
On a mammogram – an x-ray of the breast – fibroglandular tissue appears white and fatty tissue appears dark. The white areas are referred to as breast density.
Fibroglandular tissue shows up white on a mammogram. Nata Sokhrannova/Shutterstock A higher proportion of fibroglandular tissue means your breasts are dense.
There are four categories to classify breast density:
- A: almost entirely fatty
- B: scattered areas of fibroglandular density
- C: heterogeneously or consistently dense
- D: extremely dense.
Breast density is very common. Around 40% of women aged 40–74 are estimated to have “dense breasts”, meaning they fall in category C or D.
What’s the link to cancer?
Breast density is associated with the risk of breast cancer in two ways.
First, breast density usually decreases with age. But if a woman has high breast density for her age, it increases her likelihood of breast cancer.
One study looked at the risk of breast cancer over the age of 50. It found there was a 6.2% risk for the one-third of women with the lowest density. For the 5% with the highest density, the risk was 14.7%.
Second, breast density “masks” cancers if they develop. Both cancers and breast density appear white on a mammogram, making cancers very hard to see.
Breast cancer screening saves lives through early detection and improved treatment options. But we don’t yet know if telling women about their breast density leads to earlier cancer detection, or lives saved.
In Australia, screening mammography is free for all women* aged 40 and older. This is run through BreastScreen Australia, a joint national, state and territory initiative. Those aged 50-74 are invited to have a mammogram, but it’s available for free without a referral from age 40.
However, the messages Australian women currently receive about breast density – and whether it’s recorded – depends on where they live.
What does the advice say?
In 2023, the Royal Australian and New Zealand College of Radiologists updated its position statement to recommend breast density is recorded during screening and diagnostic tests in Australia and New Zealand.
Meanwhile BreastScreen Australia says it “should not routinely record breast density or provide supplemental testing for women with dense breasts”. However this position statement is from 2020 and is currently under review.
Some state and territory BreastScreen programs, including in Western Australia, South Australia and soon Victoria, notify women if they have dense breasts. Victoria is currently at an early stage of its roll-out.
While the messaging regarding breast density differs by state, none currently recommend further imaging for women with dense breasts without speaking to a doctor about individual risk.
What are the issues?
Providing recommendations for women with dense breasts is difficult.
The European Society of Breast Imaging recommends women with extremely dense breasts aged 50–70 receive an MRI every two to four years, in addition to screening mammography. This is based on a large randomised controlled trial from the Netherlands.
But the Royal Australian and New Zealand College of Radiologists describes this recommendation as “aspirational”, acknowledging cost, staffing and accessibility as challenges.
That is, it is not feasible to provide a supplemental MRI for everyone in the screening population in category D with extremely dense breasts (around 10%).
Further, there is no consensus on appropriate screening recommendations for women in the category C (heterogeneous density).
We need a national approach to breast density reporting in Australia and to do better at identifying who is most likely to benefit from further testing.
BreastScreen Australia is currently undergoing a review of its policy and funding.
One of its goals is to enable a nationally consistent approach to breast screening practices. Hopefully breast density reporting, including funding to support national implementation, will be a priority.
*This includes those recorded female at birth and who are gender diverse.
Jennifer Stone, Principal Research Fellow, School of Population and Global Health, The University of Western Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Sea Salt vs MSG – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sea salt to MSG, we picked the MSG.
Why?
Surprise! Or maybe not? The results of the poll for this one should be interesting, and will help us know whether we need to keep mentioning in every second recipe that MSG is a healthier alternative to salt.
First of all, two things:
- Don’t be fooled by their respective names, and/or with such, an appeal to naturalism. For example, hydroxybenzoic acids are a major group of beneficial phenolic compounds, whereas hemlock is a wildflower that grows in this writer’s garden and will kill you if you eat it. Actually hydroxybenzoic acids also grow here (on the apple tree), but that’s not the point. The point is: worry less about names, and more about evidence!
- Don’t be fooled by the packaging. A lot of products go for “greenwashing” of one kind or another. You’re not eating the packaging (hopefully), so don’t be swayed by a graphic designer’s implementation of a marketing team’s aesthetic choices.
If naturalism is for some reason very important to you though, do bear in mind that glutamates occur generously in many common foodstuffs (tomatoes are a fine, healthy example) and eating tomato in the presence of salt will have the same biochemical effect as eating MSG, because it’s the same chemicals.
Since there are bad rumors about MSG’s safety, especially in the US where there is often a strong distrust of anything associated with China (actually MSG was first isolated in Japan, more than 100 years ago, by Japanese biochemist Dr. Kikunae Ikeda, but that gets drowned out by the “Chinese Restaurant Syndrome” fear in the US), know that this has resulted in MSG being one of the most-studied food additives in the last 40 years or so, with many teams of scientists trying to determine its risks and not finding any (aside from the same that could be said of any substance; anything in sufficient excess will kill you, including water or oxygen).
Well, that’s all been about safety, but what makes it healthier than sea salt?
Simply, it has about ⅓ of the sodium content, that’s all. So, if you are laboring all day in a field under the hot summer sun, then probably the sea salt will be healthier, to replenish more of the sodium you lost through sweat. But for most people most of the time, having less sodium rather than more is the healthier option.
Want to learn more?
You might like to read:
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
- MSG vs. Salt: Sodium Comparison ← here be chemistry
- More Salt, Not Less? ← No
- Pink Himalayan Salt: Health Facts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: