How To Eat To Lose Belly Fat (3 Stages)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Belly fat is easier to gain than it is to lose, and it’s absolutely something that needs more attention in the kitchen than in the gym. Here’s one way of doing it:
By the numbers
First note: this video is by a man, and judging by the numbers mentioned, assumes that the viewer is also a man. An end goal of 10% body fat is a little on the low side for men, and would be dangerous for women. The magic 15% mark that he mentions as being a point where various metabolic things change, is more like 20% for women. All assuming normal hormones, of course, since it is hormones that direct this.
Healthy body fat percentages are (assuming normal hormones) in the range of 20–25% for women and 15–20% for men.
With that in mind…
The idea of this approach is to lose enough weight that your body gets rid of even the most awkward bits (e.g: visceral belly fat, which will often be the last to get used) before, if desired, then maintaining at a slightly higher body fat percentage.
- Stage 1: count calories (we don’t usually recommend this at 10almonds, but he does, so we’re reporting it here) and use your weight in pounds multiplied by 12 to give your daily calorie target. Make the majority of your diet foods that have a large volume:calorie ratio, such as fruits and vegetables, in order to feel full without overloading your metabolism. He has an interesting method of calculating a protein target; instead of the usual “1g/kg of body weight”, he says 1g per cm of height. Doing this consistently should get you to 15% body fat (so, 20%, for women).
- Stage 2: start counting fat intake too, and aim for 20–25% of your daily calories as fat. Continue, aside from that, with what you were doing in Stage 1. Doing this consistently should get you to 12% body fat (so, about 17%, for women). Being under the usual healthy level for a while should allow your body to start getting rid of visceral fat.
- Stage 3: track everything, levelling up your precision (no more “this little thing doesn’t count”), and planning ahead when it comes to social events etc. Doing this consistently should yet you to 10% body fat (so, about 15%, for women). This stage has a good chance of making most people miserable, so if that happens, consider the benefits of going back to the healthier 15% body fat (men) or 20% (women).
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Visceral Belly Fat & How To Lose It ← without calorie-counting! We prefer this 😉
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Stress Affects Your Body
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Sharon Bergquist gives us a tour:
Stress, from the inside out
Stress is a natural physical and emotional response to challenges or being overwhelmed. It can be beneficial in short-term situations (e.g. escape from a tiger) but is harmful when prolonged or frequent (e.g. escape the rat-race).
Immediate physiological response: cortisol, adrenaline (epinephrine), and norepinephrine are released by the adrenal glands.
The effects this has (non-exhaustive list; we’re just citing what’s in the video here):
- Cortisol impairs blood vessel function, promoting atherosclerosis.
- Adrenaline increases heart rate and blood pressure, leading to hypertension.
- Stress disrupts the brain-gut connection, causing:
- Digestive issues like irritable bowel syndrome and heartburn.
- Changes in gut bacteria composition, potentially affecting overall health.
- Cortisol increases appetite and cravings for energy-dense “comfort foods”.
- This in turn promotes visceral fat storage, which raises the risk of heart disease and insulin resistance.
- Immune-specific effects:
- Stress hormones initially aid in healing and immune defense.
- Chronic stress weakens immune function (by over-working it constantly), increasing susceptibility to infections and slowing recovery.
- Other systemic effects:
- Chronic stress shortens telomeres, which protect chromosomes. Shortened telomeres accelerate cellular aging.
- Chronic stress can also cause acne, hair loss, sexual dysfunction, headaches, muscle tension, fatigue, irritability, and difficulty concentrating.
So, how to manage this? The video says that viewing stressful situations as controllable challenges, rather than insurmountable threats, leads to better short-term performance and long-term health.
Which would be wonderful, except that usually things are stressful precisely because they are not entirely within the field of our control, and the usual advice is to tend to what we can control, and accept what we can’t.
However… That paradigm still leaves out the very big set of “this might be somewhat within our control or it might not; we really don’t know yet; we can probably impact it but what if we don’t do enough, or take the wrong approach and do the wrong thing? And also we have 17 competing stressors, which ones should we prioritize tending to first, and…” and so on.
To that end, we suggest checking out the “Want to learn more?” link we drop below the video today, as it is about managing stress realistically, in a world that, if we’re honest about it, can sometimes be frankly unmanageable.
Meanwhile, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Heart Health vs Systemic Stress ← this is good in and of itself, and also links to other stress-related resources of ours
Take care!
Share This Post
-
Uric Acid’s Extensive Health Impact (And How To Lower It)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Uric Acid’s Extensive Health Impact (And How To Lower It)
This is Dr. David Perlmutter. He’s a medical doctor, and a Fellow of the American College of Nutrition. He’s a member of the Editorial Board for the Journal of Alzheimer’s Disease, and has been widely published in many other peer-reviewed journals.
What does he want us to know?
He wants us to know about the health risks of uric acid (not something popularly talked about so much!), and how to reduce it.
First: what is it? Uric acid is a substance we make in our own body. However, unlike most substances we make in our body, we have negligible use for it—it’s largely a waste product, usually excreted in urine.
However, if we get too much, it can build up (and crystallize), becoming such things as kidney stones, or causing painful inflammation if it shows up in the joints, as in gout.
More seriously (unpleasant as kidney stones and gout may be), this inflammation can have a knock-on effect triggering (or worsening) other inflammatory conditions, ranging from non-alcoholic fatty liver disease, to arthritis, to dementia, and even heart problems. See for example:
- David Perlmutter | Uric Acid and Cognitive Decline
- American Heart Association | Uric acid linked to later risk for irregular heart rhythm
- World Journal of Gastroenterology | The role of uric acid in non-alcoholic steatohepatitis development
How can we reduce our uric acid levels?
Uric acid is produced when we metabolize purine nucleotides, which are found in many kinds of food. We can therefore reduce our uric acid levels by reducing our purine intake, as well as things that mess up our liver’s ability to detoxify things. Offsetting the values for confounding variables (such as fiber content, or phytochemicals that mitigate the harm), the worst offenders include…
Liver-debilitating things:
- Alcohol (especially beer)
- High-fructose corn syrup (and other fructose-containing things that aren’t actual fruit)
- Other refined sugars
- Wheat / white flour products (this is why beer is worse than wine, for example; it’s a double-vector hit)
Purine-rich things:
- Red meats and game
- Organ meats
- Oily fish, and seafood (great for some things; not great for this)
Some beans and legumes are also high in purines, but much like real fruit has a neutral or positive effect on blood sugar health despite its fructose content, the beans and legumes that are high in purines, also contain phytochemicals that help lower uric acid levels, so have a beneficial effect.
Eggs (consumed in moderation) and tart cherries have a uric-acid lowering effect.
Water is important for all aspects of health, and doubly important for this.
Hydrate well!
Lifestyle matters beyond diet
The main key here is metabolic health, so Dr. Perlmutter advises the uncontroversial lifestyle choices of moderate exercise and good sleep, as well as (more critically) intermittent fasting. We wrote previously on other things that can benefit liver health:
…in this case, that means the liver gets a break to recuperate (something it’s very good at, but does need to get a chance to do), which means that while you’re not giving it something new to do, it can quickly catch up on any backlog, and then tackle any new things fresh, next time you start eating.
Want to know more about this from Dr. Perlmutter?
You might like his article:
An Integrated Plan for Lowering Uric Acid ← more than we had room for here; he also talks about extra things to include in your diet/supplementation regime for beneficial effects!
And/or his book:
…on which much of today’s main feature was based.
Take care!
Share This Post
-
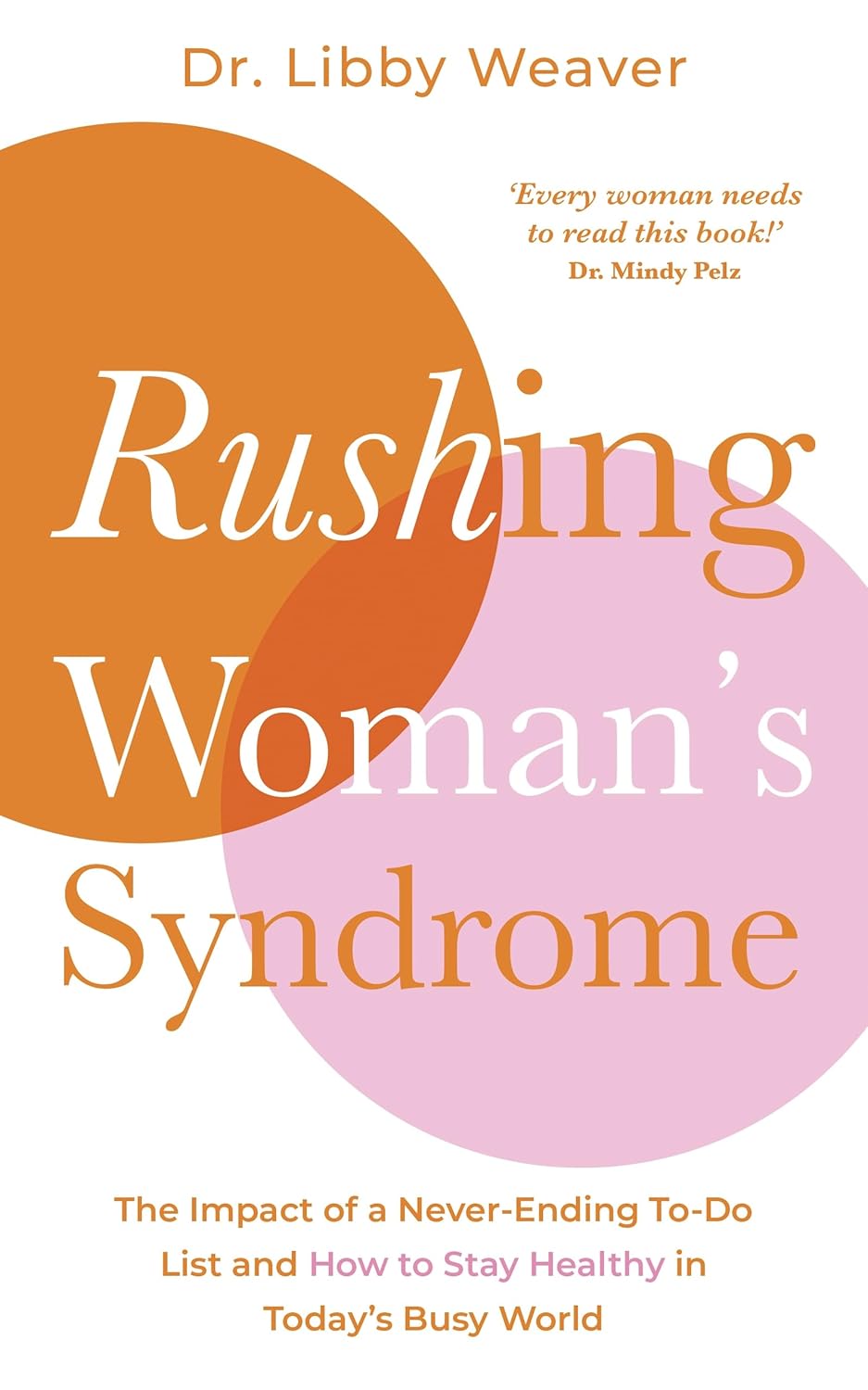
Rushing Woman’s Syndrome – by Dr. Libby Weaver
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s well-known that very many women suffer from “the triple burden” of professional work, housework, and childcare. And it’s not even necessarily that we resent any of those things or feel like they’re a burden; we (hopefully) love our professions, homes, children. But, here’s the thing: no amount of love will add extra hours to the day!
On the psychological level, a lot is about making more conscious decisions and fewer automatic reactions. For example, everyone wants everything from us right now, if not by yesterday, but when do they need it? And, is it even our responsibility? Not everything is, and many of us take on more than we should in our effort to be “enough”.
On the physical level, she covers hormones, including the menstrual/menopausal and the metabolic, as well as liver health, digestive issues, and sleep.
The style is direct and friendly, making frequent references to science but not getting deep into it.
It’s worth noting that while she acknowledges other demographics exist, she’s writing mainly for an audience of otherwise healthy straight white women with children and at least moderate financial resources, so if you fall outside of those things, there may be things that society will penalize you for and expect more from you in return for less, so that is a limitation of the book.
Bottom line: if the above describes you, you will probably get value out of this book.
Click here to check out Rushing Woman’s Syndrome, and take care of yourself too!
Share This Post
Related Posts
-
Reclaiming Body Trust – by Hilary Kinavey & Dana Sturtevant
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Authored by a therapist and a dietician, this book draws from both of their extensive professional clinical experiences, to explore how we can (often early in our lives) be led into disordered thinking when it comes to food and our bodies, and how we can “take back that which has been stolen from us”.
More prosaically: the presented goal here is for us to each figure out where we are with our own body, and how we might build our relationship with same going forwards, in the way that will work the best for us.
The style is relaxed and conversational, while taking care to cover topics that are often tricky with no less seriousness. Chapter headings such as “Your coping is rooted in wisdom”, “What does grief have to do with it?” and “Allowing for pleasure and satisfaction” give an idea of the flavors at hand here.
Bottom line: if you think your relationship with food and your body could be better, not only are you probably right, but also, this book can help.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Her Mental Health Treatment Was Helping. That’s Why Insurance Cut Off Her Coverage.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Reporting Highlights
- Progress Denials: Insurers use a patient’s improvement to justify denying mental health coverage.
- Providers Disagree: Therapists argue with insurers and the doctors they employ to continue covering treatment for their patients.
- Patient Harm: Some patients backslid when insurers cut off coverage for treatment at key moments.
These highlights were written by the reporters and editors who worked on this story.
Geneva Moore’s therapist pulled out her spiral notebook. At the top of the page, she jotted down the date, Jan. 30, 2024, Moore’s initials and the name of the doctor from the insurance company to whom she’d be making her case.
She had only one chance to persuade him, and by extension Blue Cross and Blue Shield of Texas, to continue covering intensive outpatient care for Moore, a patient she had come to know well over the past few months.
The therapist, who spoke on the condition of anonymity out of fear of retaliation from insurers, spent the next three hours cramming, as if she were studying for a big exam. She combed through Moore’s weekly suicide and depression assessments, group therapy notes and write-ups from their past few sessions together.
She filled two pages with her notes: Moore had suicidal thoughts almost every day and a plan for how she would take her own life. Even though she expressed a desire to stop cutting her wrists, she still did as often as three times a week to feel the release of pain. She only had a small group of family and friends to offer support. And she was just beginning to deal with her grief and trauma over sexual and emotional abuse, but she had no healthy coping skills.
Less than two weeks earlier, the therapist’s supervisor had struck out with another BCBS doctor. During that call, the insurance company psychiatrist concluded Moore had shown enough improvement that she no longer needed intensive treatment. “You have made progress,” the denial letter from BCBS Texas read.
When the therapist finally got on the phone with a second insurance company doctor, she spoke as fast as she could to get across as many of her points as possible.
“The biggest concern was the abnormal thoughts — the suicidal ideation, self-harm urges — and extensive trauma history,” the therapist recalled in an interview with ProPublica. “I was really trying to emphasize that those urges were present, and they were consistent.”
She told the company doctor that if Moore could continue on her treatment plan, she would likely be able to leave the program in 10 weeks. If not, her recovery could be derailed.
The doctor wasn’t convinced. He told the therapist that he would be upholding the initial denial. Internal notes from the BCBS Texas doctors say that Moore exhibited “an absence of suicidal thoughts,” her symptoms had “stabilized” and she could “participate in a lower level of care.”
The call lasted just seven minutes.
Moore was sitting in her car during her lunch break when her therapist called to give her the news. She was shocked and had to pull herself together to resume her shift as a technician at a veterinary clinic.
“The fact that it was effective immediately,” Moore said later, “I think that was the hardest blow of it all.”
Many Americans must rely on insurers when they or family members are in need of higher-touch mental health treatment, such as intensive outpatient programs or round-the-clock care in a residential facility. The costs are high, and the stakes for patients often are, too. In 2019 alone, the U.S. spent more than $106.5 billion treating adults with mental illness, of which private insurance paid about a third. One 2024 study found that the average quoted cost for a month at a residential addiction treatment facility for adolescents was more than $26,000.
Health insurers frequently review patients’ progress to see if they can be moved down to a lower — and almost always cheaper — level of care. That can cut both ways. They sometimes cite a lack of progress as a reason to deny coverage, labeling patients’ conditions as chronic and asserting that they have reached their baseline level of functioning. And if they make progress, which would normally be celebrated, insurers have used that against patients to argue they no longer need the care being provided.
Their doctors are left to walk a tightrope trying to convince insurers that patients are making enough progress to stay in treatment as long as they actually need it, but not so much that the companies prematurely cut them off from care. And when insurers demand that providers spend their time justifying care, it takes them away from their patients.
“The issues that we grapple with are in the real world,” said Dr. Robert Trestman, the chair of psychiatry and behavioral medicine at the Virginia Tech Carilion School of Medicine and chair of the American Psychiatric Association’s Council on Healthcare Systems and Financing. “People are sicker with more complex conditions.”
Mental health care can be particularly prone to these progress-based denials. While certain tests reveal when cancer cells are no longer present and X-rays show when bones have healed, psychiatrists say they have to determine whether someone has returned to a certain level of functioning before they can end or change their treatment. That can be particularly tricky when dealing with mental illness, which can be fluid, with a patient improving slightly one day only to worsen the next.
Though there is no way to know how often coverage gets cut off mid-treatment, ProPublica has found scores of lawsuits over the past decade in which judges have sharply criticized insurance companies for citing a patient’s improvement to deny mental health coverage. In a number of those cases, federal courts ruled that the insurance companies had broken a federal law designed to provide protections for people who get health insurance through their jobs.
Reporters reviewed thousands of pages of court documents and interviewed more than 50 insiders, lawyers, patients and providers. Over and over, people said these denials can lead to real — sometimes devastating — harm. An official at an Illinois facility with intensive mental health programs said that this past year, two patients who left before their clinicians felt they were ready due to insurance denials had attempted suicide.
Dr. Eric Plakun, a Massachusetts psychiatrist with more than 40 years of experience in residential and intensive outpatient programs, and a former board member of the American Psychiatric Association, said the “proprietary standards” insurers use as a basis for denying coverage often simply stabilize patients in crisis and “shortcut real treatment.”
Plakun offered an analogy: If someone’s house is on fire, he said, putting out the fire doesn’t restore the house. “I got a hole in the roof, and the windows have been smashed in, and all the furniture is charred, and nothing’s working electrically,” he said. “How do we achieve recovery? How do we get back to living in that home?”
Unable to pay the $350-a-day out-of-pocket cost for additional intensive outpatient treatment, Moore left her program within a week of BCBS Texas’ denial. The insurer would only cover outpatient talk therapy.
During her final day at the program, records show, Moore’s suicidal thoughts and intent to carry them out had escalated from a 7 to a 10 on a 1-to-10 scale. She was barely eating or sleeping.
A few hours after the session, Moore drove herself to a hospital and was admitted to the emergency room, accelerating a downward spiral that would eventually cost the insurer tens of thousands of dollars, more than the cost of the treatment she initially requested.
How Insurers Justify Denials
Buried in the denial letters that insurance companies send patients are a variety of expressions that convey the same idea: Improvement is a reason to deny coverage.
“You are better.” “Your child has made progress.” “You have improved.”
In one instance, a doctor working for Regence Blue Cross and Blue Shield of Oregon wrote that a patient who had been diagnosed with major depression was “sufficiently stable,” even as her own doctors wrote that she “continued to display a pattern of severe impairment” and needed round-the-clock care. A judge ruled that “a preponderance of the evidence” demonstrated that the teen’s continued residential treatment was medically necessary. The insurer said it can’t comment on the case because it ended with a confidential settlement.
In another, a doctor working for UnitedHealth Group wrote in 2019 that a teenage girl with a history of major depression who had been hospitalized after trying to take her own life by overdosing “was doing better.” The insurer denied ongoing coverage at a residential treatment facility. A judge ruled that the insurer’s determination “lacked any reasoning or citations” from the girl’s medical records and found that the insurer violated federal law. United did not comment on this case but previously argued that the girl no longer had “concerning medical issues” and didn’t need treatment in a 24-hour monitored setting.
To justify denials, the insurers cite guidelines that they use to determine how well a patient is doing and, ultimately, whether to continue paying for care. Companies, including United, have said these guidelines are independent, widely accepted and evidence-based.
Insurers most often turn to two sets: MCG (formerly known as Milliman Care Guidelines), developed by a division of the multibillion-dollar media and information company Hearst, and InterQual, produced by a unit of UnitedHealth’s mental health division, Optum. Insurers have also used guidelines they have developed themselves.
MCG Health did not respond to multiple requests for comment. A spokesperson for the Optum division that works on the InterQual guidelines said that the criteria “is a collection of established scientific evidence and medical practice intended for use as a first level screening tool” and “helps to move patients safely and efficiently through the continuum of care.”
A separate spokesperson for Optum also said the company’s “priority is ensuring the people we serve receive safe and effective care for their individual needs.” A Regence spokesperson said that the company does “not make coverage decisions based on cost or length of stay,” and that its “number one priority is to ensure our members have access to the care they need when they need it.”
In interviews, several current and former insurance employees from multiple companies said that they were required to prioritize the proprietary guidelines their company used, even if their own clinical judgment pointed in the opposite direction.
“It’s very hard when you come up against all these rules that are kind of setting you up to fail the patient,” said Brittainy Lindsey, a licensed mental health counselor who worked at the Anthem subsidiary Beacon and at Humana for a total of six years before leaving the industry in 2022. In her role, Lindsey said, she would suggest approving or denying coverage, which — for the latter — required a staff doctor’s sign-off. She is now a mental health consultant for behavioral health businesses and clinicians.
A spokesperson for Elevance Health, formerly known as Anthem, said Lindsey’s “recollection is inaccurate, both in terms of the processes that were in place when she was a Beacon employee, and how we operate today.” The spokesperson said “clinical judgment by a physician — which Ms. Lindsey was not — always takes precedence over guidelines.”
In an emailed statement, a Humana spokesperson said the company’s clinician reviewers “are essential to evaluating the facts and circumstances of each case.” But, the spokesperson said, “having objective criteria is also important to provide checks and balances and consistently comply with” federal requirements.
The guidelines are a pillar of the health insurance system known as utilization management, which paves the way for coverage denials. The process involves reviewing patients’ cases against relevant criteria every handful of days or so to assess if the company will continue paying for treatment, requiring providers and patients to repeatedly defend the need for ongoing care.
Federal judges have criticized insurance company doctors for using such guidelines in cases where they were not actually relevant to the treatment being requested or for “solely” basing their decisions on them.
Wit v. United Behavioral Health, a class-action lawsuit involving a subsidiary of UnitedHealth, has become one of the most consequential mental health cases of this century. In that case, a federal judge in California concluded that a number of United’s in-house guidelines did not adhere to generally accepted standards of care. The judge found that the guidelines allowed the company to wrongly deny coverage for certain mental health and substance use services the moment patients’ immediate problems improved. He ruled that the insurer would need to change its practices. United appealed the ruling on grounds other than the court’s findings about the defects in its guidelines, and a panel of judges partially upheld the decision. The case has been sent back to the district court for further proceedings.
Largely in response to the Wit case, nine states have passed laws requiring health insurers to use guidelines that align with the leading standards of mental health care, like those developed by nonprofit professional organizations.
Cigna has said that it “has chosen not to adopt private, proprietary medical necessity criteria” like MCG. But, according to a review of lawsuits, denial letters have continued to reference MCG. One federal judge in Utah called out the company, writing that Cigna doctors “reviewed the claims under medical necessity guidelines it had disavowed.” Cigna did not respond to specific questions about this.
Timothy Stock, one of the BCBS doctors who denied Moore’s request to cover ongoing care, had cited MCG guidelines when determining she had improved enough — something judges noted he had done before. In 2016, Stock upheld a decision on appeal to deny continued coverage for a teenage girl who was in residential treatment for major depression, post-traumatic stress disorder and anxiety. Pointing to the guidelines, Stock concluded she had shown enough improvement.
The patient’s family sued the insurer, alleging it had wrongly denied coverage. Blue Cross and Blue Shield of Illinois argued that there was evidence that showed the patient had been improving. But, a federal judge found the insurer misstated its significance. The judge partially ruled in the family’s favor, zeroing in on Stock and another BCBS doctor’s use of improvement to recommend denying additional care.
“The mere incidence of some improvement does not mean treatment was no longer medically necessary,” the Illinois judge wrote.
In another case, BCBS Illinois denied coverage for a girl with a long history of mental illness just a few weeks into her stay at a residential treatment facility, noting that she was “making progressive improvements.” Stock upheld the denial after an appeal.
Less than two weeks after Stock’s decision, court records show, she cut herself on the arm and leg with a broken light bulb. The insurer defended the company’s reasoning by noting that the girl “consistently denied suicidal ideation,” but a judge wrote that medical records show the girl was “not forthcoming” with her doctors about her behaviors. The judge ruled against the insurer, writing that Stock and another BCBS doctor “unreasonably ignored the weight of the medical evidence” showing that the girl required residential treatment.
Stock declined to comment. A spokesperson for BCBS said the company’s doctors who review requests for mental health coverage are board certified psychiatrists with multiple years of practice experience. The spokesperson added that the psychiatrists review all information received “from the provider, program and members to ensure members are receiving benefits for the right care, at the right place and at the right time.”
The BCBS spokesperson did not address specific questions related to Moore or Stock. The spokesperson said that the examples ProPublica asked about “are not indicative of the experience of the vast majority of our members,” and that it is committed to providing “access to quality, cost-effective physical and behavioral health care.”
A Lifelong Struggle
A former contemporary dancer with a bright smile and infectious laugh, Moore’s love of animals is eclipsed only by her affinity for plants. She moved from Indiana to Austin, Texas, about six years ago and started as a receptionist at a clinic before working her way up to technician.
Moore’s depression has been a constant in her life. It began as a child, when, she said, she was sexually and emotionally abused. She was able to manage as she grew up, getting through high school and attending Indiana University. But, she said, she fell back into a deep sadness after she learned in 2022 that the church she found comfort in as a college student turned out to be what she and others deemed a cult. In September of last year, she began an intensive outpatient program, which included multiple group and individual therapy sessions every week.
Moore, 32, had spent much of the past eight months in treatment for severe depression, post-traumatic stress disorder and anxiety when BCBS said it would no longer pay for the program in January.
The denial had come to her without warning.
“I was starting to get to the point where I did have some hope, and I was like, maybe I can see an actual end to this,” Moore said. “And it was just cut off prematurely.”
At the Austin emergency room where she drove herself after her treatment stopped, her heart raced. She was given medication as a sedative for her anxiety. According to hospital records she provided to ProPublica, Moore’s symptoms were brought on after “insurance said they would no longer pay.”
A hospital social worker frantically tried to get her back into the intensive outpatient program.
“That’s the sad thing,” said Kandyce Walker, the program’s director of nursing and chief operating officer, who initially argued Moore’s case with BCBS Texas. “To have her go from doing a little bit better to ‘I’m going to kill myself.’ It is so frustrating, and it’s heartbreaking.”
After the denial and her brief admission to the hospital emergency department in January, Moore began slicing her wrists more frequently, sometimes twice a day. She began to down six to seven glasses of wine a night.
“I really had thought and hoped that with the amount of work I’d put in, that I at least would have had some fumes to run on,” she said.
She felt embarrassed when she realized she had nothing to show for months of treatment. The skills she’d just begun to practice seemed to disappear under the weight of her despair. She considered going into debt to cover the cost of ongoing treatment but began to think that she’d rather end her life.
“In my mind,” she said, “that was the most practical thing to do.”
Whenever the thought crossed her mind — and it usually did multiple times a day — she remembered that she had promised her therapist that she wouldn’t.
Moore’s therapist encouraged her to continue calling BCBS Texas to try to restore coverage for more intensive treatment. In late February, about five weeks after Stock’s denial, records show that the company approved a request that sent her back to the same facility and at the same level of care as before.
But by that time, her condition had deteriorated so severely that it wasn’t enough.
Eight days later, Moore was admitted to a psychiatric hospital about half an hour from Austin. Medical records paint a harrowing picture of her condition. She had a plan to overdose and the medicine to do it. The doctor wrote that she required monitoring and had “substantial ongoing suicidality.” The denial continued to torment her. She told her doctor that her condition worsened after “insurance stopped covering” her treatment.
Her few weeks stay at the psychiatric hospital cost $38,945.06. The remaining 10 weeks of treatment at the intensive outpatient program — the treatment BCBS denied — would have cost about $10,000.
Moore was discharged from the hospital in March and went back into the program Stock had initially said she no longer needed.
It marked the third time she was admitted to the intensive outpatient program.
A few months later, as Moore picked at her lunch, her oversized glasses sliding down the bridge of her nose every so often, she wrestled with another painful realization. Had the BCBS doctors not issued the denial, she probably would have completed her treatment by now.
“I was really looking forward to that,” Moore said softly. As she spoke, she played with the thick stack of bracelets hiding the scars on her wrists.
A few weeks later, that small facility closed in part because of delays and denials from insurance companies, according to staff and billing records. Moore found herself calling around to treatment facilities to see which ones would accept her insurance. She finally found one, but in October, her depression had become so severe that she needed to be stepped up to a higher level of care.
Moore was able to get a leave of absence from work to attend treatment, which she worried would affect the promotion she had been working toward. To tide her over until she could go back to work, she used up the money her mother sent for her 30th birthday.
She smiles less than she did even a few months ago. When her roommates ask her to hang out downstairs, she usually declines. She has taken some steps forward, though. She stopped drinking and cutting her wrists, allowing scar tissue to cover her wounds.
But she’s still grieving what the denial took from her.
“I believed I could get better,” she said recently, her voice shaking. “With just a little more time, I could discharge, and I could live life finally.”
Kirsten Berg contributed research.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Body Scrubs: Benefits, Risks, and Guidance
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I was wondering whether I should be using a body scrub in the shower, rather than just soap. What should guide me in the choice of a body scrub, and are there any risks to be aware of?❞
Body scrubs are great for giving skin a healthy glow, but are best used sparingly—over-exfoliation leads to the opposite effect (unhappy skin, premature skin aging, etc).
As for contents:
- microplastics are now banned in most places, but you might want to check any products (and their containers!) are BPA-free, pthalate free, etc.
- fragrances in body scrubs are usually a bad idea, and many essential oils have been shown to be endocrine-disruptors, which you do not want:
About the microplastics, harmful artificial chemicals in general, and what constitutes “etc”:
About the fragrances’ (including “natural” essential oils’) endocrine-disrupting shenanigans:
Endocrine-disrupting chemicals: an Endocrine Society scientific statement
So, what might you want to use instead?
If you’re feeling adventurous, you might like to try treating yourself to a pineapple-based mask instead (a muslin cloth soaked in pineapple juice will work just fine; please don’t waterboard yourself though), as the bromelain enzymes (found very generously in pineapple juice) break down dead cells without the need for scrubbing.
Another option is a homemade salt- or sugar-scrub. Put your salt or sugar into a jar, add enough warm water to cover it, leave it for about a day, adding more water if it seems in danger of drying out, until it recrystallizes with a high water content keeping it malleable to the touch; congratulations, you now have a very simple scrub. This should still not be used more than, say, once per week, though.
Last but not least, you might consider investing in a konjac sponge; they gently remove dead skin without damaging living skin. Here’s an example product on Amazon, for your convenience
For more on gentle-yet-effective skincare, you might like to read:
Clean: The New Science of Skin and the Beauty of Doing Less
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: