Food and Nutrition – by Dr. P.K. Newby
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The “What Everyone Needs To Know” part of the title is the name of a series of books, of which this one, “Food and Nutrition”, is one.
In this case, the title is apt, and/or could have been “What Everyone Really Should Know”, or “What Everyone Would Like To Think They Know But Have Often Just Been Bluffing Their Way Through The Supermarket Aisles”.
The chapter and section headings are all in the forms of questions, such that all-together in such volume in the table of contents, they’re reminiscent of the “Jonathan Frakes Asks You Things” meme.
But, this serves a dual purpose—for one, it makes the whole book one big FAQ, which is a very convenient format. Furthermore, it prompts a little thought on the part of the reader before each section, if we indeed question for ourselves:
- Are fertilizers in farming friend or foe?
- How have the Digital Revolution and Information Age impacted our diet?
- Are canned and frozen foods inferior to fresh?
- Does snacking or meal timing matter?
- What are cereal grains and “pseudograins”?
…And so many more. But what’s best about this is:
Dr. Newby doesn’t reference her own preferences, or even have a particular way of eating she’d like us to adopt. She just lays out the science to answer each question, as discovered by high-quality studies and a general weight of evidence.
Bottom line: this book can level-up your nutritional knowledge from bluffing to really knowing! A worthy addition to anyone’s bookshelf.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Climate Change Threatens the Mental Well-Being of Youths. Here’s How To Help Them Cope.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve all read the stories and seen the images: The life-threatening heat waves. The wildfires of unprecedented ferocity. The record-breaking storms washing away entire neighborhoods. The melting glaciers, the rising sea levels, the coastal flooding.
As California wildfires stretch into the colder months and hurricane survivors sort through the ruins left by floodwaters, let’s talk about an underreported victim of climate change: the emotional well-being of young people.
A nascent but growing body of research shows that a large proportion of adolescents and young adults, in the United States and abroad, feel anxious and worried about the impact of an unstable climate in their lives today and in the future.
Abby Rafeek, 14, is disquieted by the ravages of climate change, both near her home and far away. “It’s definitely affecting my life, because it’s causing stress thinking about the future and how, if we’re not addressing the problem now as a society, our planet is going to get worse,” says Abby, a high school student who lives in Gardena, California, a city of 58,000 about 15 miles south of downtown Los Angeles.
She says wildfires are a particular worry for her. “That’s closer to where I live, so it’s a bigger problem for me personally, and it also causes a lot of damage to the surrounding areas,” she says. “And also, the air gets messed up.”
In April, Abby took a survey on climate change for kids ages 12-17 during a visit to the emergency room at Children’s Hospital of Orange County.
Rammy Assaf, a pediatric emergency physician at the hospital, adapted the survey from one developed five years ago for adults. He administered his version last year to over 800 kids ages 12-17 and their caregivers. He says initial results show climate change is a serious cause of concern for the emotional security and well-being of young people.
Assaf has followed up with the kids to ask more open-ended questions, including whether they believe climate change will be solved in their lifetimes; how they feel when they read about extreme climate events; what they think about the future of the planet; and with whom they are able to discuss their concerns.
“When asked about their outlook for the future, the first words they will use are helpless, powerless, hopeless,” Assaf says. “These are very strong emotions.”
Assaf says he would like to see questions about climate change included in mental health screenings at pediatricians’ offices and in other settings where children get medical care. The American Academy of Pediatrics recommends that counseling on climate change be incorporated into the clinical practice of pediatricians and into medical school curriculums, but not with specific regard to mental health screening.
Assaf says anxiety about climate change intersects with the broader mental health crisis among youth, which has been marked by a rise in depression, loneliness, and suicide over the past decade, though there are recent signs it may be improving slightly.
A 2022 Harris Poll of 1,500 U.S. teenagers found that 89% of them regularly think about the environment, “with the majority feeling more worried than hopeful.” In addition, 69% said they feared they and their families would be affected by climate change in the near future. And 82% said they expected to have to make key life decisions — including where to live and whether to have children — based on the state of the environment.
And the impact is clearly not limited to the U.S. A 2021 survey of 10,000 16- to 25-year-olds across 10 countries found “59% were very or extremely worried and 84% were at least moderately worried” about climate change.
Susan Clayton, chair of the psychology department at the College of Wooster in Ohio, says climate change anxiety may be more pronounced among younger people than adults. “Older adults didn’t grow up being as aware of climate change or thinking about it very much, so there’s still a barrier to get over to accept it’s a real thing,” says Clayton, who co-created the adult climate change survey that Assaf adapted for younger people.
By contrast, “adolescents grew up with it as a real thing,” Clayton says. “Knowing you have the bulk of your life ahead of you gives you a very different view of what your life will be like.” She adds that younger people in particular feel betrayed by their government, which they don’t think is taking the problem seriously enough, and “this feeling of betrayal is associated with greater anxiety about the climate.”
Abby believes climate change is not being addressed with sufficient resolve. “I think if we figure out how to live on Mars and explore the deep sea, we could definitely figure out how to live here in a healthy environment,” she says.
If you are a parent whose children show signs of climate anxiety, you can help.
Louise Chawla, professor emerita in the environmental design program at the University of Colorado-Boulder, says the most important thing is to listen in an open-ended way. “Let there be space for kids to express their emotions. Just listen to them and let them know it’s safe to express these emotions,” says Chawla, who co-founded the nonprofit Growing Up Boulder, which works with the city’s schools to encourage kids to engage civically, including to help shape their local environment.
Chawla and others recommend family activities that reinforce a commitment to the environment. They can be as simple as walking or biking and participating in cleanup or recycling efforts. Also, encourage your children to join activities and advocacy efforts sponsored by environmental, civic, or religious organizations.
Working with others can help alleviate stress and feelings of powerlessness by reassuring kids they are not alone and that they can be proactive.
Worries about climate change should be seen as a learning opportunity that might even lead some kids to their life’s path, says Vickie Mays, professor of psychology and health policy at UCLA, who teaches a class on climate change and mental health — one of eight similar courses offered recently at UC campuses.
“We should get out of this habit of ‘everything’s a mental health problem,’” Mays says, “and understand that often a challenge, a stress, a worry can be turned into advocacy, activism, or a reach for new knowledge to change the situation.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
Treadmill vs Road
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Why do I get tired much more quickly running outside, than I do on the treadmill? Every time I get worn out quickly but at home I can go for much longer!❞
Short answer: the reason is Newton’s laws of motion.
In other words: on a treadmill, you need only maintain your position in space relative the the Earth while the treadmill moves beneath you, whereas on the road, you need to push against the Earth with sufficient force to move it relative to your body.
Illustrative thought experiment to make that clearer: if you were to stand on a treadmill with roller skates, and hold onto the bar with even just one finger, you would maintain your speed as far as the treadmill’s computer is concerned—whereas to maintain your speed on a flat road, you’d still need to push with your back foot every few yards or so.
More interesting answer: it’s a qualitatively different exercise (i.e. not just quantitively different). This is because of all that pushing you’re having to do on the road, while on a treadmill, the only pushing you have to do is just enough to counteract gravity (i.e. to keep you upright).
As such, both forms of running are a cardio exercise (because simply moving your legs quickly, even without having to apply much force, is still something that requires oxygenated blood feeding the muscles), but road-running adds an extra element of resistance exercise for the muscles of your lower body. Thus, road-running will enable you to build-maintain muscle much more than treadmill-running will.
Some extra things to bear in mind, however:
1) You can increase the resistance work for either form of running, by adding weight (such as by wearing a weight vest):
Weight Vests Against Osteoporosis: Do They Really Build Bone?
…and while road-running will still be the superior form of resistance work (for the reasons we outlined above), adding a weight vest will still be improving your stabilization muscles, just as it would if you were standing still while holding the weight up.
2) Stationary cycling does not have the same physics differences as stationary running. By this we mean: an exercise bike will require your muscles to do just as much pushing as they would on a road. This makes stationary cycling an excellent choice for high intensity resistance training (HIRT):
3) The best form of exercise is the one that you will actually do. Thus, when it’s raining sidewise outside, a treadmill inside will get exercise done better than no running at all. Similarly, a treadmill exercise session takes a lot less preparation (“switch it on”) than a running session outside (“get dressed appropriately for the weather, apply sunscreen if necessary, remember to bring water, etc etc”), and thus is also much more likely to actually occur. The ability to stop whenever one wants is also a reassuring factor that makes one much more likely to start. See for example:
How To Do HIIT (Without Wrecking Your Body)
Take care!
Share This Post
-
The Emperor’s New Klotho, Or Something More?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Unzipping The Genes Of Aging?
Klotho is an enzyme encoded in humans’ genes—specifically, in the KL gene.
It’s found throughout all living parts of the human body (and can even circulate about in its hormonal form, or come to rest in its membranaceous form), and its subgroups are especially found:
- α-klotho: in the brain
- β-klotho: in the liver
- γ-klotho: in the kidneys
Great! Why do we care?
Klotho, its varieties and variants, its presence or absence, are very important in aging.
Almost every biological manifestation of aging in humans has some klotho-related indicator; usually the decrease or mutation of some kind of klotho.
Which way around the cause and effect go has been the subject of much debate and research: do we get old because we don’t have enough klotho, or do we make less klotho because we’re getting old?
Of course, everything has to be tested per variant and per system, so that can take a while (punctuated by research scientists begging for more grants to do the next one). Given that it’s about aging, testing in humans would take an incredibly long while, so most studies so far have been rodent studies.
The general gist of the results of rodent studies is “reduced klotho hastens aging; increased klotho slows it”.
(this can be known by artificially increasing or decreasing the level of klotho expression, again something easier in mice as it is harder to arrange transgenic humans for the studies)
Here’s one example of many, of that vast set of rodent studies:
Suppression of Aging in Mice by the Hormone Klotho
Relevance for Alzheimer’s, and a science-based advice
A few years ago (2020), an Alzheimer’s study was undertaken; they noted that the famous apolipoprotein E4 (apoE4) allele is the strongest genetic risk factor for Alzheimer’s, and that klotho may be another. FGF21 (secreted by the liver, mostly during fasting) binds to its own receptor (FGFR1) and its co-receptor β-klotho. Since this is a known neuroprotective factor, they wondered whether klotho itself may interact with β-amyloid (Aβ), and found:
❝Aβ can enhance the ability of klotho to draw FGF21 to regions of incipient neurodegeneration in AD❞
In other words: β-amyloid, the substance whose accumulation is associated with neurodegeneration in Alzheimer’s disease, is a mediator in klotho bringing a known neuroprotective factor, FGF21, to the areas of neurodegeneration
In fewer words: klotho calls the firefighters to the scene of the fire
Read more: Alignment of Alzheimer’s disease amyloid β-peptide and klotho
The advice based on this? Consider practicing intermittent fasting, if that is viable for you, as it will give your liver more FGF21-secreting time, and the more FGF21, the more firefighters arrive when klotho sounds the alarm.
See also: Intermittent Fasting: What’s the truth?
…and while you’re at it:
Does intermittent fasting have benefits for our brain?
A more recent (2023) study with a slightly different (but connected) purpose, found results consistent with this:
Longevity factor klotho enhances cognition in aged nonhuman primates
…and, for that matter this (2023) study that found:
Associations between klotho and telomere biology in high stress caregivers
…which looks promising, but we’d like to see it repeated with a sounder method (they sorted caregiving into “high-stress” and “low-stress” depending on whether a child was diagnosed with ASD or not, which is by no means a reliable way of sorting this). They did ask for reported subjective stress levels, but to be more objective, we’d like to see clinical markers of stress (e.g. cortisol levels, blood pressure, heart rate changes, etc).
A very recent (April 2024) study found that it has implications for more aspects of aging—and this time, in humans (but using a population-based cohort study, rather than lab conditions):
Can I get it as a supplement?
Not with today’s technology and today’s paucity of clinical trials, you can’t. Maybe in the future!
However… The presence of senescent (old, badly copied, stumbling and staggering onwards when they should have been killed and eaten and recycled already) cells actively reduces klotho levels, which means that taking supplements that are senolytic (i.e., that kill those senescent cells) can increase serum klotho levels:
Orally-active, clinically-translatable senolytics restore α-Klotho in mice and humans
Ok, what can I take for that?
We wrote about a senolytic supplement that you might enjoy, recently:
Fisetin: The Anti-Aging Assassin
Want to know more?
If you have the time, Dr. Peter Attia interviews Dr. Dena Dubal (researcher in several of the above studies) here:
Click Here If The Embedded Video Doesn’t Load Automatically
Enjoy!
Share This Post
Related Posts
-
The “Yes I Can” Salad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sometimes, we are given to ask ourselves: “Can I produce a healthy and tasty salad out of what I have in?” and today we show how, with a well-stocked pantry, the answer is “yes I can”, regardless of what is (or isn’t) in the fridge.
You will need
- 1 can cannellini beans, drained
- 1 can sardines (if vegetarian/vegan, substitute ½ can chickpeas, drained)
- 1 can mandarin segments
- 1 handful pitted black olives, from a jar (or from a can, if you want to keep the “yes I can” theme going)
- ½ red onion, thinly sliced (this can be from frozen, defrosted—sliced/chopped onion is always a good thing to have in your freezer, by the way; your writer here always has 1–6 lbs of chopped onions in hers, divided into 1lb bags)
- 1 oz lemon juice
- 1 tbsp chopped parsley (this can be freeze-dried, but fresh is good if you have it)
- 1 tbsp extra virgin olive oil
- 1 tbsp chia seeds
- 1 tsp miso paste
- 1 tsp honey (omit if you don’t care for sweetness; substitute with agave nectar if you do like sweetness but don’t want to use honey specifically)
- 1 tsp red chili flakes
Method
(we suggest you read everything at least once before doing anything)
1) Combine the onion and the lemon juice in a small bowl, massaging gently
2) Mix (in another bowl) the miso paste with the chili flakes, chia seeds, honey, olive oil, and the spare juice from the can of mandarin segments, and whisk it to make a dressing.
3) Add the cannellini beans, sardines (break them into bite-size chunks), mandarin segments, olives, and parsley, tossing them thoroughly (but gently) in the dressing.
4) Top with the sliced onion, discarding the excess lemon juice, and serve:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Three Daily Servings of Beans?
- We Are Such Stuff As Fish Are Made Of
- Chia: The Tiniest Seeds With The Most Value
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
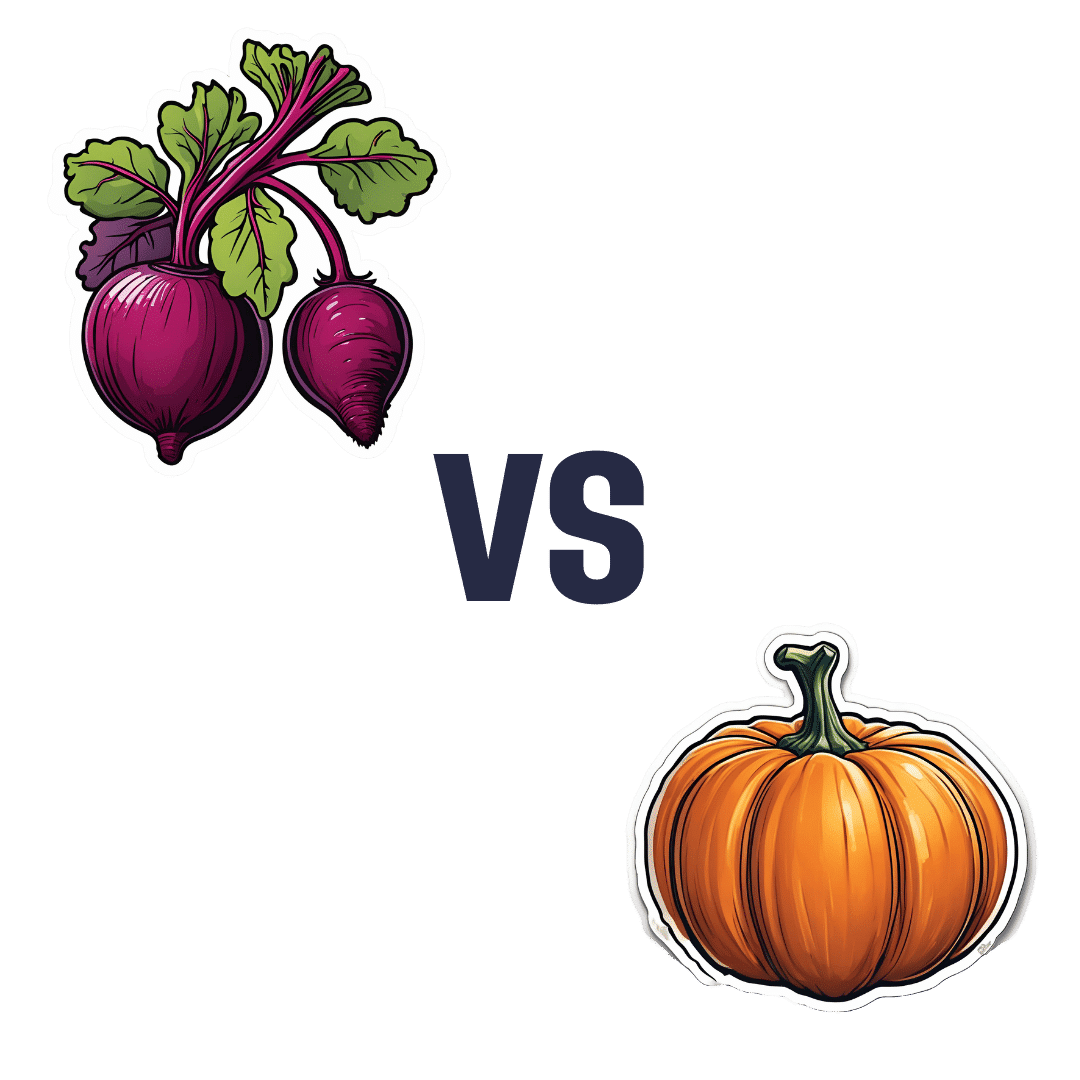
Beetroot vs Pumpkin – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing beetroot to pumpkin, we picked the beetroot.
Why?
It was close! And an argument could be made for either.
In terms of macros, beetroot has about 3x more protein and about 3x more fiber, as well as about 2x more carbs, making it the “more food per food” option. While both have a low glycemic index, we picked the beetroot here for its better numbers overall.
In the category of vitamins, beetroot has more of vitamins B6 and B9, while pumpkin has more of vitamins A, B2, B3, B5, E, and K. So, a fair win for pumpkin this time.
When it comes to minerals, though, beetroot has more calcium, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while pumpkin has a tiny bit more copper. An easy win for beetroot here.
In short, both are great, and although pumpkin shines in the vitamin category, beetroot wins on overall nutritional density.
Want to learn more?
You might like to read:
No, beetroot isn’t vegetable Viagra. But here’s what it can do
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Who Initiates Sex & Why It Matters
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In an ideal world, it wouldn’t matter any more than who first says “let’s get something to eat” when hungry. But in reality, it can cause serious problems on both sides:
Fear and loathing?
The person who initiates gets the special prize of an n% chance of experiencing rejection, and then what? Try again, and again, and risk seeming pushy? Or leave the ball in the other person’s court, where it may then go untouched for the next few months, because (in the most positive scenario) they were waiting for you to initiate at a better time for them?
The person who does not initiate, and/but does not want sex at that time, gets the special prize of either making their partner feel unwanted, insecure, and perhaps unloved, or else grudgingly consenting to sex that’s going to be no fun while your heart’s not in it, and thus create the same end result plus you had an extra bad experience?
So, that sucks all around:
- Initiating touch (sex or cuddling) can feel like a test of being wanted, whereupon a lack of initiation or response may be misinterpreted as a lack of love or appreciation.
- Meanwhile, non-reciprocation might stem from exhaustion or unrelated issues. For many, it’s a physiological lottery.
10almonds note: not discussed in this video, but for many couples, problems can also arise because one partner or another just isn’t showing up with the expected physical signs of physiological arousal, so even if they say (and mean!) an enthusiastic “yes”, their body’s signs get misread as a “not really, though”, resulting in one partner feeling rejected, and both feeling inadequate—on account of something that was completely unrelated to how the person actually felt about the prospect of sex*.
*Sometimes, physiological arousal will simply not accompany psychological arousal, no matter how sincere the latter. And on the flipside, sometimes the signs of physiological arousal will just show up without psychological arousal. The human body is just like that sometimes. We all must listen to our partners’ words, not their genitals!
The solution to this problem is thus the same as the solution to the rest of the problem that is discussed in the video, and it’s: good communication.
That can be easier said than done, of course—not everyone is at their most eloquent in such situations! Which is why it can be important to have those conversations first outside of the bedroom when the stakes are low/non-existent.
Even with the best communication, a more general, overarching non-reciprocity (real or perceived) of sexual desire can cause bitterness, resentment, and can ultimately be relationship-ending if a resolution that’s acceptable to everyone involved is not found.
Ultimately, the work as a couple must begin from within as individuals—addressing self-worth issues to better navigate love and intimacy.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Relationships: When To Stick It Out & When To Call It Quits
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: