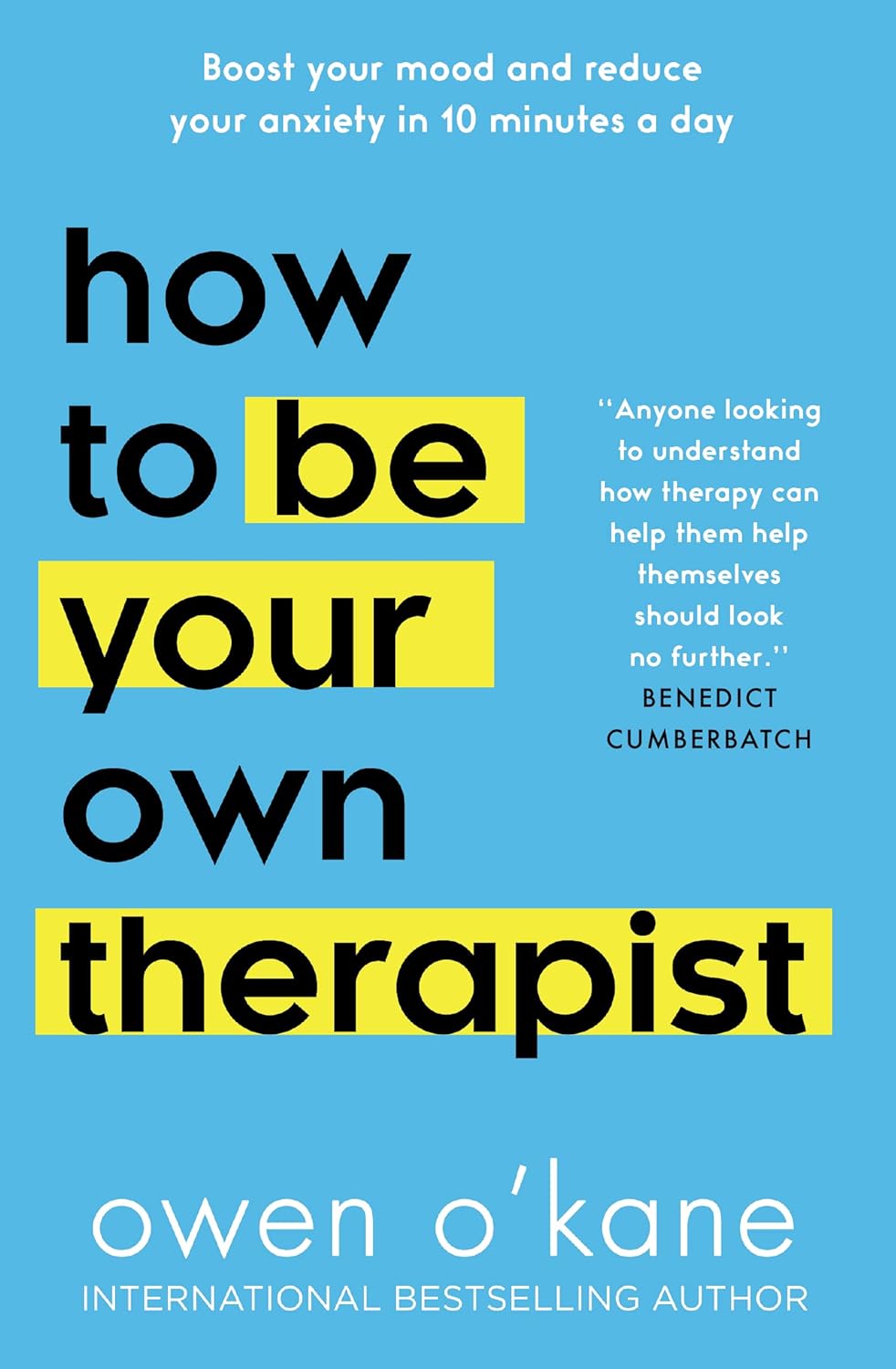
How to Be Your Own Therapist – by Owen O’Kane
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Finding the right therapist can be hard. Sometimes, even just accessing a therapist, any therapist, can be hard, if circumstances are adverse. Sometimes we’d like therapy, but want to feel “better prepared for it” before we do.
Owen O’Kane, a highly qualified and well-respected psychotherapist, wants to put some tools in our hands. The premise of this book is that “in 10 minutes a day” one can give oneself an amount of therapy that will be beneficial.
Naturally, in 10 minutes a day, this isn’t going to be the kind of therapy that will work through major traumas, so what can it do?
Those 10 minutes are spread into three sessions:
- 4 minutes in the morning
- 3 minutes in the afternoon
- 3 minutes in the evening
The idea is:
- To do a quick mental health “check-in” before the day gets started, ascertain what one needs in that context, and make a simple plan to get/have it.
- To keep one’s mental health on track by taking a little pause to reassess and adjust if necessary
- To reflect on the day, amplify the positive, and let go of the negative to what extent is practical, in order to rest well ready for the next day
Where O’Kane excels is in explaining how to do those things in a way that is neither overly simplistic and wishy-washy, nor so arcane and convoluted as to create more work and render the day more difficult.
In short, this book is a great prelude to (or adjunct to) formal therapy, and for those for whom therapy isn’t accessible and/or desired, a great way to keep oneself on a mentally healthy track.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fascia Hopping: The Powerful Over-50 Exercise You’re Probably Not Doing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A 62-year-old man reported feeling 10 years younger after just 8 days of fascia hopping. Now, anecdote ≠ data, but it seems worth investigating:
Let’s hop straight to it
Fascia is the web-like layer of connective tissue that divides your muscles and organs from each other. It simultaneously holds some stuff in place, and allows other parts to glide over each other with minimal friction.
At least, that’s what it’s supposed to do.
Like any body part, it can go wrong. And like any body part, it needs maintenance. In fascia’s case, the maintenance is to keep it slippy where it should be slippy and grippy where it should be grippy.
Here’s an exercise series for that, as described/shown in the video:
Prepping the fascia:
- Align posture: head lifted, shoulders down.
- Stretch fascia in all directions (up-down, left-right).
- Maintain a “fascia wetsuit” concept—taut but not unduly tense.
Springboard feet setup:
- Stand on balls of feet, heels slightly raised.
- Bounce gently to engage fascia elasticity.
“Fascia Strength & Power” dance:
- Move hips in a figure-eight motion.
- Keep shoulders relaxed, allowing movement to flow from the center.
Fascia hopping:
- Keep heels fixed, bounce lightly.
- Progress to small hops if possible.
- Maintain a smooth rhythm to activate elasticity.
Do these for 2 minutes daily for 7 days. It doesn’t have to be a dedicated exercise session; you can do it while you’re waiting for the water to boil in the kitchen, or things like that.
For more on these exercises plus visual demonstrations (it’s very simple), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Fascia: Why (And How) You Should Take Care Of Yours
Take care!
Share This Post
-
Stuck in fight-or-flight mode? 5 ways to complete the ‘stress cycle’ and avoid burnout or depression
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Can you remember a time when you felt stressed leading up to a big life event and then afterwards felt like a weight had been lifted? This process – the ramping up of the stress response and then feeling this settle back down – shows completion of the “stress cycle”.
Some stress in daily life is unavoidable. But remaining stressed is unhealthy. Chronic stress increases chronic health conditions, including heart disease and stroke and diabetes. It can also lead to burnout or depression.
Exercise, cognitive, creative, social and self-soothing activities help us process stress in healthier ways and complete the stress cycle.
What does the stress cycle look like?
Scientists and researchers refer to the “stress response”, often with a focus on the fight-or-flight reactions. The phrase the “stress cycle” has been made popular by self-help experts but it does have a scientific basis.
The stress cycle is our body’s response to a stressful event, whether real or perceived, physical or psychological. It could be being chased by a vicious dog, an upcoming exam or a difficult conversation.
The stress cycle has three stages:
- stage 1 is perceiving the threat
- stage 2 is the fight-or-flight response, driven by our stress hormones: adrenaline and cortisol
- stage 3 is relief, including physiological and psychological relief. This completes the stress cycle.
Different people will respond to stress differently based on their life experiences and genetics.
Unfortunately, many people experience multiple and ongoing stressors out of their control, including the cost-of-living crisis, extreme weather events and domestic violence.
Remaining in stage 2 (the flight-or-flight response), can lead to chronic stress. Chronic stress and high cortisol can increase inflammation, which damages our brain and other organs.
When you are stuck in chronic fight-or-flight mode, you don’t think clearly and are more easily distracted. Activities that provide temporary pleasure, such as eating junk food or drinking alcohol are unhelpful strategies that do not reduce the stress effects on our brain and body. Scrolling through social media is also not an effective way to complete the stress cycle. In fact, this is associated with an increased stress response.
Stress and the brain
In the brain, chronic high cortisol can shrink the hippocampus. This can impair a person’s memory and their capacity to think and concentrate.
Chronic high cortisol also reduces activity in the prefrontal cortex but increases activity in the amygdala.
The prefrontal cortex is responsible for higher-order control of our thoughts, behaviours and emotions, and is goal-directed and rational. The amygdala is involved in reflexive and emotional responses. Higher amygdala activity and lower prefrontal cortex activity explains why we are less rational and more emotional and reactive when we are stressed.
There are five types of activities that can help our brains complete the stress cycle. https://www.youtube.com/embed/eD1wliuHxHI?wmode=transparent&start=0 It can help to understand how the brain encounters stress.
1. Exercise – its own complete stress cycle
When we exercise we get a short-term spike in cortisol, followed by a healthy reduction in cortisol and adrenaline.
Exercise also increases endorphins and serotonin, which improve mood. Endorphins cause an elated feeling often called “runner’s high” and have anti-inflammatory effects.
When you exercise, there is more blood flow to the brain and higher activity in the prefrontal cortex. This is why you can often think more clearly after a walk or run. Exercise can be a helpful way to relieve feelings of stress.
Exercise can also increase the volume of the hippocampus. This is linked to better short-term and long-term memory processing, as well as reduced stress, depression and anxiety.
2. Cognitive activities – reduce negative thinking
Overly negative thinking can trigger or extend the stress response. In our 2019 research, we found the relationship between stress and cortisol was stronger in people with more negative thinking.
Higher amygdala activity and less rational thinking when you are stressed can lead to distorted thinking such as focusing on negatives and rigid “black-and-white” thinking.
Activities to reduce negative thinking and promote a more realistic view can reduce the stress response. In clinical settings this is usually called cognitive behaviour therapy.
At home, this could be journalling or writing down worries. This engages the logical and rational parts of our brain and helps us think more realistically. Finding evidence to challenge negative thoughts (“I’ve prepared well for the exam, so I can do my best”) can help to complete the stress cycle.
Journalling could help process stressful events and complete the stress cycle. Shutterstock/Fellers Photography 3. Getting creative – a pathway out of ‘flight or fight’
Creative activities can be art, craft, gardening, cooking or other activities such as doing a puzzle, juggling, music, theatre, dancing or simply being absorbed in enjoyable work.
Such pursuits increase prefrontal cortex activity and promote flow and focus.
Flow is a state of full engagement in an activity you enjoy. It lowers high-stress levels of noradrenaline, the brain’s adrenaline. When you are focussed like this, the brain only processes information relevant to the task and ignores non-relevant information, including stresses.
4. Getting social and releasing feel-good hormones
Talking with someone else, physical affection with a person or pet and laughing can all increase oxytocin. This is a chemical messenger in the brain that increases social bonding and makes us feel connected and safe.
Laughing is also a social activity that activates parts of the limbic system – the part of the brain involved in emotional and behavioural responses. This increases endorphins and serotonin and improves our mood.
5. Self-soothing
Breathing exercises and meditation stimulate the parasympathetic nervous system (which calms down our stress responses so we can “reset”) via the vagus nerves, and reduce cortisol.
A good cry can help too by releasing stress energy and increasing oxytocin and endorphins.
Emotional tears also remove cortisol and the hormone prolactin from the body. Our prior research showed cortisol and prolactin were associated with depression, anxiety and hostility.
Getting moving can help with stress and its effects on the brain. Shutterstock/Jaromir Chalabala Action beats distraction
Whether it’s watching a funny or sad movie, exercising, journalling, gardening or doing a puzzle, there is science behind why you should complete the stress cycle.
Doing at least one positive activity every day can also reduce our baseline stress level and is beneficial for good mental health and wellbeing.
Importantly, chronic stress and burnout can also indicate the need for change, such as in our workplaces. However, not all stressful circumstances can be easily changed. Remember help is always available.
If you have concerns about your stress or health, please talk to a doctor.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14 or Kids Helpline on 1800 55 1800.
Theresa Larkin, Associate professor of Medical Sciences, University of Wollongong and Susan J. Thomas, Associate professor in Mental Health and Behavioural Science, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
The Checklist Manifesto – by Dr. Atul Gawande
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Gawande, himself a general surgeon, uses checklists a lot. He is, unequivocally, an expert in his field. He “shouldn’t” need a checklist to tell him to do such things as “Check you have the correct patient”. But checklists are there as a safety net. And, famously, “safety regulations are written in blood”, after all.
And, who amongst us has never made such a “silly” error? From forgetting to turn the oven on, to forgetting to take the handbrake off, it takes only a momentary distraction to think we’ve done something we haven’t.
You may be wondering: why a whole book on this? Is it just many examples of the usefulness of checklists? Because I’m already sold on that, so, what else am I going to get out of it?
Dr. Gawande also explains in clear terms:
- How to optimize “all necessary steps” with “as few steps as possible”
- The important difference between read-do checklists and do-confirm checklists
- To what extent we should try to account for the unexpected
- How to improve compliance (i.e., making sure you actually use it, no matter how tempting it will be to go “yeah this is automatic for me now” and gloss over it)
- The role of checklists in teams, and in passing on knowledge
…and more.
Bottom line: if you’ve ever tried to make tea without putting the tea-leaves in the pot, this is the book that will help you avoid making more costly mistakes—whatever your area of activity or interest.
Click here to check out the Checklist Manifesto, and make fewer mistakes!
Share This Post
Related Posts
-
Eat To Beat Cancer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Controlling What We Can, To Avoid Cancer
Every time a cell in our body is replaced, there’s a chance it will be cancerous. Exactly what that chance is depends on very many factors. Some of them we can’t control; others, we can.
Diet is a critical, modifiable factor
We can’t choose, for example, our genes. We can, for the most part, choose our diet. Why “for the most part”?
- Some people live in a food desert (the Arctic Circle is a good example where food choices are limited by supply)
- Some people have dietary restrictions (whether by health condition e.g. allergy, intolerance, etc or by personal-but-unwavering choice, e.g. vegetarian, vegan, kosher, halal, etc)
But for most of us, most of the time, we have a good control over our diet, and so that’s an area we can and should focus on.
Choose your animal protein wisely
If you are vegan, you can skip this section. If you are not, then the short version is:
- Fish: almost certainly fine
- Poultry: the jury is out; data is leaning towards fine, though
- Red meat: significantly increased cancer risk
- Processed meat: significantly increased cancer risk
For more details (and a run-down on the science behind the above super-summarized version):
- Do We Need Animal Products To Be Healthy? ← A mythbuster article that outlines many health properties (good and bad) of animal products
- The Whys and Hows of Cutting Meats Out Of Your Diet ← A life-hack article about acting on that information
Skip The Ultra-Processed Foods
Ok, so this one’s probably not a shocker in its simplest form:
❝Studies are showing us is that not only do the ultraprocessed foods increase the risk of cancer, but that after a cancer diagnosis such foods increase the risk of dying❞
Source: Is there a connection between ultraprocessed food and cancer?
There’s an unfortunate implication here! If you took the previous advice to heart and cut out [at least some] meat, and/but then replaced that with ultra-processed synthetic meat, then this was not a great improvement in cancer risk terms.
Ultra-processed meat is worse than unprocessed, regardless of whether it was from an animal or was synthetic.
In other words: if you buy textured soy pieces (a common synthetic meat), it pays to look at the ingredients, because there’s a difference between:
- INGREDIENTS: SOY
- INGREDIENTS: Rehydrated Textured SOY Protein (52%), Water, Rapeseed Oil, SOY Protein Concentrate, Seasoning (SULPHITES) (Dextrose, Flavourings, Salt, Onion Powder, Food Starch Modified, Yeast Extract, Colour: Red Iron Oxide), SOY Leghemoglobin, Fortified WHEAT Flour (WHEAT Flour, Calcium Carbonate, Iron, Niacin, Thiamin), Bamboo Fibre, Methylcellulose, Tomato Purée, Salt, Raising Agent: Ammonium Carbonates
Now, most of those original base ingredients are/were harmless per se (as are/were the grapes in wine—before processing into alcohol), but it has clearly been processed to Hell and back to do all that.
Choose the one that just says “soy”. Or eat soybeans. Or other beans. Or lentils. Really there are a lot of options.
About soy, by the way…
There is (mostly in the US, mostly funded by the animal agriculture industry) a lot of fearmongering about soy. Which is ironic, given the amount of soy that is fed to livestock to be fed to humans, but it does bear addressing:
❝Soy foods are safe for all cancer patients and are an excellent source of plant protein. Studies show soy may improve survival after breast cancer❞
Source: Food risks and cancer: What to avoid
(obviously, if you have a soy allergy then you should not consume soy—for most people, the above advice stands, though)
Advanced Glycation End-Products
These (which are Very Bad™ for very many things, including cancer) occur specifically as a result of processing animal proteins and fats.
Note: not even necessarily ultra-processing, just processing can do it. But ultra-processing is worse. What’s the difference, you wonder?
The difference between “ultra-processed” and just “processed”:
- Your average hotdog has been ultra-processed. It’s not only usually been changed with many artificial additives, it’s also been through a series of processes (physical and chemical) and ends up bearing little relation to the creature it came from.
- Your bacon (that you bought fresh from your local butcher, not a supermarket brand of unknown provenance, and definitely not the kind that might come on the top of frozen supermarket pizza) has been processed. It’s undergone a couple of simple processes on its journey “from farm to table”. Remember also that when you cook it, that too is one more process (and one that results in a lot of AGEs).
Read more: What’s so bad about AGEs?
Note if you really don’t want to cut out certain foods, changing the way you cook them (i.e., the last process your food undergoes before you eat it) can also reduce AGES:
Advanced Glycation End Products in Foods and a Practical Guide to Their Reduction in the Diet
Get More Fiber
❝The American Institute for Cancer Research shows that for every 10-gram increase in fiber in the diet, you improve survival after cancer diagnosis by 13%❞
Source: Plant-based diet is encouraged for patients with cancer
Yes, that’s post-diagnosis, but as a general rule of thumb, what is good/bad for cancer when you have it is good/bad for cancer beforehand, too.
If you’re thinking that increasing your fiber intake means having to add bran to everything, happily there are better ways:
Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Almonds vs Macadamias – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing almonds to macadamias, we picked the almonds.
Why?
It’s not just our pro-almonds bias:
In terms of macros, almonds have 3x the protein and as well as more fiber and carbs, the ratio of which latter two give almonds the lower glycemic index, while macadamias have more total fat, and 4x the saturated fat percentage. All in all, we say this is a win for almonds in this category.
In the category of vitamins, almonds have more of vitamins B2, B3, B9, E, and choline, while macadamias have more of vitamins B1, B5, B6, and C. A modest 5:4 win for almonds, unless we consider that almonds have more than 47x as much vitamin E (almonds are an exceptionally good source of vitamin E), in which case, a stronger win for almonds.
When it comes to minerals, almonds have more calcium, copper, iron, magnesium, phosphorus, potassium, selenium, and zinc, while macadamias have more manganese. A very clear win for almonds.
Adding up the sections makes for a convincing overall win for almonds, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Why You Should Diversify Your Nuts!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Sardinian Cholesterol Paradox
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Broadly speaking, low-density lipoprotein (LDL), or “bad” cholesterol, is generally considered to be… Well… Bad. Specifically because of how it can functionally narrow arteries, causing bits of floating detritus to get stuck in it, narrow it further, and eventually harden into atherosclerotic plaque, at which point it becomes even harder for the body to clear out.
We wrote about the process here: Demystifying Cholesterol
When it comes to cholesterol, the most common lay understanding (especially under a certain age) is “it’s bad”.
A more informed view (and more common after a certain age) is “LDL cholesterol is bad; HDL cholesterol is good”.
A more nuanced view is “LDL cholesterol is established as significantly associated with (and almost certainly a causal factor of) atherosclerotic cardiovascular disease and related mortality in men; in women it is less strongly associated and may or may not be a causal factor”
We wrote more about that, here: Statins: His & Hers? ← despite most research being on men, statins have very different effects (and side effects) for women, often being relatively less useful, and more dangerous. There are exceptions (for some women’s specific profiles they can still be worthwhile), but the trend is certainly troubling.
What, then, of Sardinia?
Sardinia is well-known for being one of the “Supercentenarian Blue Zones”, a place whose inhabitants enjoy (on average, statistically) unusually healthy longevity. These places have been looked to for clues as to how to live the healthiest life.
For example: From Blue To Green: News From The Centenarian Blue Zones
However, researchers recently were investigating life in a region of Sardinia where a lot of people are aged 90+, and followed the health of 168 of them for up to 6 years (because in the case of those who died during that time, obviously the time was less than 6 years).
Note: because this was specifically a Blue Zones study, they only included participants of whom all four grandparents were born within the Blue Zone—so not, for example, looking at the health of someone who just moved there from New York, say.
They collected a lot of interesting data (of course), but what we’re talking about today is that they found that participants with LDL levels above 130 mg/dL had a significantly longer average survival than those with LDL levels below this threshold. Specifically, a 40% lower mortality risk.
This is interesting, because LDL levels ≥130 mg/dL are considered moderate hypercholesterolemia (i.e., the LDL levels are a bit too high).
However, if the same participants had total cholesterol levels over 250mg/dL, they got no extra survival benefits, and very high cholesterol was still linked with shorter survival.
You can read the paper here: The Cholesterol Paradox in Long-Livers from a Sardinia Longevity Hot Spot (Blue Zone)
But before you reach for the butter…
The researchers have several hypotheses about why these results could be so, including:
- The longevity has less to do with LDL itself, and more to do with the diet, with the ratio of grain to olive oil.
- Most of the participants with higher LDL cholesterol were on antihypertensive drugs, which a) will obviously have a cardioprotective effect, and b) means that their heart health is probably enjoying greater scrutiny, and medical scrutiny can also have a protective effect (indeed, that’s the point of it).
- It was also speculated that the locals of that region may have a genetic defense against the harm of moderate hypercholesterolemia, due to historical exposure to malaria meaning that naturally slightly higher cholesterol levels without increased cardiovascular risk may have been naturally selected-for (i.e. those without it were more likely to die of malaria and not pass on their genes).
Thus, it may be that it’s not so applicable more generally. However, it is still reason to at least re-examine how bad LDL cholesterol actually is, and whether for some demographics it could have a protective factor (much like “overweight” BMI is a protective factor for people over 65).
Still, if you’d like to keep on top of your cholesterol levels, check out:
How To Lower Cholesterol Naturally, Without Statins
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: