Gut Renovation – by Dr. Roshini Raj, with Sheila Buff
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Unless we actually feel something going on down there, gut health is an oft-neglected part of overall health—which is unfortunate, because invisible as it may often be, it affects so much.
Gastroenterologist Dr. Roshini Raj gives us all the need-to-know information, explanations of why things happen the way they do with regard to the gut, and tips, tricks, and hacks to improve matters.
She also does some mythbusting along the way, and advises about what things don’t make a huge difference, including what medications don’t have a lot of evidence for their usefulness.
The style is easy-reading pop-science, with plenty of high-quality medical content.
Reading between the lines, a lot of the book as it stands was probably written by the co-author, Sheila Buff, who is a professional ghostwriter and specializes in working closely with doctors to produce works that are readable and informative to the layperson while still being full of the doctor’s knowledge and expertise. So a reasonable scenario is that Dr. Raj gave her extensive notes, she took it from there, passed it back to her for medical corrections, and they had a little back and forth until it was done. Whatever their setup, the end result was definitely good!
Bottom line: if you’d like a guide to gut health that’s practical and easy to read, while being quite comprehensive and certainly a lot more than “eat probiotics and fiber”, then this book is a fine choice.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Aging Is Inevitable… Or is it?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Aging is inevitable… Or is it?
We’ve talked before about how and why aging happens. We’ve also talked about the work to tackle aging as basically an engineering problem, with the premise that our bodies are biological machines, and machines can be repaired. We also recommended a great book about this, by the way. But that’s about interfering with the biological process of aging. What about if the damage is already done?
“When the damage is done, it’s done”
We can do a lot to try to protect ourselves from aging, and we might be able to slow down the clock, but we can’t stop it, and we certainly can’t reverse it… right?
Wrong! Or at least, so we currently understand, in some respects. Supplementation with phosphatidylserine, for example, has shown promise for not just preventing, but treating, neurodegeneration (such as that caused by Alzheimer’s disease). It’s not a magic bullet and so far the science is at “probably” and “this shows great promise for…” and “this appears to…”
Phosphatidylserene does help slow neurodegeneration
…because of its role in allowing your cells to know whether they have permission to die.
This may seem a flippant way of putting it, but it’s basically how cell death works. Cells do need to die (if they don’t, that’s called cancer) and be replaced with new copies, and those copies need to be made before too much damage is accumulated (otherwise the damage is compounded with each new iteration). So an early cell death-and-replacement is generally better for your overall health than a later one.
However, neurons are tricky to replace, so phosphatidylserine effectively says “not you, hold on” to keep the rate of neuronal cell death nearer to the (slow) rate at which they can be replaced.
One more myth to bust…
For the longest time we thought that adults, especially older adults, couldn’t make new brain cells at all, that we grew a certain number, then had to hang onto them until we died… suffering diminished cognitive ability with age, on account of losing brain cells along the way.
It’s partly true: it’s definitely easier to kill brain cells than to grow them… Mind you, that’s technically true of people, too, yet the population continues to boom!
Anyway, new research showing that adults do, in fact, grow new braincells was briefly challenged by a 2018 study that declared: Human hippocampal neurogenesis drops sharply in children to undetectable levels in adults after all, never mind, go back to your business.
So was adult neurogenesis just a myth to be busted after all? Nope.
It turned out, the 2018 study had a methodological flaw!
To put it in lay terms: they had accidentally melted the evidence.
A 2019 study overcame this flaw by using a shorter fixation time for the cell samples they wanted to look at, and found that there were tens of thousands of “baby neurons” (again with the lay terms), newly-made brain cells, in samples from adults ranging from 43 to 87.
Now, there was still a difference: the samples from the youngest adult had 30% more newly-made braincells than the 87-year-old, but given that previous science thought brain cell generation stopped in childhood, the fact that an 87-year-old was generating new brain cells 30% less quickly than a 43-year-old is hardly much of a criticism!
As an aside: samples from patients with Alzheimer’s also had a 30% reduction in new braincell generation, compared to samples from patients of the same age without Alzheimer’s. But again… Even patients with Alzheimer’s were still growing some new brain cells.
Read it for yourself: Adult hippocampal neurogenesis is abundant in neurologically healthy subjects and drops sharply in patients with Alzheimer’s disease
In a nutshell…
- We can’t fully hit pause on aging just yet, but we can definitely genuinely slow it
- We can also, in some very specific ways, reverse it
- We can slow the loss of brain cells
- We can grow new brain cells
- We can reduce our risk of Alzheimer’s, and at least somewhat mitigate it if it appears
- We know that phosphatidylserine supplementation may help with most (if not all) of the above
- We don’t sell that (or anything else) but for your convenience, here it is on Amazon if you’re interested
Share This Post
-
How To Grow In Comfort
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Grow (Without Leaving Your Comfort Zone)
“You have to get out of your comfort zone!” we are told, from cradle to grave.
When we are young, we are advised (or sometimes more forcefully instructed!) that we have to try new things. In our middle age, we are expected to be the world’s greatest go-getters, afraid of nothing and always pushing limits. And when we are old, people bid us “don’t be such a dinosaur”.
It is assumed, unquestioned, that growth can only occur through hardship and discomfort.
But what if that’s a discomforting lie?
Butler (2023) posited an idea: “We never achieve success faster and with less effort than when we are in our comfort zone”
Her words are an obvious callback to the ideas of Csikszentmihalyi (1970) in the sense of “flow”, in the sense in which that word is used in psychology.
Flow is: when a person is in a state of energized focus, full involvement, and enjoyment of an activity.
As a necessary truth (i.e: a function of syllogistic logic), the conditions of “in a state of flow” and “outside of one’s comfort zone” cannot overlap.
From there, we can further deduce (again by simple logic) that if flow can be found, and/but cannot be found outside of the comfort zone, then flow can only be found within the comfort zone.
That is indeed comforting, but what about growth?
Imagine you’ve never gone camping in your life, but you want to get outside of your comfort zone, and now’s the time to do it. So, you check out some maps of the Yukon, purchase some camping gear, and off you go into the wilderness. In the event that you survive to report it, you will indeed be able to say “it was not comfortable”.
But, did growth occur? Maybe, but… it’s a folly to say “what doesn’t kill us makes us stronger” as a reason to pursue such things. Firstly, there’s a high chance it may kill us. Secondly, what doesn’t kill us often leaves us incredibly weakened and vulnerable.
When Hannibal famously took his large army of mostly African mercenaries across the Alps during winter to march on Rome from the other side, he lost most of his men on the way, before proceeding to terrorize Northern Italy convincingly with the small remainder. But! Their hard experience hadn’t made them stronger; it had just removed the weaker soldiers, making the resultant formations harder to break.
All this to say, please do not inflict hardship and discomfort and danger in the hopes it’ll make you stronger; it will probably do the opposite.
But…
If, instead of wilderness trekking in the Yukon…
- You start off with a camper van holiday, then you’ll be taking a fair amount of your comfort with you. In effect, you will be stretching and expanding your comfort zone without leaving it.
- Then maybe another year you might try camping in a tent on a well-catered camping site.
- Later, you might try “roughing it” at a much less well-catered camping site.
- And so on.
Congratulations, you have tried new things and undergone growth, taking your comfort zone with you all the way!
This is more than just “easing yourself into” something
It really is about taking your comfort with you too. If you want to take up running, don’t ask “how can I run just a little bit first” or “how can I make it easier” (well, feel free to ask those things too, but) ask yourself: how can I bring my comfort with me? Comfortable shoes, perhaps, an ergonomic water bottle, shade for your head, maybe.
❝Any fool can rough it, but a good soldier can make himself comfortable in any circumstances❞
~ British Army maxim
This goes for more than just physical stuff, too
If you want to learn a new skill, the initial learning curve can be anxiety-inducing, especially if you are taking a course and worried about keeping up or “not being good enough”.
So, “secretly” study in advance, at your leisure, get yourself a head start. Find a degree of comfort in what you’ve learned so far, and then bring that comfort with you into your entry-level course that is now less intimidating.
Discomfort isn’t a badge of honor (and impedes growth)
Take that extra rest stop on the highway. Bring your favorite coffee with you. Use that walking stick, if it helps.
Whatever it takes to bring your comfort with you, bring it.
Trust us, you’ll get further that way.
Share This Post
-
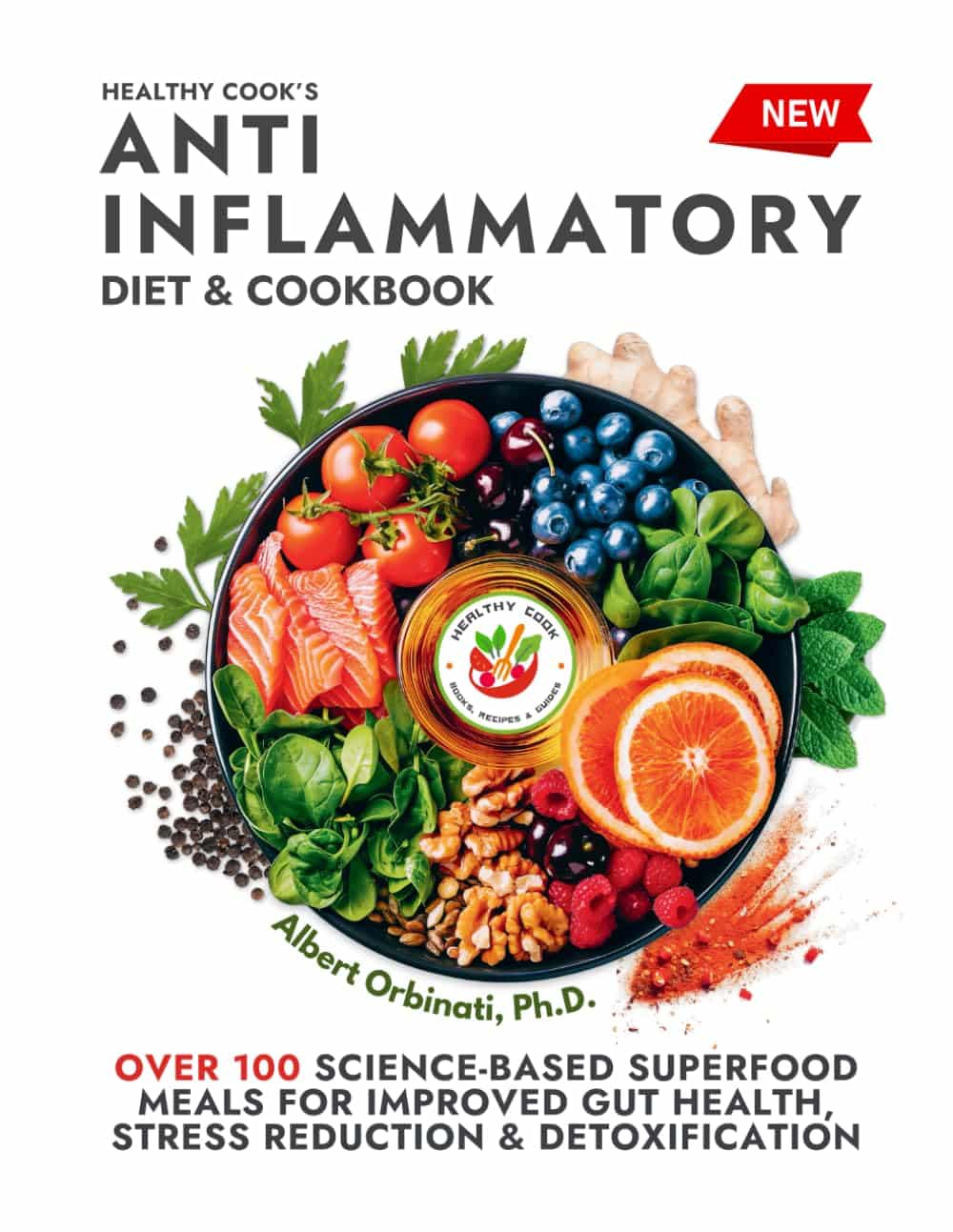
Healthy Cook’s Anti-Inflammatory Diet & Cookbook – by Dr. Albert Orbinati
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Chronic inflammation is a root cause of very many illnesses, and exacerbates almost all the ones it doesn’t cause. So, reducing inflammation is a very good way to stay well in general, reducing one’s risk factors for very many other diseases.
Dr. Orbinati starts by giving advice for adjusting to an anti-inflammatory diet, including advice on trying an elimination diet, if you suspect an undiagnosed allergy/intolerance.
Thereafter, he gives guidance on pantry-stocking—not just what anti-inflammatory foods to include and what inflammatory foods to skip, but also, what food and nutrient pairings are particularly beneficial, like how black pepper and turmeric are both anti-inflammatory by themselves, but the former greatly increases the bioavailability of the latter if consumed together.
The rest of the book—aside from assorted appendices, such as 8 pages of scientific references—is given over to the recipes.
The recipes themselves are, obviously, anti-inflammatory in focus. As one might expect, therefore, most are vegetarian and many are vegan, but we do find many recipes with chicken and fish as well; there’s also some use of eggs and fermented dairy in some of the recipes too.
The book certainly does deliver on its promise of flavorful healthy food; that’s what happens when one includes a lot of herbs and spices in one’s cooking, as well as the fact that many other polyphenol-rich foods are, by nature, tasty in and of themselves.
Bottom line: if you’d like to expand your anti-inflammatory culinary repertoire, this book is a top-tier choice for that.
Click here to check out Healthy Cook’s Anti-Inflammatory Diet & Cookbook, and spice up your kitchen!
Share This Post
Related Posts
-
I Contain Multitudes – by Ed Yong
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A little while back we reviewed a book (Planet of Viruses) about the role of viruses in our lives, beyond the obvious. Today’s book gives the same treatment to microbes in general—mostly bacteria.
We all know about pathogens, and we all know about gut microbiota and that some (hopefully the majority) there are good for our health. This book covers those things too, but also much more.
Pulitzer Prize-winning science writer Ed Yong takes a big picture view (albeit, of some very small things) and looks at the many ways microbes keep us alive, directly or indirectly. From the microbes that convert certain proteins in breast milk into a form that babies can digest (yes, this means we produce nutrients in breast milk that have been evolved solely to feed that bacterium), to those without which agriculture would simply not work, we’re brought to realize how much our continued existence is contingent on our trillions of tiny friends.
The style throughout is easy-reading pop-science, very accessible. There’s also plenty in terms of practical take-away value, when it comes to adjusting our modern lives to better optimize the benefits we get from microbes—inside and out.
Bottom line: if you’d like to learn about the role of microbes in our life beyond “these ones are pathogens” and “these ones help our digestion”, this is the book for you.
Click here to check out I Contain Multitudes, and learn more about yours and those around you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
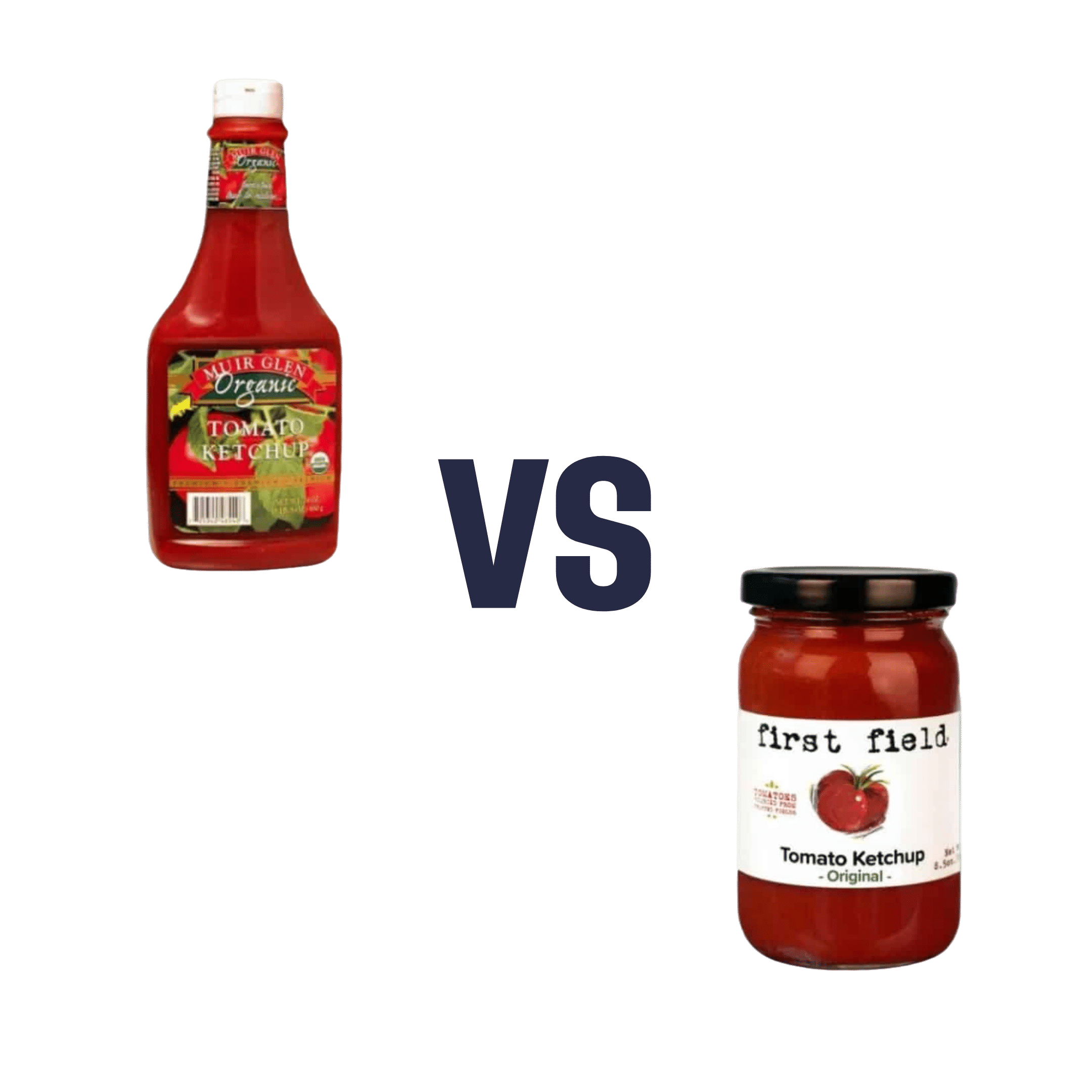
Muir Glen Organic vs First Field Original – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Muir Glen Organic Ketchup to First Field Original Ketchup, we picked the First Field.
Why?
This one was a little unfair to you, as you can’t turn them around to read the ingredients here. But the point we want to share the most today is: you have to turn them around and read the ingredients! You absolutely cannot rely on appearances!
While the Muir Glen Organic may have a very “greenwashed” aesthetic going on and the word “organic” is more eye-catching than any other word on the label, it contains 4x as much sugar and 4x as much sodium.
Side-by-side, they have, per tablespoon:
First Field Original: 1g sugar, 60mg sodium
Muir Glen Organic: 4g sugar, 240mg sodiumBut what about the importance of being organic?
Well, we have one more surprise for you: the First Field ketchup is organic too, non-GMO, and contains no added concentrates either.
This isn’t an ad for First Field (by all means enjoy their products or don’t; we’re not invested), but it is a heartfelt plea to always check the backs of products and read the labels, because fronts of products can’t be relied upon at all.
I’m sure we all get caught out sometimes, but the less often, the better!
PS: we write this, of course, before seeing the results of your voting. Maybe it won’t be a “Muir Glen Organic” sweep in the polls. But either way, it’s a call to vigilance, and a “very good, carry on” to everyone who does this already
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Beat Sugar Addiction Now! – by Dr. Jacob Teitelbaum & Chrystle Fiedler
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sugar isn’t often thought of as an addiction in the same category as alcohol or nicotine, but it’s actually very similar in some ways…
A bold claim, but: in each case, it has to do with dopamine responses to something that has:
- an adverse effect on our health,
- a quickly developed tolerance to same,
- and unpleasant withdrawal symptoms when quitting.
However, not all sugar addictions are created equal, and Dr. Teitelbaum lays four different types of sugar addiction out for us:
- Most related to “I need to perform and I need to perform now”
- Most related to “I just need something to get me through one more stressful day, again, just like every day before it”
- Most related to “ate too much sugar because of the above, and now a gut overgrowth of C. albicans is at the wheel”
- Most related to “ate too much sugar because of the above, and now insulin resistance is a problem that perpetuates itself too”
Of course, these may overlap, and indeed, they tend to stack cumulatively as time goes by.
However, Dr. Teitelbaum notes that as readers we may recognize ourselves as being at a particular point in the above, and there are different advices for each of them.
You thought it was just going to be about going cold turkey? Nope!
Instead, a multi-vector approach is recommended, including adjustments to sleep, nutrition, immune health, hormonal health, and more.
In short: if you’ve been trying to to kick the “White Death” habit as Gloria Swanson called it (sugar, that is, not the WW2 Finnish sniper of the same name—we can’t help you with that one), then this book is really much more helpful than others that take the “well, just don’t eat it, then” approach!
Pick up your copy of Beat Sugar Addiction Now from Amazon, and start your journey!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: