Fatigue? Unexplained weight gain and dry skin? Could it be Hashimoto’s disease?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Maybe you feel worn out. Perhaps you’re also having trouble losing weight. Generally, you just don’t feel 100%.
Could it be Hashimoto’s disease? This common autoimmune thyroid disorder is when your immune system (which fights off viruses and bacteria), mistakenly attacks a part of your body. In this case, it’s your thyroid – a gland located at the base of your neck – and can cause low thyroid hormones levels (hypothyroidism).
Hypothyroidism affects one in 33 Australians and Hashimoto’s is one of the most common thyroid conditions in first-world countries.
While symptoms can be subtle, untreated Hashimoto’s can cause long-term problems with your heart, memory and fertility. Here is what you need to know.
What happens when you have Hashimoto’s?
Your thyroid gland is a butterfly-shaped gland in the neck. It is essential in regulating things like muscle function, digestion, metabolism, the heart and lungs. In children, thyroid hormones are also needed for normal growth and development.
Hashimoto’s thyroid disease, named after the Japanese doctor who discovered it in 1912, is also known as Hashimoto’s thyroiditis or chronic lymphocytic thyroiditis. The disease can cause the immune system to mistakenly produce proteins called antibodies (thyroid peroxidase and thyroglobulin). These can cause inflammation and long-term damage to the thyroid gland. Over time, as thyroid tissue is inflamed and/or destroyed, there can be a decrease in the production of thyroid hormones (hypothyroidism).
Hashimoto’s can present subtly at first. If you only have antibodies with no change in thyroid levels, it is likely you won’t have any symptoms.
However, as the disease progresses, you may experience fatigue, weight gain (or difficulty losing weight), increased sensitivity to the cold, constipation, dry skin, muscle aches, irregular or heavy menstrual cycles, enlarged thyroid (goitre) and occasionally hair loss, including at the ends of your eyebrows.
What causes Hashimoto’s thyroid disease?
Several risk factors can contribute to the development of Hashimoto’s including:
-
genetic risk – your risk is higher if you have family members with Hashimoto’s
-
gender – women are up to ten times more likely than men to develop the disease
-
age – you are more likely to develop the disease from 30 to 50 years of age
-
autoimmune condition – having another autoimmune condition like systemic lupus, Type 1 diabetes and celiac disease increases your risk
-
excessive iodine intake and radiation exposure may also increase risk in people who are already genetically at greater risk.
What are the long-term risks?
Long-term, untreated Hashimoto’s thyroiditis can cause heart issues, higher cholesterol levels, nerve damage (peripheral neuropathy), reduced cognition and infertility.
In pregnancy, Hashimoto’s has a higher risk of pre-eclampsia (high blood pressure affecting several organs), premature birth, placental abruption (when the placenta separates from the inner wall of the uterus before birth) and, in severe cases, pregnancy loss.
The disease has also been linked with an increased risk (but low incidence) of the lymphocytes of the thyroid turning into cancer cells to cause thyroid lymphoma.
How is Hashimoto’s diagnosed?
Diagnosis can be confirmed with a blood test to check thyroid levels and antibodies.
Thyroid peroxidase antibodies are commonly present but about 5% of patients test antibody-negative. In those people, diagnosis depends on the thyroid levels, clinical presentation and ultrasound appearance of general inflammation. An ultrasound may not be required though, especially if the diagnosis is obvious.
Three hormone levels are tested to determine if you have Hashimoto’s.
Thyroid stimulating hormone (TSH) is produced by the brain to speak to the thyroid, telling it to produce two types of thyroid hormones – T3 and T4.
If you have either relative or absolute thyroid hormone deficiency, a test will show the stimulating hormones as high because the brain is trying to get the thyroid to work harder.
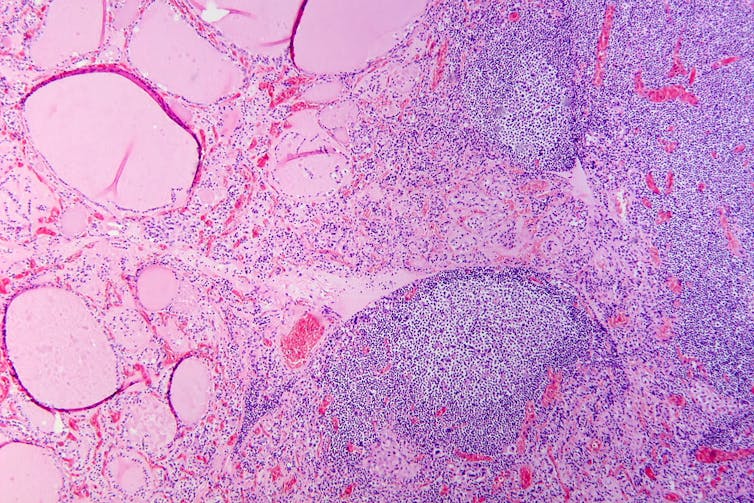
Patho/Wikimedia Commons, CC BY-SA
Can it be treated?
The management of Hashimoto’s depends on the severity of the thyroid levels. Up to 20% of the population can have antibodies but normal thyroid levels. This is still Hashimoto’s thyroid disease, but it is very mild and does not require treatment. There is no current treatment to reduce antibody levels alone.
Because thyroid peroxidase antibodies increase the risk of abnormal thyroid levels in the future, regular thyroid testing is recommended.
When the thyroid stimulating hormone is high with normal thyroid hormone levels it is termed “subclinical hypothyroidism”. When it is paired with low hormone levels it is called “overt hypothyroidism”. The first is a mild form of the disease and treatment depends on the degree of stimulating hormone elevation.
Overt hypothyroidism warrants treatment. The main form of this is thyroid hormone replacement therapy (levothyroxine) with the dose of the drug adjusted until thyroid levels are within the normal range. This is usually a lifelong treatment but, once the dose is optimised, hormone levels usually remain relatively stable.
In some people with very enlarged thyroid glands causing compressive symptoms (such as difficulty swallowing or breathing), thyroidectomy (surgical removal of the thyroid) is considered.
Hashimoto’s thyroiditis is a common condition caused by your body’s immune system incorrectly damaging to your thyroid and can go undetected. Long-term, untreated, it can cause issues with your heart, cognition, and fertility. It can be diagnosed with a simple blood test. Speak to your doctor if you have any concerns as early diagnosis and treatment can help prevent complications.
Aakansha Zala, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is ADHD Being Over-Diagnosed For Cash?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is ADHD Being Systematically Overdiagnosed?
The BBC’s investigative “Panorama” program all so recently did a documentary in which one of their journalists—who does not have ADHD—went to three private clinics and got an ADHD diagnosis from each of them:
- The BBC documentary: Private ADHD Clinics Exposed (28 mins)
- Their “5 Minutes” version: ADHD Undercover: How I Was Misdiagnosed (6 mins)
So… Is it really a case of show up, pay up, and get a shiny new diagnosis?
The BBC Panorama producers cherry-picked 3 private providers, and during those clinical assessments, their journalist provided answers that would certainly lead to a diagnosis.
This was contrasted against a three-hour assessment with an NHS psychiatrist—something that rarely happens in the NHS. Which prompts the question…
How did he walk into a 3-hour psychiatrist assessment, when most people have to wait in long waiting lists for a much more cursory appointment first with assorted gatekeepers, before going on another long waiting list, for an also-much-shorter appointment with a psychiatrist?
That would be because the NHS psychiatrist was given advance notification that this was part of an investigation and would be filmed (the private clinics were not gifted the same transparency)
So, maybe just a tad unequal treatment!
In case you’re wondering, here’s what that very NHS psychiatrist had to say on the topic:
Is it really too easy to be diagnosed with ADHD?
(we’ll give you a hint—remember Betteridge’s Law!)
❝Since the documentary aired, I have heard from people concerned that GPs could now be more likely to question legitimate diagnoses.
But as an NHS psychiatrist it is clear to me that the root of this issue is not overdiagnosis.
Instead, we are facing the combined challenges of remedying decades of underdiagnosis and NHS services that were set up when there was little awareness of ADHD.❞
~ Dr. Mike Smith, Psychiatrist
The ADHD foundation, meanwhile, has issued its own response, saying:
❝We are disappointed that BBC Panorama has opted to broadcast a poorly researched, sensationalist piece of television journalism.❞
Share This Post
-
The Healing of America – by Thomas Reid
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First let’s be clear: this is about the US healthcare system, and thus will be mostly relevant for US Americans. Still, many outside of the US may have an interest, and in fact the book does talk about the healthcare systems of many other countries (hence the subtitle mentioning “a global quest”), outlining how each works, and what the journey was that got them there.
The author, a veteran journalist with a 60+ year-long career, notes that affordable healthcare is a social problem so complex, that only 33 out of 32 of the world’s richest countries have managed to do it. That’s a little glib and can be quibbled in the minutiae, but when it comes down to it, insulin in the US still costs 50x what it does in most places, and in pretty much all aspects of healthcare, US Americans are being fleeced at every turn.
He examines why this happens, and what currently prevents the US from lowering healthcare costs. He finds the culprits to be the profitmongers along the way (insurance companies in cahoots with drug companies in cahoots with hospitals, etc), as well as a pervasive belief that since healthcare is so expensive, how could the richest country on Earth possibly pay for it? Many Americans will believe that the answer is that other countries have inferior care, but this tends to stem from a mistaken belief that medical treatment actually costs what Americans are billed for it. The fact is: the same quality of care can be provided for a lot less, as many countries demonstrate.
The book doesn’t argue for any one particular solution; it doesn’t have to be entirely state-funded like the UK, or consumer-funded but seriously low price caps like in Japan; there are many other models to choose from. The argument that is made is that if so many other countries can have medical bankruptcy being a thing unheard-of instead of the leading cause of bankruptcy, then so can the US, and here’s a wide menu of methods to choose from.
Bottom line: if you’re a US American and you’d like to think you could get the same quality of care without lining numerous corporate pockets along the way with your hard-earned cash, then this book will open your eyes to what is possible.
Click here to check out The Healing Of America, and learn how you could get the same, for less!
Share This Post
-
The 3 Phases Of Fat Loss (& How To Do It Right!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cori Lefkowith, of “Redefining Strength” and “Strength At Any Age” fame, has advice:
As easy as 1, 2, 3?
Any kind of fat loss plan will not work unless it takes into account that the body can and will adapt to a caloric deficit, meaning that constantly running a deficit will only ever yield short term results, followed by regaining weight (and feeling hungry the whole time). So, instead, if fat loss is your goal, you might want to consider doing it in these stages:
1. Lifestyle adjustments (main phase)
Focus on sustainable, gradual improvements in diet and workouts.
- Key strategies:
- Start with small, manageable changes, for example focusing on making your protein intake around 30–35% of your total calories.
- Track your current habits to identify realistic adjustments.
- Balance strength training and cardio, as maintaining your muscle is (and will remain) important.
- Signs of Progress:
- Slow changes in the numbers on the scale (up to 1 lb/week).
- Inches being lost (but probably not many), improved energy levels, and stable performance in workouts.
Caution: avoid feelings of extreme hunger or restriction. This is not supposed to be arduous.
2. Mini cut (short-term intensive)
Used for quick fat loss or breaking plateaus; lasts 7–14 days.
- Key strategies:
- Larger calorie deficit (e.g: 500 calories).
- High protein intake (40–50% of your total calories).
- Focus on strength training and reduce cardio, to avoid muscle loss.
- Signs of Progress:
- Rapid scale changes (up to 5 lbs/week).
- Reduced bloating, potential energy dips, and cravings.
- Temporary performance stagnation in workouts. Don’t worry about this; it’s expected and fine.
Caution: do not exceed 21 days, to avoid the metabolic adaptation that we talked about.
3. Diet break (rest & reset)
A maintenance period to recharge mentally and physically, typically lasting 7–21 days.
- Key strategies:
- Gradually increase calories (200–500) to maintenance level.
- Focus on performance goals and reintroducing foods you enjoy.
- Combine strength training with steady-state cardio.
- Signs of Progress:
- Increased energy, improved workout performance, and feeling fuller.
- Scale may fluctuate initially but stabilize or decrease by the end.
- Inches will be lost as muscle is built and fat is burned.
The purpose of this third stage is to prevent metabolic adaptation, regain motivation, and (importantly!) test maintenance.
For more on these and how best to implement them, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
- Key strategies:
Related Posts
-
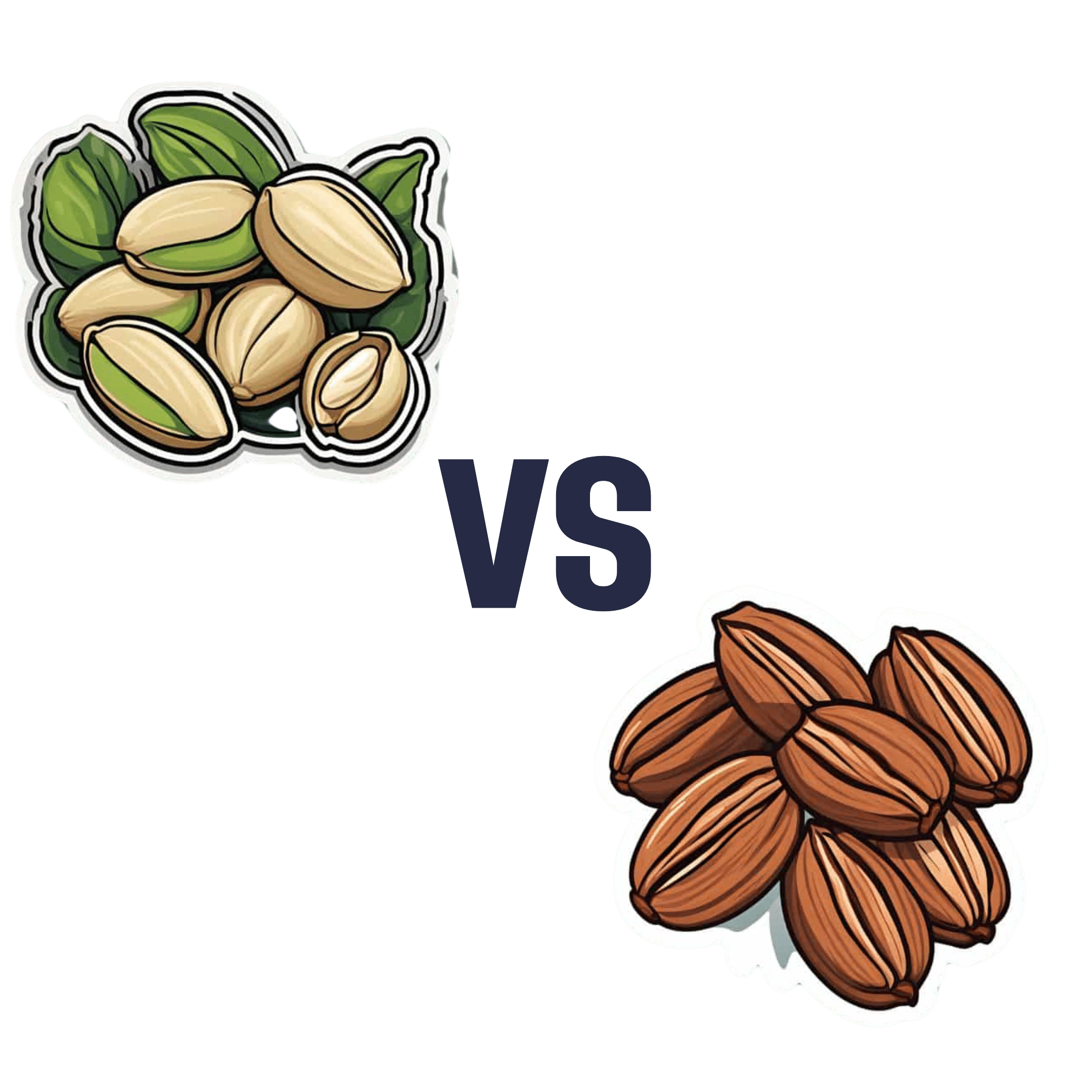
Pistachios vs Pecans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pistachios to pecans, we picked the pistachios.
Why?
Firstly, the macronutrients: pistachios have twice as much protein and fiber. Pecans have more fat, though in both of these nuts the fats are healthy.
The category of vitamins is an easy win for pistachios, with a lot more of vitamins A, B1, B2, B3, B6, B9, C, and E. Especially the 8x vitamin A, 7x vitamin B6, 4x vitamin C, and 2x vitamin E, and as the percentages are good too, these aren’t small differences. Pecans, meanwhile, boast only a little more vitamin B5 (pantothenic acid, the one whose name means “it’s everywhere”, because that’s how easy it is to get it).
In terms of minerals, pistachios have more calcium, iron, phosphorus, potassium, and selenium, while pecans have more manganese and zinc. So, a fair win for pistachios on this one.
Adding up the three different kinds of win for pistachios means that *drumroll* pistachios win overall, and it’s not close.
As ever, do enjoy both though, because diversity is healthy!
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What is mitochondrial donation? And how might it help people have a healthy baby one day?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mitochondria are tiny structures in cells that convert the food we eat into the energy our cells need to function.
Mitochondrial disease (or mito for short) is a group of conditions that affect this ability to generate the energy organs require to work properly. There are many different forms of mito and depending on the form, it can disrupt one or more organs and can cause organ failure.
There is no cure for mito. But an IVF procedure called mitochondrial donation now offers hope to families affected by some forms of mito that they can have genetically related children free from mito.
After a law to allow mitochondrial donation in Australia was passed in 2022, scientists are now preparing for a clinical trial to see if mitochondrial donation is safe and works.
Jonathan Borba/Pexels What is mitochondrial disease?
There are two types of mitochondrial disease.
One is caused by faulty genes in the nuclear DNA, the DNA we inherit from both our parents and which makes us who we are.
The other is caused by faulty genes in the mitochondria’s own DNA. Mito caused by faulty mitochondrial DNA is passed down through the mother. But the risk of disease is unpredictable, so a mother who is only mildly affected can have a child who develops serious disease symptoms.
Mitochondrial disease is the most common inherited metabolic condition affecting one in 5,000 people.
Some people have mild symptoms that progress slowly, while others have severe symptoms that progress rapidly. Mito can affect any organ, but organs that need a lot of energy such as brain, muscle and heart are more often affected than other organs.
Mito that manifests in childhood often involves multiple organs, progresses rapidly, and has poor outcomes. Of all babies born each year in Australia, around 60 will develop life-threatening mitochondrial disease.
What is mitochondrial donation?
Mitochondrial donation is an experimental IVF-based technique that offers people who carry faulty mitochondrial DNA the potential to have genetically related children without passing on the faulty DNA.
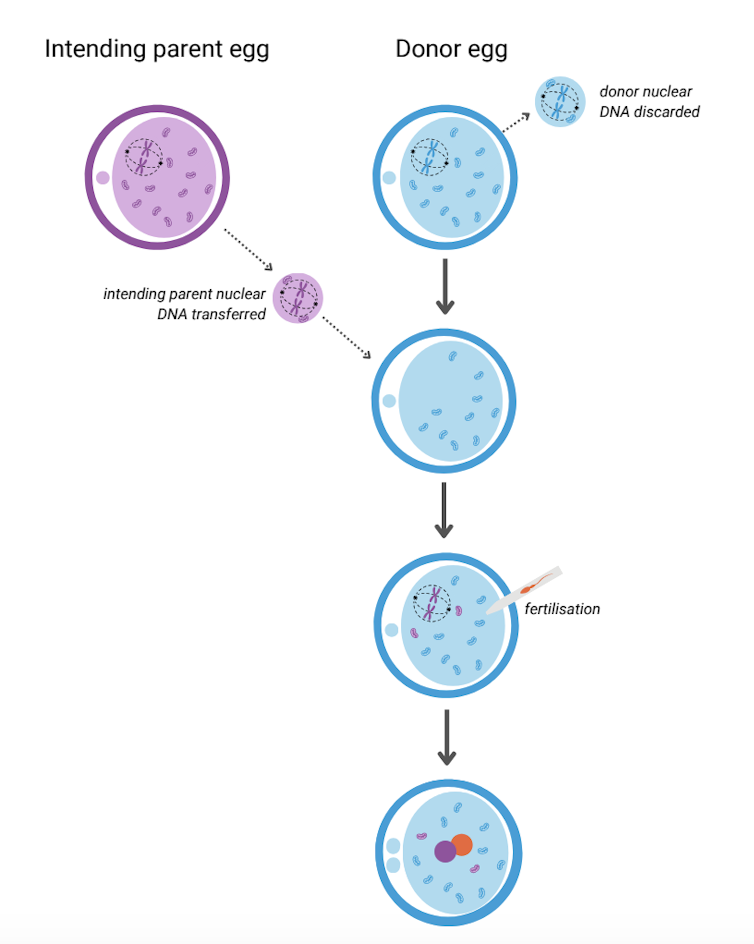
It involves removing the nuclear DNA from the egg of someone who carries faulty mitochondrial DNA and inserting it into a healthy egg donated by someone not affected by mito, which has had its nuclear DNA removed.
The donor egg (in blue) has had its nuclear DNA removed. Author provided The resulting egg has the nuclear DNA of the intending parent and functioning mitochondria from the donor. Sperm is then added and this allows the transmission of both intending parents’ nuclear DNA to the child.
A child born after mitochondrial donation will have genetic material from the three parties involved: nuclear DNA from the intending parents and mitochondrial DNA from the egg donor. As a result the child will likely have a reduced risk of mito, or no risk at all.
The procedure removes the faulty DNA to reduce the chance of it passing on to the baby. Josh Willink/Pexels This highly technical procedure requires specially trained scientists and sophisticated equipment. It also requires both the person with mito and the egg donor to have hormone injections to stimulate the ovaries to produce multiple eggs. The eggs are then retrieved in an ultrasound-guided surgical procedure.
Mitochondrial donation has been pioneered in the United Kingdom where a handful of babies have been born as a result. To date there have been no reports about whether they are free of mito.
Maeve’s Law
After three years of public consultation The Mitochondrial Donation Law Reform (Maeve’s Law) Bill 2021 was passed in the Australian Senate in 2022, making mitochondrial donation legal in a research and clinical trial setting.
Maeve’s law stipulates strict conditions including that clinics need a special licence to perform mitochondrial donation.
To make sure mitochondrial donation works and is safe before it’s introduced into Australian clinical practice, the law also specifies that initial licences will be issued for pre-clinical and clinical trial research and training.
We’re expecting one such licence to be issued for the mitoHOPE (Healthy Outcomes Pilot and Evaluation) program, which we are part of, to perfect the technique and conduct a clinical trial to make sure mitochondrial donation is safe and effective.
Before starting the trial, a preclinical research and training program will ensure embryologists are trained in “real-life” clinical conditions and existing mitochondrial donation techniques are refined and improved. To do this, many human eggs are needed.
The need for donor eggs
One of the challenges with mitochondrial donation is sourcing eggs. For the preclinical research and training program, frozen eggs can be used, but for the clinical trial “fresh” eggs will be needed.
One possible source of frozen eggs is from people who have stored eggs they don’t intend to use.
A recent study looked at data on the outcomes of eggs stored at a Melbourne clinic from 2012 to 2021. Over the ten-year period, 1,132 eggs from 128 patients were discarded. No eggs were donated to research because the clinics where the eggs were stored did not conduct research requiring donor eggs.
However, research shows that among people with stored eggs, the number one choice for what to do with eggs they don’t need is to donate them to research.
This offers hope that, given the opportunity, those who have eggs stored that they don’t intend to use might be willing to donate them to mitochondrial donation preclinical research.
As for the “fresh” eggs needed in the future clinical trial, this will require individuals to volunteer to have their ovaries stimulated and eggs retrieved to give those people impacted by mito a chance to have a healthy baby. Egg donors may be people who are friends or relatives of those who enter the trial, or it might be people who don’t know someone affected by mito but would like to help them conceive.
At this stage, the aim is to begin enrolling participants in the clinical trial in the next 12 to 18 months. However this may change depending on when the required licences and ethics approvals are granted.
Karin Hammarberg, Senior Research Fellow, Global and Women’s Health, School of Public Health & Preventive Medicine, Monash University; Catherine Mills, Professor of Bioethics, Monash University; Mary Herbert, Professor, Anatomy & Developmental Biology, Monash University, and Molly Johnston, Research fellow, Monash Bioethics Centre, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What’s Your Plant Diversity Score?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We speak often about the importance of dietary diversity, and of that, especially diversity of plants in one’s diet, but we’ve never really focused on it as a main feature, so that’s what we’re going to do today.
Specifically, you may have heard the advice to “eat 30 different kinds of plants per week”. But where does that come from, and is it just a number out of a hat?
The magic number?
It is not, in fact, a number out of a hat. It’s from a big (n=11,336) study into what things affect the gut microbiome for better or for worse. It was an observational population study, championing “citizen science” in which volunteers tracked various things and collected and sent in various samples for analysis.
The most significant finding of this study was that those who consumed more than 30 different kinds of plants per week, had a much better gut microbiome than those who consumed fewer than 10 different kinds of plants per week (there is a bell curve at play, and it gets steep around 10 and 30):
American Gut: an Open Platform for Citizen Science Microbiome Research
Why do I care about having a good gut microbiome?
Gut health affects almost every other kind of health; it’s been called “the second brain” for the various neurotransmitters and other hormones it directly makes or indirectly regulates (which in turn affect every part of your body), and of course there is the vagus nerve connecting it directly to the brain, impacting everything from food cravings to mood swings to sleep habits.
See also:
Any other benefits?
Yes there are! Let’s not forget: as we see often in our “This or That” section, different foods can be strong or weak in different areas of nutrition, so unless we want to whip out a calculator and database every time we make food choices, a good way to cover everything is to simply eat a diverse diet.
And that goes not just for vitamins and minerals (which would be true of animal products also), but in the case of plants, a wide range of health-giving phytochemicals too:
Measuring Dietary Botanical Diversity as a Proxy for Phytochemical Exposure
Ok, I’m sold, but 30 is a lot!
It is, but you don’t have to do all 30 in your first week of focusing on this, if you’re not already accustomed to such diversity. You can add in one or two new ones each time you go shopping, and build it up.
As for “what counts”: we’re counting unprocessed or minimally-processed plants. So for example, an apple is an apple, as are dried apple slices, as is apple sauce. Any or all of those would count as 1 plant type.
Note also that we’re counting types, not totals. If you’re having apple slices with apple sauce, for some reason? That still only counts as 1.
However, while apple sauce still counts as apples (minimally processed), you cannot eat a cake and say “that’s 2 because there was wheat and sugar cane somewhere in its dim and distant history”.
Nor is your morning espresso a fruit (by virtue of coffee beans being the fruit of the plant, botanically speaking). However, it would count as 1 plant type if you eat actual coffee beans—this writer has been known to snack on such; they’re only healthy in very small portions though, because their saturated fat content is a little high.
You, however, count grains in general, as well as nuts and seeds, not just fruits and vegetables. As for herbs and spices, they count for ¼ each, except for salt, which might get lumped in with spices but is of course not a plant.
How to do it
There’s a reason we’re doing this in our Saturday Life Hacks edition. Here are some tips for getting in far more plants than you might think, a lot more easily than you might think:
- Buy things ready-mixed. This means buying the frozen mixed veg, the frozen mixed chopped fruit, the mixed nuts, the mixed salad greens etc. This way, when you’re reaching for one pack of something, you’re getting 3–5 different plants instead of one.
- Buy things individually, and mix them for storage. This is a more customized version of the above, but in the case of things that keep for at least a while, it can make lazy options a lot more plentiful. Suddenly, instead of rice with your salad you’re having sorghum, millet, buckwheat, and quinoa. This trick also works great for dried berries that can just be tipped into one’s morning oatmeal. Or, you know, millet, oats, rye, and barley. Suddenly, instead of 1 or 2 plants for breakfast you have maybe 7 or 8.
- Keep a well-stocked pantry of shelf-stable items. This is good practice anyway, in case of another supply-lines shutdown like at the start of the COVID-19 pandemic. But for plant diversity, it means that if you’re making enchiladas, then instead using kidney beans because that’s what’s in the cupboard, you can raid your pantry for kidney beans, black beans, pinto beans, fava beans, etc etc. Yes, all of them; that’s a list, not a menu.
- Shop in the discount section of the supermarket. You don’t have shop exclusively there, but swing by that area, see what plants are available for next to nothing, and buy at least one of each. Figure out what to do with it later, but the point here is that it’s a good way to get suggestions of plants that you weren’t actively looking for—and novelty is invariably a step into diversity.
- Shop in a different store. You won’t be able to beeline the products you want on autopilot, so you’ll see other things on the way. Also, they may have things your usual store doesn’t.
- Shop in person, not online—at least as often as is practical. This is because when shopping for groceries online, the store will tend to prioritize showing you items you’ve bought before, or similar items to those (i.e. actually the same item, just a different brand). Not good for trying new things!
- Consider a meal kit delivery service. Because unlike online grocery shopping, this kind of delivery service will (usually) provide you with things you wouldn’t normally buy. Our sometimes-sponsor Purple Carrot is a fine option for this, but there are plenty of others too.
- Try new recipes, especially if they have plants you don’t normally use. Make a note of the recipe, and go out of your way to get the ingredients; if it seems like a chore, reframe it as a little adventure instead. Honestly, it’s things like this that keep us young in more ways than just what polyphenols can do!
- Hide the plants. Whether or not you like them; hide them just because it works in culinary terms. By this we mean; blend beans into that meaty sauce; thicken the soup with red lentils, blend cauliflower into the gravy. And so on.
One more “magic 30”, while we’re at it…
30g fiber per day makes a big (positive) difference to many aspects of health. Obviously, plants are where that comes from, so there’s a big degree of overlap here, but most of the tips we gave are different, so for double the effectiveness, check out:
Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: