How they did it: STAT reporters expose how ailing seniors suffer when Medicare Advantage plans use algorithms to deny care
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a call with a long-time source, what stood out most to STAT reporters Bob Herman and Casey Ross was just how viscerally frustrated and angry the source was about an algorithm used by insurance companies to decide how long patients should stay in a nursing home or rehab facility before being sent home.
The STAT stories had a far-reaching impact:
- The U.S. Senate Committee on Homeland Security and Government Affairs took a rare step of launching a formal investigation into the use of algorithms by the country’s three largest Medicare Advantage insurers.
- Thirty-two House members urged the Centers for Medicare and Medicaid Services to increase the oversight of algorithms that health insurers use to make coverage decisions.
- In a rare step, CMS launched its own investigation into UnitedHealth. It also stiffened its regulations on the use of proprietary algorithms and introduced plans to audit denials across Medicare Advantage plans in 2024.
- Based on STAT’s reporting, Medicare Advantage beneficiaries filed two class-action lawsuits against UnitedHealth and its NaviHealth subsidiary, the maker of the algorithm, and against Humana, another major health insurance company that was also using the algorithm.
- Amid scrutiny, UnitedHealth renamed NaviHealth.
The companies never allowed an on-the-record interview with their executives, but they acknowledged that STAT’s reporting was true, according to the news organization.
Ross and Herman spoke with The Journalist’s Resource about their project and shared the following eight tips.
1. Search public comments on proposed federal rules to find sources.
Herman and Ross knew that the Centers for Medicare and Medicaid Services had put out a request for public comments, asking stakeholders within the Medicare Advantage industry how the system could improve.
There are two main ways to get Medicare coverage: original Medicare, which is a fee-for-service health plan, and Medicare Advantage, which is a type of Medicare health plan offered by private insurance companies that contract with Medicare. Medicare Advantage plans have increasingly become popular in recent years.
Under the Social Security Act, the public has the opportunity to submit comments on Medicare’s proposed national coverage determinations. CMS uses public comments to inform its proposed and final decisions. It responds in detail to all public comments when issuing a final decision.
The reporters began combing through hundreds of public comments attached to a proposed Medicare Advantage rule that was undergoing federal review. NaviHealth, the UnitedHealth subsidiary and the maker of the algorithm, came up in many of the comments, which include the submitters’ information.
“These are screaming all-caps comments to federal regulators about YOU NEED TO SOMETHING ABOUT THIS BECAUSE IT’S DISGUSTING,” Ross says.
“The federal government is proposing rules and regulations all the time,” adds Herman, STAT’s business of health care reporter. “If someone’s going to take the time and effort to comment on them, they must have at least some knowledge of what’s going on. It’s just a great tool for any journalist to use to figure out more and who to contact.”
The reporters also found several attorneys who had complained in the comments. They began reaching out to them, eventually gaining access to confidential documents and intermediaries who put them in touch with patients to show the human impact of the algorithm.
2. Harness the power of the reader submission box.
At the suggestion of an editor, the reporters added a reader submission box at the bottom of their first story, asking them to share their own experiences with Medicare Advantage denials.
The floodgates opened. Hundreds of submissions arrived.
By the end of their first story, Herman and Ross had confidential records and some patients, but they had no internal sources in the companies they were investigating, including Navihealth. The submission box led them to their first internal source.
The journalists also combed through LinkedIn and reached out to former and current employees, but the response rate was much lower than what they received via the submission box.
The submission box “is just right there,” Herman says. “People who would want to reach out to us can do it right then and there after they read the story and it’s fresh in their minds.”
3. Mine podcasts relevant to your story.
The reporters weren’t sure if they could get interviews with some of the key figures in the story, including Tom Scully, the former head of the Centers for Medicare and Medicaid Services who drew up the initial plans for NaviHealth years before UnitedHealth acquired it.
But Herman and another colleague had written previously about Scully’s private equity firm and they had found a podcast where he talked about his work. So Herman went back to the podcast — where he discovered Scully had also discussed NaviHealth.
The reporters also used the podcast to get Scully on the phone for an interview.
“So we knew we had a good jumping off point there to be like, ‘OK, you’ve talked about NaviHealth on a podcast, let’s talk about this,’” Herman says. “I think that helped make him more willing to speak with us.”
4. When covering AI initiatives, proceed with caution.
“A source of mine once said to me, ‘AI is not magic,’” Ross says. “People need to just ask questions about it because AI has this aura about it that it’s objective, that it’s accurate, that it’s unquestionable, that it never fails. And that is not true.”
AI is not a neutral, objective machine, Ross says. “It’s based on data that’s fed into it and people need to ask questions about that data.”
He suggests several questions to ask about the data behind AI tools:
- Where does the data come from?
- Who does it represent?
- How is this tool being applied?
- Do the people to whom the tool is being applied match the data on which it was trained? “If racial groups or genders or age of economic situations are not adequately represented in the training set, then there can be an awful lot of bias in the output of the tool and how it’s applied,” Ross says.
- How is the tool applied within the institution? Are people being forced to forsake their judgment and their own ability to do their jobs to follow the algorithm?
5. Localize the story.
More than half of all Medicare beneficiaries have Medicare Advantage and there’s a high likelihood that there are multiple Medicare Advantage plans in every county across the nation.
“So it’s worth looking to see how Medicare Advantage plans are growing in your area,” Herman says.
Finding out about AI use will most likely rely on shoe-leather reporting of speaking with providers, nursing homes and rehab facilities, attorneys and patients in your community, he says. Another source is home health agencies, which may be caring for patients who were kicked out of nursing homes and rehab facilities too soon because of a decision by an algorithm.
The anecdote that opens their first story involves a small regional health insurer in Wisconsin, which was using NaviHealth and a contractor to manage post-acute care services, Ross says.
“It’s happening to people in small communities who have no idea that this insurer they’ve signed up with is using this tool made by this other company that operates nationally,” Ross says.
There are also plenty of other companies like NaviHealth that are being used by Medicare Advantage plans, Herman says. “So it’s understanding which Medicare Advantage plans are being sold in your area and then which post-acute management companies they’re using,” he adds.
Some regional insurers have online documents that show which contractors they use to evaluate post-acute care services.
6. Get familiar with Medicare’s appeals databases
Medicare beneficiaries can contest Medicare Advantage denials through a five-stage process, which can last months to years. The appeals can be filed via the Office of Medicare Hearings and Appeals.
“Between 2020 and 2022, the number of appeals filed to contest Medicare Advantage denials shot up 58%, with nearly 150,000 requests to review a denial filed in 2022, according to a federal database,” Ross and Herman write in their first story. “Federal records show most denials for skilled nursing care are eventually overturned, either by the plan itself or an independent body that adjudicates Medicare appeals.”
There are several sources to find appeals data. Be mindful that the cases themselves are not public to protect patient privacy, but you can find the number of appeals filed and the rationale for decisions.
CMS has two quality improvement organizations, or QIOs, Livanta and Kepro, which are required to file free, publicly-available annual reports, about the cases they handle, Ross says.
Another company, Maximus, a Quality Improvement Contractor, also files reports on prior authorization cases it adjudicates for Medicare. The free annual reports include data on raw numbers of cases and basic information about the percentage denials either overturned or upheld on appeal, Ross explains.
CMS also maintains its own database on appeals for Medicare Part C (Medicare Advantage plans) and Part D, which covers prescription drugs, although the data is not complete, Ross explains.
7. Give your editor regular updates.
“Sprinkle the breadcrumbs in front of your editors,” Ross says.
“If you wrap your editors in the process, you’re more likely to be able to get to the end of [the story] before they say, ‘That’s it! Give me your copy,’” Ross says.
8. Get that first story out.
“You don’t have to know everything before you write that first story,” Ross says. “Because with that first story, if it has credibility and it resonates with people, sources will come forward and sources will continue to come forward.”
Read the stories
Denied by AI: How Medicare Advantage plans use algorithms to cut off care for seniors in need
UnitedHealth pushed employees to follow an algorithm to cut off Medicare patients’ rehab care
UnitedHealth used secret rules to restrict rehab care for seriously ill Medicare Advantage patients
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Natural Alternatives for Depression Treatment
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Questions and Answers at 10almonds
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
Natural alternatives to medication for depression?
Great question! We did a mean feature a while back, but we definitely have much more to say! We’ll do another main feature soon, but in the meantime, here’s what we previously wrote:
See: The Mental Health First-Aid That You’ll Hopefully Never Need
^This covers not just the obvious, but also why the most common advice is not helpful, and practical tips to actually make manageable steps back to wellness, on days when “literally just survive the day” is one’s default goal.
Share This Post
-
Goji Berries vs Cherries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing goji berries to cherries, we picked the goji berries.
Why?
Looking at the macros first, goji berries have more protein, fiber, and carbs, as well as the lower glycemic index, although cherries are great too. Still, a clear and easy win here.
In the category of vitamins, goji berries have more of vitamins A and C, while cherries have more of vitamin K; in the other vitamins these two fruits are close enough to equal that variants in what kind of cherry it is will push it slightly one way or the other. However, it’s worth noting that goji berries have 1,991% more vitamin A and 16,033% more vitamin C, while cherries have only 20% more vitamin K. So, all in all, another clear win for goji berries.
When it comes to minerals, goji berries have more calcium and iron, while cherries have more copper. Again, the margins of difference are very much in goji berries’ favor, with 1,088% more calcium and 2,025% more iron, while cherries have 35% more copper. So, again, a win for goji berries.
The polyphenol contents of cherries differ far too much to comment here, but as a general rule of thumb, goji berries have more antioxidant powers than cherries, but cherries are also excellent for this.
In short, enjoy either or both, but goji berries are the more nutritionally dense!
Want to learn more?
You might like to read:
Take care!
Share This Post
-
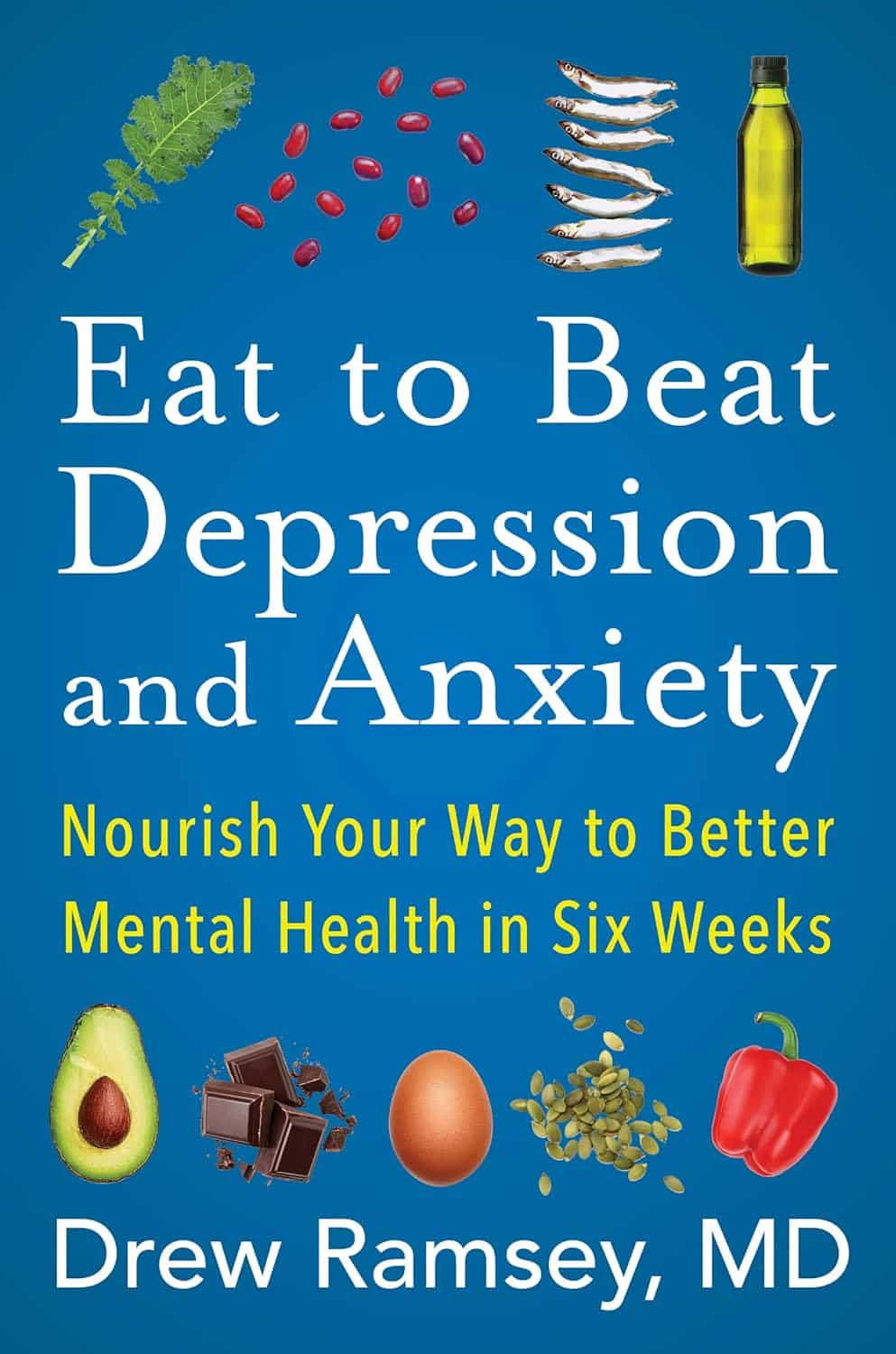
Eat to Beat Depression and Anxiety – by Dr. Drew Ramsey
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most of us could use a little mood boost sometimes, and some of us could definitely stand to have our baseline neurochemistry elevated a bit. We’ve probably Googled “foods to increase dopamine”, and similar phrases. So, why is this a book, and not just an article saying to eat cashews and dark chocolate?
Dr. Drew Ramsey takes a holistic approach to health. By this we mean that to have good health, the whole body and mind must be kept healthy. Let a part slip, and the others will soon follow. Improve a part, and the others will soon follow, too.
Of course, there is only so much that diet can do. Jut as no diet will replace a Type 1 Diabetic’s pancreas with a working one, no diet will treat the causes of some kinds of depression and anxiety.
For this reason, Dr. Ramsey, himself a psychiatrist (and a farmer!) recommends a combination of talking therapy and diet, with medications as a “third leg” to be included when necessary. The goal, for him, is to reduce dependence on medications, while still recognizing when they can be useful or even necessary.
As for the practical, actionable advices in the book, he does (unsurprisingly) recommend a Mediterranean diet. Heavy on the greens and beans, plenty of colorful fruit and veg, small amounts of fish and seafood, even smaller amounts of grass-fed beef and fermented dairy. He also discusses a bunch of “superfoods” he particularly recommends.
Nor does he just hand-wave the process; he talks about the science of how and why each of these things helps.
And in practical terms, he even devotes some time to helping the reader get our kitchen set up, if we’re not already ready-to-go in that department. He also caters to any “can’t cook / won’t cook” readers and how to work around that too.
Bottom line: if you’d like to get rewiring your brain (leveraging neuroplasticity is a key component of the book), this will get you on track. A particular strength is how the author “thinks of everything” in terms of common problems that people (especially: depressed and anxious people!) might have in implementing his advices.
Share This Post
Related Posts
-
Can You Repair Your Own Teeth At Home?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I liked your article on tooth remineralization, I saw a “home tooth repair kit”, and wondered if it is as good as what dentists do, or at least will do the job well enough to save a dentist visit?❞
Firstly, for any wondering about the tooth remineralization, here you go:
Tooth Remineralization: How To Heal Your Teeth Naturally
Now, to answer your question, we presume you are talking about something like this kit available on Amazon. In which case, some things to bear in mind:
- This kind of thing is generally intended as a stop-gap measure until you see a dentist, because you cracked your tooth or lost a filling or something today, and will see the dentist next week, say.
- This kind of thing is not what Dr. Michelle Jorgensen was talking about in another video* that we wrote about; rather, it is using a polymer filler to rebuild what is missing. The key difference is: this is using plastic, which is not what your teeth are made of, so it will never “take” as part of the tooth, as some biomimetic dentistry options can do.
- Yes, this does also mean you are putting microplastics (because the powder is usually micronized polymer beads with zinc oxide, to which you add a liquid to create a paste that will set) in your mouth and quite possibly right next to an open blood supply depending on what’s damaged and whether capillaries were reaching it.
- Because of the different material and application method, the adhesion is nothing like professional fillings (be they metal or resin), and thus the chances of it coming out again or so high that it’s more a question of when, rather than if.
- If you have damage under there (as we presume you do in any scenario where you are using this), then if it’s not professionally cleaned before the filling goes in, then it can get infected, and (less dramatically, but still importantly) any extant decay can also get worse. We say “professionally”, because you will not be able to do an adequate job with your toothbrush, floss, etc at home, and even if you got dentist’s tools (which you can buy, by the way, but we don’t recommend), you will no more be able to do the same quality job as a dentist who has done that many times a day every day for the past 20 years, as buying expensive paintbrushes would make you able to restore a Renaissance painting without messing it up.
*See: Dangers Of Root Canals And Crowns, & What To Do Instead ← what she recommends instead is biomimetic dentistry, which is also more prosaically called “conservative restorative dentistry”, i.e. it tries to conserve as much as possible, replace lost material on a like-for-like basis, and generally end up with a result that’s as close to natural as possible.
In other words, the short answer to your question is “no, sorry, it isn’t and it won’t”
However! A just like it’s good to have a first aid kit in the house even if it won’t do the same job as an ambulance crew, it can be good to have a tooth repair kit (essentially, a tooth first-aid kit) in the house, precisely to use it just as a stop-gap measure in the event that you one day crack a tooth or lose a filling or such, and don’t want to leave it open to all things in the meantime.
(The results of this sort of kit are so not long-term in nature that it will be quick and easy for your dentist to remove it to do their own job once you get there)
If in doubt, always see your dentist as soon as possible, as many things are a lot less work to treat now, than to treat later. Just, make sure to advocate for yourself and what you actually want/need, and don’t let them upsell you on something you didn’t come in for while you’re sitting in their chair—that’s a conversation to be had in advance with a clear head and no pressure (and nobody’s hands in your mouth)!
See also: Dentists Are Pulling ‘Healthy’ and Treatable Teeth To Profit From Implants, Experts Warn
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What you need to know about endometriosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Endometriosis affects one in 10 people with a uterus who are of reproductive age. This condition occurs when tissue similar to the endometrium—the inner lining of the uterus—grows on organs outside of the uterus, causing severe pain that impacts patients’ quality of life.
Read on to learn more about endometriosis: What it is, how it’s diagnosed and treated, where patients can find support, and more.
What is endometriosis, and what areas of the body can it affect?
The endometrium is the tissue that lines the inside of the uterus and sheds during each menstrual cycle. Endometriosis occurs when endometrial-like tissue grows outside of the uterus.
This tissue can typically grow in the pelvic region and may affect the outside of the uterus, fallopian tubes, ovaries, vagina, bladder, intestines, and rectum. It has also been observed outside of the pelvis on the lungs, spleen, liver, and brain.
What are the symptoms?
Symptoms may include pelvic pain and cramping before or during menstrual periods, heavy menstrual bleeding, bleeding or spotting between periods, pain with bowel movements or urination, pain during or after sex or orgasm, fatigue, nausea, bloating, and infertility.
The pain associated with this condition has been linked to depression, anxiety, and eating disorders. A meta-analysis published in 2019 found that more than two-thirds of patients with endometriosis report psychological stress due to their symptoms.
Who is at risk?
Endometriosis most commonly occurs in people with a uterus between the ages of 25 and 40, but it can also affect pre-pubescent and post-menopausal people. In rare cases, it has been documented in cisgender men.
Scientists still don’t know what causes the endometrial-like tissue to grow, but research shows that people with a family history of endometriosis are at a higher risk of developing the condition. Other risk factors include early menstruation, short menstrual cycles, high estrogen, low body mass, and starting menopause at an older age.
There is no known way to prevent endometriosis.
How does endometriosis affect fertility?
Up to 50 percent of people with endometriosis may struggle to get pregnant. Adhesions and scarring on the fallopian tubes and ovaries as well as changes in hormones and egg quality can contribute to infertility.
Additionally, when patients with this condition are able to conceive, they may face an increased risk of pregnancy complications and adverse pregnancy outcomes.
Treating endometriosis, taking fertility medications, and using assistive reproductive technology like in vitro fertilization can improve fertility outcomes.
How is endometriosis diagnosed, and what challenges do patients face when seeking a diagnosis?
A doctor may perform a pelvic exam and request an ultrasound or MRI. These exams and tests help identify cysts or other unusual tissue that may indicate endometriosis.
Endometriosis can only be confirmed through a surgical laparoscopy (although less-invasive diagnostic tests are currently in development). During the procedure, a surgeon makes a small cut in the patient’s abdomen and inserts a thin scope to check for endometrial-like tissue outside of the uterus. The surgeon may take a biopsy, or a small sample, and send it to a lab.
It takes an average of 10 years for patients to be properly diagnosed with endometriosis. A 2023 U.K. study found that stigma around menstrual health, the normalization of menstrual pain, and a lack of medical training about the condition contribute to delayed diagnoses. Patients also report that health care providers dismiss their pain and attribute their symptoms to psychological factors.
Additionally, endometriosis has typically been studied among white, cisgender populations. Data on the prevalence of endometriosis among people of color and transgender people is limited, so patients in those communities face additional barriers to care.
What treatment options are available?
Treatment for endometriosis depends on its severity. Management options include:
- Over-the-counter pain medication to alleviate pelvic pain
- Hormonal birth control to facilitate lighter, less painful periods
- Hormonal medications such as gonadotropin-releasing hormone (GnRH) or danazol, which stop the production of hormones that cause menstruation
- Progestin therapy, which may stop the growth of endometriosis tissue
- Aromatase inhibitors, which reduce estrogen
In some cases, a doctor may perform a laparoscopic surgery to remove endometrial-like tissue.
Depending on the severity of the patient’s symptoms and scar tissue, some doctors may also recommend a hysterectomy, or the removal of the uterus, to alleviate symptoms. Doctors may also recommend removing the patient’s ovaries, inducing early menopause to potentially improve pain.
Where can people living with endometriosis find support?
Given the documented mental health impacts of endometriosis, patients with this condition may benefit from therapy, as well as support from others living with the same symptoms. Some peer support organizations include:
- Endometriosis Coalition Patient Support Group (virtual)
- MyEndometriosisTeam (virtual)
- Endo Black, Inc. (Washington, D.C.)
- endoQueer (virtual)
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Nudge – by Richard Thaler & Cass Sunstein
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How often in life do we make a suboptimal decision that ends up plaguing us for a long time afterwards? Sometimes, a single good or bad decision can even directly change the rest of our life.
So, it really is important that we try to optimize the decisions we do make.
Professors Richard Thaler and Cass Sunstein look at all kinds of decision-making in this book. Their goal, as per the subtitle, is “improving decisions about health, wealth, and happiness”.
For the most part, the book concentrates on “nudges”. Small factors that influence our decisions one way or another.
Most importantly: that some of them are very good reasons to be nudged; others, very bad ones. And they often look similar.
Where this book excels is in highlighting the many ways we make decisions without even thinking about it… or we think about it, but only down a prescribed, foreseen track, to an externally expected conclusion (for example, an insurance company offering three packages, but two of them exist only to direct you to the “correct” choice).
A weakness of the book is that in some aspects it’s a little inconsistent. The authors describe their economic philosophy as “libertarian paternalism”, and as libertarians they’re against mandates, except when as paternalists they’re for them. But, if we take away their labels, this boils down to “some mandates can be good and some can be bad”, which would not be so inconsistent after all.
Bottom line: if you’d like to better understand your own decision-making processes through the eyes of policy-setting economists (especially Sunstein, who worked for the White House Office of Information & Regulatory Affairs) whose job it is to make sure you make the “right” decisions, then this is a very enlightening book.
Click here to check out Nudge and improve your decision-making clarity!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: