Foods Linked To Urinary Incontinence In Middle-Age (& Foods That Avert It)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Incontinence is an inconvenience associated with aging, especially for women. Indeed, as the study we’re going to talk about today noted:
❝Estrogen deficiency during menopause, aging, reproductive history, and factors increasing intra-abdominal pressure may lead to structural and functional failure in the pelvic floor.❞
However, that was just the “background”, before they got the study going, because…
❝Lifestyle choices, such as eating behavior, may contribute to pelvic floor disorders. The objective of the study was to investigate associations of eating behavior with symptoms of pelvic floor disorders, that is, stress urinary incontinence, urgency urinary incontinence, fecal incontinence, and constipation or defecation difficulties among middle-aged women.❞
~ Ibid.
How the study went
The researchers examined 1,098 Finnish women aged 47–55. It was a cross-sectional observational study, so no intervention was made, just: gathering data and analysing it. They examined:
- Eating behavior (i.e. what one’s diet is like; their questionnaire was quite comprehensive and the simplified conclusion doesn’t do that justice)
- Food consumption frequency (i.e. temporal patterns of eating)
- Demographic variables (e.g. age, education, etc)
- Gynecological variables (e.g. menopause status, hysterectomy, etc)
- Physical activity variables (e.g. light, moderate, heavy, previous history of no exercise, regular, competitive sport, etc)
With those things taken into account, the researchers crunched the numbers to assess the associations of dietary factors with pelvic floor disorders.
What they found
Adjusting for possible confounding variables…
- those with disordered eating patterns (e.g. overeating, restrictive eating, swinging between the two behaviors) were 50% higher chance of developing urinary incontinence than the norm
- those who more frequently consumed ready-made foods got 50% higher chance of developing urinary incontinence than the norm
- those who ate fruits daily enjoyed a 20% lower chance of urinary incontinence than the norm
So, in practical terms:
- practice mindful eating
- avoid ready-made foods
- enjoy fruit
You can read the paper in full here (it obviously goes into a lot more detail, and also covers other things beyond the scope of this article, such as fecal incontinence or, conversely, constipation—needless to say, the same advice stands in any case):
As for why this works the way it does: the study focused on the association and only hypothesized the question of “how”, but they did write a bit about that too, and it is almost certainly mostly a matter of gut health vs inflammation.
We really only have room for that kind of one-line summary here, but do read the paper if you’re interested, as it also talks about other dietary factors that had an impact, with the above-listed items being the topmost impactful factors, but for example (to take just one snippet of many possible ones):
❝In particular, saturated fatty acids (SFA) and cholesterol increased the risk for symptoms❞
~ Ibid. ← so do read it, for many more snippets like this!
What else does and doesn’t work
We covered a little while back the question of whether it is strengthening to hold one’s pee, or better to go whenever one feels the urge, and the answer is clear:
Meanwhile, supplements on the other hand are a mixed bag; there are some that probably help, and others, not so much:
What’s in the supplements that claim to help you cut down on bathroom breaks? And do they work?
Want to do more?
Check out these previous articles of ours:
Pelvic Floor Exercises (Not Kegels!) To Prevent Urinary Incontinence
and
Keeping Your Kidneys Happy: It’s About More Than Just Hydration! ← important at all ages, but especially relevant after 60
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Random Acts of Medicine – by Dr. Anupam Jena & Dr. Christopher Worsham
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We talked recently of small things that can change how productive your doctor’s appointment is, and this book is a more scientific version of that, and on a grander scale.
The author use what they call “natural experiments”, essentially observational studies, to determine what factors beyond the obvious affect health outcomes. With this approach, they address such questions as why kids with summer birthdays are more likely to get the flu, and why heart attack outcomes improve when there’s a cardiologists’ convention elsewhere. And many more such things that can seem like non-causal correlation, until one examines the causative factors, and controls (in the statistical analysis; remember this is still entirely observational, so no interventions are made) for other potential confounding factors.
They also look at what factors influence doctors’ decisions in ways they certainly shouldn’t, but they do, because doctors are as prone to biases as everyone else. And, for that matter, what factors influence patients’ decisions in ways they certainly shouldn’t—for the same reason. The authors acknowledge that they themselves are not immune, and you, dear reader, are not immune either.
Nevertheless, the practical value in this book comes from trying to at least be more aware of such things, the better to either leverage them, or at least ensure you don’t fall foul of them.
The style is conversational pop-science, making for quite light reading, albeit with many footnotes and a respectable bibliography.
Bottom line: if you’d like to understand more about the machinations that decide who lives and who dies (especially when sometimes it will be you or a loved one who lives or dies), then this is a fascinating book that that delves deeply into that.
Click here to check out Random Acts Of Medicine, and be aware!
Share This Post
-
ADHD For Smart Ass Women – by Tracy Otsuka
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about ADHD in adults before, what makes this one different? It’s the wholly female focus. Which is not to say some things won’t apply to men too, they will.
But while most books assume a male default unless it’s “bikini zone” health issues, this one is written by a woman for women focusing on the (biological and social) differences in ADHD for us.
A strength of the book is that it neither seeks to:
- over-medicalize things in a way that any deviation from the norm is inherently bad and must be fixed, nor
- pretend that everything’s a bonus, that we are superpowered and beautiful and perfect and capable and have no faults that might ever need addressing actually
…instead, it gives a good explanation of the ins and outs of ADHD in women, the strengths and weaknesses that this brings, and good solid advice on how to play to the strengths and reduce (or at least work around) the weaknesses.
Bottom line: this book has been described as “ADHD 2.0 (a very popular book that we’ve reviewed previously), but for women”, and it deserves that.
Click here to check out ADHD for Smart Ass Women, and fall in love with your neurodivergent brain!
Share This Post
-
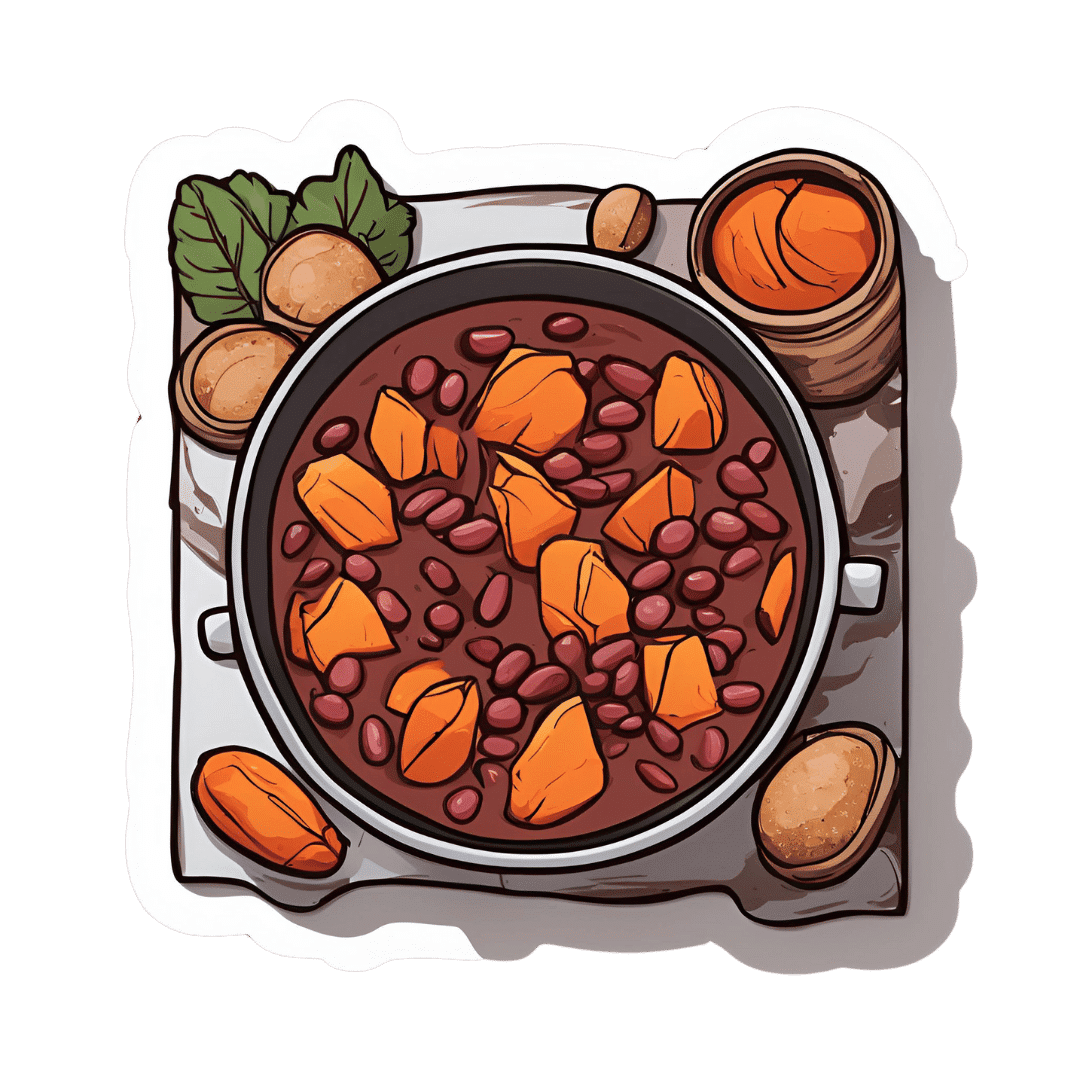
Ghanaian Red Bean & Sweet Potato Groundnut Stew
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a dish popular in principle throughout West Africa. We say “in principle” because that’s a big place, and there is a lot of regional variation. The archetypal peanut stew is from Senegal (as maafe) or Mali (as tigadèguèna), but for its more balanced nutritional profile we’ve chosen one from Ghana—and since there are regional variations within Ghana too, we should specify that this one is from the south.
If you are allergic to nuts, you can substitute a seed butter (or tahini) for the nut butter, and omit the nuts—this will work in culinary terms and be fine healthwise, but we can’t claim it would be the same dish, having lost its defining ingredient. If your allergy is solely to peanuts, then substituting with any oily nut would work. So, not almonds for example, but cashews or even walnuts would be fine.
You will need
- 1½ lbs sweet potatoes, peeled and cut into ½” cubes
- 2 cups low-sodium vegetable stock
- 2 cans kidney beans, drained, cooked, and rinsed (or 2 cups same; cooked, drained, and rinsed)
- 1 can chopped tomatoes
- ½ cup unsalted dry-roasted peanuts
- 1 onion, chopped
- 1 red bell pepper, deseeded and chopped
- ¼ bulb garlic, finely chopped
- 2 heaped tbsp unsalted peanut butter, minimal (ideally: no) additives
- 2 tsp white miso paste
- 2 tsp grated fresh ginger
- 1 tsp ground cumin
- 1 tsp cayenne pepper
- 1 tsp black pepper
- ½ tsp MSG or 1 tsp low-sodium salt
- ½ tsp coarsely ground nigella seeds
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a sauté pan, or other pan suitable for both frying and fitting the entire stew in. Fry the onions until softened, turn the heat down low, and add the garlic, ginger, red bell pepper, cumin, cayenne, black pepper, and MSG/salt.
2) Add ¼ cup of the vegetable stock, and the sweet potato, and turn the heat back up, on high for about 30 seconds to get it to temperature, and then take it down to a simmer.
3) Stir in the miso paste and chopped tomatoes.
4) Add most of the rest of the vegetable stock, keeping ¼ cup aside. Simmer for about 20 minutes.
5) Stir in the kidney beans, and simmer for about 30 minutes more—the sweet potato should be soft now; if it isn’t, let it simmer a while longer until it is.
6) Combine the peanut butter with the remaining ¼ cup vegetable stock, and blend until smooth. Stir it into the stew.
7) If the stew is looking more like a soup than a stew, take out 1 cup and blend this 1 cup to a purée, adding it back in.
8) Add half the peanuts unto the stew. Taste, and adjust the seasonings if necessary.
9) Crush the remaining peanuts using a pestle and mortar; not too much though; you want them broken into bits, not pulverised.
10) Garnish with the crushed nuts and nigella seeds, and serve.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat More (Of This) For Lower Blood Pressure
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we used 4/5 today!
Take care!
Share This Post
Related Posts
-
A New $16,000 Postpartum Depression Drug Is Here. How Will Insurers Handle It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A much-awaited treatment for postpartum depression, zuranolone, hit the market in December, promising an accessible and fast-acting medication for a debilitating illness. But most private health insurers have yet to publish criteria for when they will cover it, according to a new analysis of insurance policies.
The lack of guidance could limit use of the drug, which is both novel — it targets hormone function to relieve symptoms instead of the brain’s serotonin system, as typical antidepressants do — and expensive, at $15,900 for the 14-day pill regimen.
Lawyers, advocates, and regulators are watching closely to see how insurance companies will shape policies for zuranolone because of how some handled its predecessor, an intravenous form of the same drug called brexanolone, which came on the market in 2019. Many insurers required patients to try other, cheaper medications first — known as the fail-first approach — before they could be approved for brexanolone, which was shown in early trials reviewed by the FDA to provide relief within days. Typical antidepressants take four to six weeks to take effect.
“We’ll have to see if insurers cover this drug and what fail-first requirements they put in” for zuranolone, said Meiram Bendat, a licensed psychotherapist and an attorney who represents patients.
Most health plans have yet to issue any guidelines for zuranolone, and maternal health advocates worry that the few that have are taking a restrictive approach. Some policies require that patients first try and fail a standard antidepressant before the insurer will pay for zuranolone.
In other cases, guidelines require psychiatrists to prescribe it, rather than obstetricians, potentially delaying treatment since OB-GYN practitioners are usually the first medical providers to see signs of postpartum depression.
Advocates are most worried about the lack of coverage guidance.
“If you don’t have a published policy, there is going to be more variation in decision-making that isn’t fair and is less efficient. Transparency is really important,” said Joy Burkhard, executive director of the nonprofit Policy Center for Maternal Mental Health, which commissioned the study.
With brexanolone, which was priced at $34,000 for the three-day infusion, California’s largest insurer, Kaiser Permanente, had such rigorous criteria for prescribing it that experts said the policy amounted to a blanket denial for all patients, according to an NPR investigation in 2021.
KP’s written guidelines required patients to try and fail four medications and electroconvulsive therapy before they would be eligible for brexanolone. Because the drug was approved only for up to six months postpartum, and trials of typical antidepressants take four to six weeks each, the clock would run out before a patient had time to try brexanolone.
An analysis by NPR of a dozen other health plans at the time showed Kaiser Permanente’s policy on brexanolone to be an outlier. Some did require that patients fail one or two other drugs first, but KP was the only one that recommended four.
Miriam McDonald, who developed severe postpartum depression and suicidal ideation after giving birth in late 2019, battled Kaiser Permanente for more than a year to find effective treatment. Her doctors put her on a merry-go-round of medications that didn’t work and often carried unbearable side effects, she said. Her doctors refused to prescribe brexanolone, the only FDA-approved medication specifically for postpartum depression at the time.
“No woman should suffer like I did after having a child,” McDonald said. “The policy was completely unfair. I was in purgatory.”
One month after NPR published its investigation, KP overhauled its criteria to recommend that women try just one medication before becoming eligible for brexanolone.
Then, in March 2023, after the federal Department of Labor launched an investigation into the insurer — citing NPR’s reporting — the insurer revised its brexanolone guidelines again, removing all fail-first recommendations, according to internal documents recently obtained by NPR. Patients need only decline a trial of another medication.
“Since brexanolone was first approved for use, more experience and research have added to information about its efficacy and safety,” the insurer said in a statement. “Kaiser Permanente is committed to ensuring brexanolone is available when physicians and patients determine it is an appropriate treatment.”
“Kaiser basically went from having the most restrictive policy to the most robust,” said Burkhard of the Policy Center for Maternal Mental Health. “It’s now a gold standard for the rest of the industry.”
McDonald is hopeful that her willingness to speak out and the subsequent regulatory actions and policy changes for brexanolone will lead Kaiser Permanente and other health plans to set patient-friendly policies for zuranolone.
“This will prevent other women from having to go through a year of depression to find something that works,” she said.
Clinicians were excited when the FDA approved zuranolone last August, believing the pill form, taken once a day at home over two weeks, will be more accessible to women compared with the three-day hospital stay for the IV infusion. Many perinatal psychiatrists told NPR it is imperative to treat postpartum depression as quickly as possible to avoid negative effects, including cognitive and social problems in the baby, anxiety or depression in the father or partner, or the death of the mother to suicide, which accounts for up to 20% of maternal deaths.
So far, only one of the country’s six largest private insurers, Centene, has set a policy for zuranolone. It is unclear what criteria KP will set for the new pill. California’s Medicaid program, known as Medi-Cal, has not yet established coverage criteria.
Insurers’ policies for zuranolone will be written at a time when the regulatory environment around mental health treatment is shifting. The U.S. Department of Labor is cracking down on violations of the Mental Health Parity and Addiction Equity Act of 2008, which requires insurers to cover psychiatric treatments the same as physical treatments.
Insurers must now comply with stricter reporting and auditing requirements intended to increase patient access to mental health care, which advocates hope will compel health plans to be more careful about the policies they write in the first place.
In California, insurers must also comply with an even broader state mental health parity law from 2021, which requires them to use clinically based, expert-recognized criteria and guidelines in making medical decisions. The law was designed to limit arbitrary or cost-driven denials for mental health treatments and has been hailed as a model for the rest of the country. Much-anticipated regulations for the law are expected to be released this spring and could offer further guidance for insurers in California setting policies for zuranolone.
In the meantime, Burkhard said, patients suffering from postpartum depression should not hold back from asking their doctors about zuranolone. Insurers can still grant access to the drug on a case-by-case basis before they formalize their coverage criteria.
“Providers shouldn’t be deterred from prescribing zuranolone,” Burkhard said.
This article is from a partnership that includes KQED, NPR and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Taking A Trip Through The Evidence On Psychedelics
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
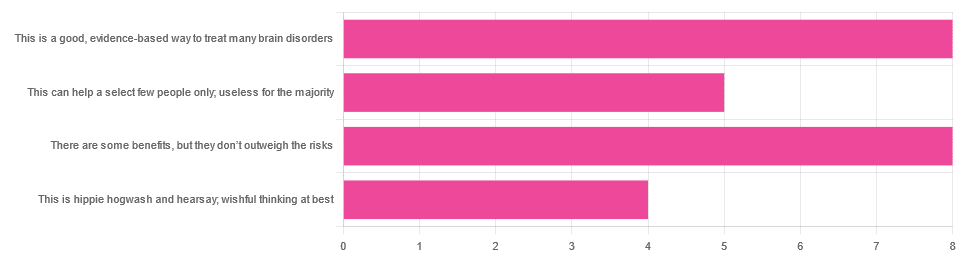
In Tuesday’s newsletter, we asked you for your opinions on the medicinal use of psychedelics, and got the above-depicted, below-described, set of responses:
- 32% said “This is a good, evidence-based way to treat many brain disorders”
- 32% said “There are some benefits, but they don’t outweigh the risks”
- 20% said “This can help a select few people only; useless for the majority”
- 16% said “This is hippie hogwash and hearsay; wishful thinking at best”
Quite a spread of answers, so what does the science say?
This is hippie hogwash and hearsay; wishful thinking at best! True or False?
False! We’re tackling this one first, because it’s easiest to answer:
There are some moderately-well established [usually moderate] clinical benefits from some psychedelics for some people.
If that sounds like a very guarded statement, it is. Part of this is because “psychedelics” is an umbrella term; perhaps we should have conducted separate polls for psilocybin, MDMA, ayahuasca, LSD, ibogaine, etc, etc.
In fact: maybe we will do separate main features for some of these, as there is a lot to say about each of them separately.
Nevertheless, looking at the spread of research as it stands for psychedelics as a category, the answers are often similar across the board, even when the benefits/risks may differ from drug to drug.
To speak in broad terms, if we were to make a research summary for each drug it would look approximately like this in each case:
- there has been research into this, but not nearly enough, as “the war on drugs” may well have manifestly been lost (the winner of the war being: drugs; still around and more plentiful than ever), but it did really cramp science for a few decades.
- the studies are often small, heterogenous (often using moderately wealthy white student-age population samples), and with a low standard of evidence (i.e. the methodology often has some holes that leave room for reasonable doubt).
- the benefits recorded are often small and transient.
- in their favor, though, the risks are also generally recorded as being quite low, assuming proper safe administration*.
*Illustrative example:
Person A takes MDMA in a club, dances their cares away, has had only alcohol to drink, sweats buckets but they don’t care because they love everyone and they see how we’re all one really and it all makes sense to them and then they pass out from heat exhaustion and dehydration and suffer kidney damage (not to mention a head injury when falling) and are hospitalized and could die;
Person B takes MDMA in a lab, is overwhelmed with a sense of joy and the clarity of how their participation in the study is helping humanity; they want to hug the researcher and express their gratitude; the researcher reminds them to drink some water.
Which is not to say that a lab is the only safe manner of administration; there are many possible setups for supervised usage sites. But it does mean that the risks are often as much environmental as they are risks inherent to the drug itself.
Others are more inherent to the drug itself, such as adverse cardiac events for some drugs (ibogaine is one that definitely needs medical supervision, for example).
For those who’d like to see numbers and clinical examples of the bullet points we gave above, here you go; this is a great (and very readable) overview:
NIH | Evidence Brief: Psychedelic Medications for Mental Health and Substance Use Disorders
Notwithstanding the word “brief” (intended in the sense of: briefing), this is not especially brief and is rather an entire book (available for free, right there!), but we do recommend reading it if you have time.
This can help a select few people only; useless for the majority: True or False?
True, technically, insofar as the evidence points to these drugs being useful for such things as depression, anxiety, PTSD, addiction, etc, and estimates of people who struggle with mental health issues in general is often cited as being 1 in 4, or 1 in 5. Of course, many people may just have moderate anxiety, or a transient period of depression, etc; many, meanwhile, have it worth.
In short: there is a very large minority of people who suffer from mental health issues that, for each issue, there may be one or more psychedelic that could help.
This is a good, evidence-based way to treat many brain disorders: True or False?
True if and only if we’re willing to accept the so far weak evidence that we discussed above. False otherwise, while the jury remains out.
One thing in its favor though is that while the evidence is weak, it’s not contradictory, insofar as the large preponderance of evidence says such therapies probably do work (there aren’t many studies that returned negative results); the evidence is just weak.
When a thousand scientists say “we’re not completely sure, but this looks like it helps; we need to do more research”, then it’s good to believe them on all counts—the positivity and the uncertainty.
This is a very different picture than we saw when looking at, say, ear candling or homeopathy (things that the evidence says simply do not work).
We haven’t been linking individual studies so far, because that book we linked above has many, and the number of studies we’d have to list would be:
n = number of kinds of psychedelic drugs x number of conditions to be treated
e.g. how does psilocybin fare for depression, eating disorders, anxiety, addiction, PTSD, this, that, the other; now how does ayahuasca fare for each of those, and so on for each drug and condition; at least 25 or 30 as a baseline number, and we don’t have that room.
But here are a few samples to finish up:
- Psilocybin as a New Approach to Treat Depression and Anxiety in the Context of Life-Threatening Diseases—A Systematic Review and Meta-Analysis of Clinical Trials
- Therapeutic Use of LSD in Psychiatry: A Systematic Review of Randomized-Controlled Clinical Trials
- Efficacy of Psychoactive Drugs for the Treatment of Posttraumatic Stress Disorder: A Systematic Review of MDMA, Ketamine, LSD and Psilocybin
- Changes in self-rumination and self-compassion mediate the effect of psychedelic experiences on decreases in depression, anxiety, and stress.
- Psychedelic Treatments for Psychiatric Disorders: A Systematic Review and Thematic Synthesis of Patient Experiences in Qualitative Studies
- Repeated lysergic acid diethylamide (LSD) reverses stress-induced anxiety-like behavior, cortical synaptogenesis deficits and serotonergic neurotransmission decline
In closing…
The general scientific consensus is presently “many of those drugs may ameliorate many of those conditions, but we need a lot more research before we can say for sure”.
On a practical level, an important take-away from this is twofold:
- drugs, even those popularly considered recreational, aren’t ontologically evil, generally do have putative merits, and have been subject to a lot of dramatization/sensationalization, especially by the US government in its famous war on drugs.
- drugs, even those popularly considered beneficial and potentially lifechangingly good, are still capable of doing great harm if mismanaged, so if putting aside “don’t do drugs” as a propaganda of the past, then please do still hold onto “don’t do drugs alone”; trained professional supervision is a must for safety.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Not To Get Sick: A Cookbook – by Dr. Benjamin Bikman and Diana Keuilian
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Dr. Bikman’s excellent “Why We Get Sick”, and if you haven’t read that yet, we recommend doing so.
Nevertheless, you don’t need to have read it to benefit from this one, which is about cooking with those learnings (from the other book) in mind.
Before getting to the recipes, we get a section recapping what we learned previously, as well as adding some more general lifestyle advices beyond the kitchen. The science is also expanded a bit, to include such things as the two-way relationship between insulin and aging, as well as the interplay with other metrics of health, including blood lipids, for example.
The authors then provide a plan, in the three stages: reverse (insulin resistance), prevent (insulin resistance), maintain (insulin sensitivity).
The recipes themselves, of which there are 70, are of course tailored to do the above three things; they’re also quite diverse, albeit if you are vegetarian or vegan, you should know in advance that most of these recipes are not.
Bottom line: if the above doesn’t apply to you, and you would like to improve your insulin sensitivity, this book can indeed help.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: