Falling vaccination rates put children at risk of preventable diseases. Governments need a new strategy to boost uptake
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Child vaccination is one of the most cost-effective health interventions. It accounts for 40% of the global reduction in infant deaths since 1974 and has led to big health gains in Australia over the past two decades.
Australia has been a vaccination success story. Ten years after we begun mass vaccination against polio in 1956, it was virtually eliminated. Our child vaccination rates have been among the best in the world.
But after peaking in 2020, child vaccination in Australia is falling. Governments need to implement a comprehensive strategy to boost vaccine uptake, or risk exposing more children to potentially preventable infectious diseases.

Child vaccination has been a triumph
Thirty years ago, Australia’s childhood vaccination rates were dismal. Then, in 1997, governments introduced the National Immunisation Program to vaccinate children against diseases such as diphtheria, tetanus, and measles.
Measures to increase coverage included financial incentives for parents and doctors, a public awareness campaign, and collecting and sharing local data to encourage the least-vaccinated regions to catch up with the rest of the country.
What followed was a public health triumph. In 1995, only 52% of one-year-olds were fully immunised. By 2020, Australia had reached 95% coverage for one-year-olds and five-year-olds. At this level, it’s difficult even for highly infectious diseases, such as measles, to spread in the community, protecting both the vaccinated and unvaccinated.

Gaps between regions and communities closed too. In 1999, the Northern Territory’s vaccination rate for one-year-olds was the lowest in the country, lagging the national average by six percentage points. By 2020, that gap had virtually disappeared.
The difference between vaccination rates for First Nations children and other children also narrowed considerably.
It made children healthier. The years of healthy life lost due to vaccine-preventable diseases for children aged four and younger fell by nearly 40% in the decade to 2015.
Some diseases have even been eliminated in Australia.
Our success is slipping away
But that success is at risk. Since 2020, the share of children who are fully vaccinated has fallen every year. For every child vaccine on the National Immunisation Schedule, protection was lower in 2024 than in 2020.
Gaps between parts of Australia are opening back up. Vaccination rates in the highest-coverage parts of Australia are largely stable, but they are falling quickly in areas with lower vaccination.
In 2018, there were only ten communities where more than 10% of one-year-old children were not fully vaccinated. Last year, that number ballooned to 50 communities. That leaves more areas vulnerable to disease and outbreaks.
While Noosa, the Gold Coast Hinterland and Richmond Valley (near Byron Bay) have persistently had some of the country’s lowest vaccination rates, areas such as Manjimup in Western Australia and Tasmania’s South East Coast have recorded big declines since 2018.
Missing out on vaccination isn’t just a problem for children.
One preprint study (which is yet to be peer-reviewed) suggests vaccination during pregnancy may also be declining.
Far too many older Australians are missing out on recommended vaccinations for flu, COVID, pneumococcal and shingles. Vaccination rates in aged care homes for flu and COVID are worryingly low.
What’s going wrong?
Australia isn’t alone. Since the pandemic, child vaccination rates have fallen in many high-income countries, including New Zealand, the United Kingdom and the United States.
Globally, in 2023, measles cases rose by 20%, and just this year, a measles outbreak in rural Texas has put at least 13 children in hospital.
Alarmingly, some regions in Australia have lower measles vaccination than that Texas county.
The timing of trends here and overseas suggests things shifted, or at least accelerated, during the pandemic. Vaccine hesitancy, fuelled by misinformation about COVID vaccines, is a growing threat.
This year, vaccine sceptic Robert F. Kennedy Jr was appointed to run the US health system, and Louisiana’s top health official has reportedly cancelled the promotion of mass vaccination.
In Australia, a recent survey found 6% of parents didn’t think vaccines were safe, and 5% believed they don’t work.
Those concerns are far more common among parents with children who are partially vaccinated or unvaccinated. Among the 2% of parents whose children are unvaccinated, almost half believe vaccines are not safe for their child, and four in ten believe vaccines didn’t work.
Other consequences of the pandemic were a spike in the cost of living, and a health system struggling to meet demand. More than one in ten parents said cost and difficulty getting an appointment were barriers to vaccinating their children.
There’s no single cause of sliding vaccination rates, so there’s no one solution. The best way to reverse these worrying trends is to work on all the key barriers at once – from a lack of awareness, to inconvenience, to lack of trust.
What governments should do
Governments should step up public health campaigns that counter misinformation, boost awareness of immunisation and its benefits, and communicate effectively to low-vaccination groups. The new Australian Centre for Disease Control should lead the charge.
Primary health networks, the regional bodies responsible for improving primary care, should share data on vaccination rates with GPs and pharmacies. These networks should also help make services more accessible to communities who are missing out, such as migrant groups and disadvantaged families.
State and local governments should do the same, sharing data and providing support to make maternal child health services and school-based vaccination programs accessible for all families.

Governments should also be more ambitious about tackling the growing vaccine divides between different parts of the country. The relevant performance measure in the national vaccination agreement is weak. States must only increase five-year-old vaccination rates in four of the ten areas where it is lowest. That only covers a small fraction of low-vaccination areas, and only the final stage of child vaccination.
Australia needs to set tougher goals, and back them with funding.
Governments should fund tailored interventions in areas with the lowest rates of vaccination. Proven initiatives include training trusted community members as “community champions” to promote vaccinations, and pop-up clinics or home visits for free vaccinations.
At this time of year, childcare centres and schools are back in full swing. But every year, each new intake has less protection than the previous cohort. Governments are developing a new national vaccination strategy and must seize the opportunity to turn that trend around. If it commits to a bold national plan, Australia can get back to setting records for child vaccination.
Peter Breadon, Program Director, Health and Aged Care, Grattan Institute and Wendy Hu, Associate, Health Program, Grattan Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
As Nuns Disappear, Many Catholic Hospitals Look More Like Megacorporations
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ST. LOUIS — Inside the more than 600 Catholic hospitals across the country, not a single nun can be found occupying a chief executive suite, according to the Catholic Health Association.
Nuns founded and led those hospitals in a mission to treat sick and poor people, but some were also shrewd business leaders. Sister Irene Kraus, a former chief executive of Daughters of Charity National Health System, was famous for coining the phrase “no margin, no mission.” It means hospitals must succeed — generating enough revenue to exceed expenses — to fulfill their original mission.
The Catholic Church still governs the care that can be delivered to millions in those hospitals each year, using religious directives to ban abortions and limit contraceptives, in vitro fertilization, and medical aid in dying.
But over time, that focus on margins led the hospitals to transform into behemoths that operate for-profit subsidiaries and pay their executives millions, according to hospital tax filings. These institutions, some of which are for-profit companies, now look more like other megacorporations than like the charities for the destitute of yesteryear.
The absence of nuns in the top roles raises the question, said M. Therese Lysaught, a Catholic moral theologist and professor at Loyola University Chicago: “What does it mean to be a Catholic hospital when the enterprise has been so deeply commodified?”
The St. Louis area serves as the de facto capital of Catholic hospital systems. Three of the largest are headquartered here, along with the Catholic hospital lobbying arm. Catholicism is deeply rooted in the region’s culture. During Pope John Paul II’s only U.S. stop in 1999, he led Mass downtown in a packed stadium of more than 100,000 people.
For a quarter century, Sister Mary Jean Ryan led SSM Health, one of those giant systems centered on St. Louis. Now retired, the 86-year-old said she was one of the last nuns in the nation to lead a Catholic hospital system.
Ryan grew up Catholic in Wisconsin and joined a convent while in nursing school in the 1960s, surprising her family. She admired the nuns she worked alongside and felt they were living out a higher purpose.
“They were very impressive,” she said. “Not that I necessarily liked all of them.”
Indeed, the nuns running hospitals defied the simplistic image often ascribed to them, wrote John Fialka in his book “Sisters: Catholic Nuns and the Making of America.”
“Their contributions to American culture are not small,” he wrote. “Ambitious women who had the skills and the stamina to build and run large institutions found the convent to be the first and, for a long time, the only outlet for their talents.”
This was certainly true for Ryan, who climbed the ranks, working her way from nurse to chief executive of SSM Health, which today has hospitals in Illinois, Missouri, Oklahoma, and Wisconsin.
The system was founded more than a century ago when five German nuns arrived in St. Louis with $5. Smallpox swept through the city and the Sisters of St. Mary walked the streets offering free care to the sick.
Their early foray grew into one of the largest Catholic health systems in the country, with annual revenue exceeding $10 billion, according to its 2023 audited financial report. SSM Health treats patients in 23 hospitals and co-owns a for-profit pharmacy benefit manager, Navitus, that coordinates prescriptions for 14 million people.
But Ryan, like many nuns in leadership roles in recent decades, found herself confronted with an existential crisis. As fewer women became nuns, she had to ensure the system’s future without them.
When Ron Levy, who is Jewish, started at SSM as an administrator, he declined to lead a prayer in a meeting, Ryan recounted in her book, “On Becoming Exceptional.”
“Ron, I’m not asking you to be Catholic,” she recalled telling him. “And I know you’ve only been here two weeks. So, if you’d like to make it three, I suggest you be prepared to pray the next time you’re asked.”
Levy went on to serve SSM for more than 30 years — praying from then on, Ryan wrote.
In Catholic hospitals, meetings are still likely to start with a prayer. Crucifixes often adorn buildings and patient rooms. Mission statements on the walls of SSM facilities remind patients: “We reveal the healing presence of God.”
Above all else, the Catholic faith calls on its hospitals to treat everyone regardless of race, religion, or ability to pay, said Diarmuid Rooney, a vice president of the Catholic Health Association. No nuns run the trade group’s member hospitals, according to the lobbying group. But the mission that compelled the nuns is “what compels us now,” Rooney said. “It’s not just words on a wall.”
The Catholic Health Association urges its hospitals to evaluate themselves every three years on whether they’re living up to Catholic teachings. It created a tool that weighs seven criteria, including how a hospital acts as an extension of the church and cares for poor and marginalized patients.
“We’re not relying on hearsay that the Catholic identity is alive and well in our facilities and hospitals,” Rooney said. “We can actually see on a scale where they are at.”
The association does not share the results with the public.
At SSM Health, “our Catholic identity is deeply and structurally ingrained” even with no nun at the helm, spokesperson Patrick Kampert said. The system reports to two boards. One functions as a typical business board of directors while the other ensures the system abides by the rules of the Catholic Church. The church requires the majority of that nine-member board to be Catholic. Three nuns currently serve on it; one is the chair.
Separately, SSM also is required to file an annual report with the Vatican detailing the ways, Kampert said, “we deepen our Catholic identity and further the healing ministry of Jesus.” SSM declined to provide copies of those reports.
From a business perspective, though, it’s hard to distinguish a Catholic hospital system like SSM from a secular one, said Ruth Hollenbeck, a former Anthem insurance executive who retired in 2018 after negotiating Missouri hospital contracts. In the contracts, she said, the difference amounted to a single paragraph stating that Catholic hospitals wouldn’t do anything contrary to the church’s directives.
To retain tax-exempt status under Internal Revenue Service rules, all nonprofit hospitals must provide a “benefit” to their communities such as free or reduced-price care for patients with low incomes. But the IRS provides a broad definition of what constitutes a community benefit, which gives hospitals wide latitude to justify not needing to pay taxes.
On average, the nation’s nonprofit hospitals reported that 15.5% of their total annual expenses were for community benefits in 2020, the latest figure available from the American Hospital Association.
SSM Health, including all of its subsidiaries, spent proportionately far less than the association’s average for individual hospitals, allocating roughly the same share of its annual expenses to community efforts over three years: 5.1% in 2020, 4.5% in 2021, and 4.9% in 2022, according to a KFF Health News analysis of its most recent publicly available IRS filings and audited financial statements.
A separate analysis from the Lown Institute think tank placed five Catholic systems — including the St. Louis region’s Ascension — on its list of the 10 health systems with the largest “fair share” deficits, which means receiving more in tax breaks than what they spent on the community. And Lown said three St. Louis-area Catholic health systems — Ascension, SSM Health, and Mercy — had fair share deficits of $614 million, $235 million, and $92 million, respectively, in the 2021 fiscal year.
Ascension, Mercy, and SSM disputed Lown’s methodology, arguing it doesn’t take into account the gap between the payments they receive for Medicaid patients and the cost of delivering their care. The IRS filings do.
But, Kampert said, many of the benefits SSM provides aren’t reflected in its IRS filings either. The forms reflect “very simplistic calculations” and do not accurately represent the health system’s true impact on the community, he said.
Today, SSM Health is led by longtime business executive Laura Kaiser. Her compensation in 2022 totaled $8.4 million, including deferred payments, according to its IRS filing. Kampert defended the amount as necessary “to retain and attract the most qualified” candidate.
By contrast, SSM never paid Ryan a salary, giving instead an annual contribution to her convent of less than $2 million a year, according to some tax filings from her long tenure. “I didn’t join the convent to earn money,” Ryan said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
NADᐩ Against Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Nicotinamide adenine dinucleotide, or “NAD” to its friends, is a coenzyme produced in the human body (amongst other places), and it is critical for cellular energy metabolism, but there’s more to it than that.
Today we’ll be looking mostly at NAD+, of which the + indicates the positive formal charge of one of its nitrogen atoms. We won’t get too much into the chemistry of this, but we will mention that it’s a cofactor with NADH—the former accepting electrons and the latter donating electrons.
Both NAD+ and NADH are critical to good health, but we’re going to focus on NAD+ for the simple reason that it gets depleted with aging.
Note: it gets depleted with aging.
Chronological age is not so important here, but there is a direct relationship between biological aging and NAD+ depletion.
For example, healthy centenarians tend not to have depleted NAD+ levels. Further, its depletion (in those in whom it is depleted) is then a causal factor for many age-related diseases:
❝Remarkably, ageing is accompanied by a gradual decline in tissue and cellular NAD+ levels in multiple model organisms, including rodents and humans.
This decline in NAD+ levels is linked causally to numerous ageing-associated diseases, including cognitive decline, cancer, metabolic disease, sarcopenia and frailty.
Many of these ageing-associated diseases can be slowed down and even reversed by restoring NAD+ levels.❞
~ Dr. Rosalba Perrone et al.
Read in full: NAD+ metabolism and its roles in cellular processes during ageing
As for restoring those NADᐩ levels, that does help in interventional trials, whether by supplementing directly, or with NAD precursors*:
❝NAD+ levels steadily decline with age, resulting in altered metabolism and increased disease susceptibility.
Restoration of NAD+ levels in old or diseased animals can promote health and extend lifespan, prompting a search for safe and efficacious NAD-boosting molecules that hold the promise of increasing the body’s resilience, not just to one disease, but to many, thereby extending healthy human lifespan.❞
~ Dr. David Sinclair et al.
Read more: Therapeutic Potential of NAD-Boosting Molecules: The In Vivo Evidence
*There are actually also other NAD-boosting molecules besides NAD itself and its precursors. For example, the liver will not produce NADᐩ unless it has aminocarboxymuconate-semialdehyde decarboxylase (or “ACMSD”, to its friends), which limits the production of NADᐩ. Why, you ask? The theory is that it is a kind of evolutionary conservativism, much like not lighting a fire without the ability to put it out. In any case, taking ACMSD-blockers will thus result in an increased endogenous production of NADᐩ.
You can read about this here:
De novo NAD+ synthesis enhances mitochondrial function and improves health
Nor is taking supplements or drugs the only way to get more of it; there’s an enzyme nicotinamide phosphoribosyltransferase (“NAMPT”, to its friends) involved in the synthesis of NADᐩ, and exercise boosts levels by 127% (i.e., it more than doubles the levels), based on a modest three-week exercise bike regimen:
Skeletal muscle NAMPT is induced by exercise in humans
And to underline that point, another study found that resistance training (so, a different kind of exercise from that of the previous study) boosts levels of NADᐩ itself by the same 127%:
One way to get more out of NADᐩ
We’ll get straight to the point: it works very well paired with a senolytic agent, i.e. something that kills aging cells so that they get recycled sooner:
NAD+, Senolytics, or Pyruvate for Healthy Aging?
To read more about senolytics, check out:
Fisetin: The Anti-Aging Assassin
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Share This Post
-
Take These To Lower Cholesterol! (Statin Alternatives)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Ada Ozoh, a diabetes specialist, took an interest in this upon noting the many-headed beast that is metabolic syndrome means that neither diabetes nor cardiovascular disease exist in a vacuum, and there are some things that can help a lot against both. Here she shares some of her top recommendations:
Statin-free options
Dr. Ozoh recommends:
- Bergamot: lowers LDL (“bad” cholesterol) by about 30% and slightly increases HDL (“good” cholesterol), at 500–1000mg/day, seeing results in 1–6 months
- Berberine: prevents fat absorption and helps burn stored fat, as well as reducing blood sugar levels and blood pressure, at 1,500mg/day
- Silymarin: protects the liver, and lowers cholesterol in type 2 diabetes, at 280–420mg/day
- Phytosterols: lower cholesterol by about 10%; found naturally in many plants, but it takes supplementation to read the needed (for this purpose) dosage of 2g/day
- Red yeast rice: this is white rice fermented with yeast, and it lowers LDL cholesterol by about 25%, seeing results in around 3 months
For more information on all of the above (including more details on the biochemistry, as well as potential issues to be aware of), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Statins: His & Hers? Very Different For Men & Women
- Berberine For Metabolic Health
- Milk Thistle For The Brain, Bones, & More ← this is about silymarin, which is extracted from Silybum marianum, the milk thistle plant
Take care!
Share This Post
Related Posts
-
Which Comes First, Cardio or Weights? – by Alex Hutchinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a book of questions and answers, myths and busts, and in short, all things exercise.
It’s laid out as many micro-chapters with questions as headers. The explanations are clear and easy to understand, with several citations (of studies and other academic papers) per question.
While it’s quite comprehensive (weighing in at a hefty 300+ pages), it’s not the kind of book where one could just look up any given piece of information that one wants.
Its strength, rather, lies in pre-emptively arming the reader with knowledge, and correcting many commonly-believed myths. It can be read cover-to-cover, or just dipped into per what interests you (the table of contents lists all questions, so it’s easy to flip through).
Bottom line: if you’ve found the world of exercise a little confusing and would like it demystifying, this book will result in a lot of “Oooooh” moments.
Click here to check out Which Comes First, Cardio or Weights?, and know your stuff!
PS: the short answer to the titular question is “mix it up and keep it varied”
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Hardwiring Happiness – by Dr. Rick Hanson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Publishers are very excitable about “the new science of…”, and it’s almost never actually a new science of. But what about in this case?
No, it isn’t. It’s the very well established science of! And that’s a good thing, because it means this book is able to draw on quite a lot of research and established understanding of how neuroplasticity works, to leverage that and provide useful guidance.
A particular strength of this book is that while it polarizes the idea that some people have “happy amygdalae” and some people have “sad amygdalae”, it acknowledges that it’s not just a fated disposition and is rather the result of the lives people have led… And then provides advice on upgrading from sad to happy, based on the assumption that the reader is quite possibly coming from a non-ideal starting point.
The bookdoes an excellent job of straddling neuroscience and psychology, which sounds like not much of a straddle (the two are surely very connected, after all, right?) but this does mean that we’re hearing about the chemical structure of DNA inside the nuclei of the neurons of the insula, not long after reading an extended gardening metaphor about growth, choices, and vulnerabilities.
Bottom line: if you’d like a guide to changing your brain for the better (happier) that’s not just “ask yourself: what if it goes well?” and similar CBTisms, then this is a fine book for you.
Click here to check out Hardwiring Happiness, and indeed hardwire happiness!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Oral vaccines could provide relief for people who suffer regular UTIs. Here’s how they work
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a recent TikTok video, Australian media personality Abbie Chatfield shared she was starting a vaccine to protect against urinary tract infections (UTIs).
Huge news for the UTI girlies. I am starting a UTI vaccine tonight for the first time.
Chatfield suffers from recurrent UTIs and has turned to the Uromune vaccine, an emerging option for those seeking relief beyond antibiotics.
But Uromune is not a traditional vaccine injected to your arm. So what is it and how does it work?
9nong/Shutterstock First, what are UTIs?
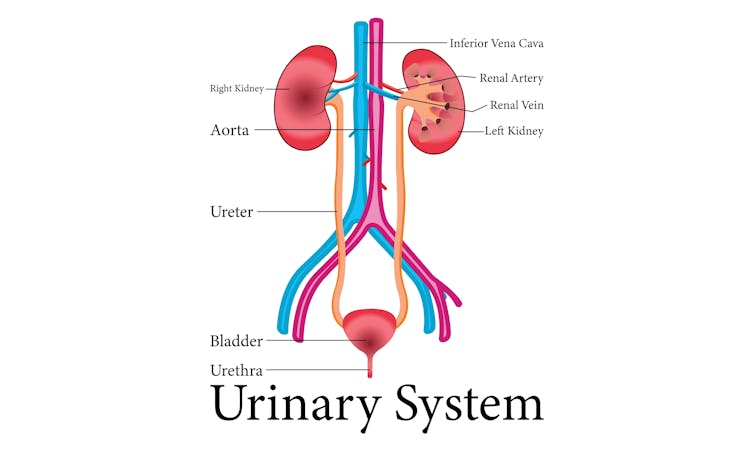
UTIs are caused by bacteria entering the urinary system. This system includes the kidneys, bladder, ureters (thin tubes connecting the kidneys to the bladder), and the urethra (the tube through which urine leaves the body).
The most common culprit is Escherichia coli (E. coli), a type of bacteria normally found in the intestines.
While most types of E. coli are harmless in the gut, it can cause infection if it enters the urinary tract. UTIs are particularly prevalent in women due to their shorter urethras, which make it easier for bacteria to reach the bladder.
Roughly 50% of women will experience at least one UTI in their lifetime, and up to half of those will have a recurrence within six months.
UTIs are caused by bacteria enterning the urinary system. oxo7051/Shutterstock The symptoms of a UTI typically include a burning sensation when you wee, frequent urges to go even when the bladder is empty, cloudy or strong-smelling urine, and pain or discomfort in the lower abdomen or back. If left untreated, a UTI can escalate into a kidney infection, which can require more intensive treatment.
While antibiotics are the go-to treatment for UTIs, the rise of antibiotic resistance and the fact many people experience frequent reinfections has sparked more interest in preventive options, including vaccines.
What is Uromune?
Uromune is a bit different to traditional vaccines that are injected into the muscle. It’s a sublingual spray, which means you spray it under your tongue. Uromune is generally used daily for three months.
It contains inactivated forms of four bacteria that are responsible for most UTIs, including E. coli. By introducing these bacteria in a controlled way, it helps your immune system learn to recognise and fight them off before they cause an infection. It can be classified as an immunotherapy.
A recent study involving 1,104 women found the Uromune vaccine was 91.7% effective at reducing recurrent UTIs after three months, with effectiveness dropping to 57.6% after 12 months.
These results suggest Uromune could provide significant (though time-limited) relief for women dealing with frequent UTIs, however peer-reviewed research remains limited.
Any side effects of Uromune are usually mild and may include dry mouth, slight stomach discomfort, and nausea. These side effects typically go away on their own and very few people stop treatment because of them. In rare cases, some people may experience an allergic reaction.
How can I access it?
In Australia, Uromune has not received full approval from the Therapeutic Goods Administration (TGA), and so it’s not something you can just go and pick up from the pharmacy.
However, Uromune can be accessed via the TGA’s Special Access Scheme or the Authorised Prescriber pathway. This means a GP or specialist can apply for approval to prescribe Uromune for patients with recurrent UTIs. Once the patient has a form from their doctor documenting this approval, they can order the vaccine directly from the manufacturer.
Antibiotics are the go-to treatment for UTIs – but scientists are looking at options to prevent them in the first place. Photoroyalty/Shutterstock Uromune is not covered under the Pharmaceutical Benefits Scheme, meaning patients must cover the full cost out-of-pocket. The cost of a treatment program is around A$320.
Uromune is similarly available through special access programs in places like the United Kingdom and Europe.
Other options in the pipeline
In addition to Uromune, scientists are exploring other promising UTI vaccines.
Uro-Vaxom is an established immunomodulator, a substance that helps regulate or modify the immune system’s response to bacteria. It’s derived from E. coli proteins and has shown success in reducing UTI recurrences in several studies. Uro-Vaxom is typically prescribed as a daily oral capsule taken for 90 days.
FimCH, another vaccine in development, targets something called the adhesin protein that helps E. coli attach to urinary tract cells. FimCH is typically administered through an injection and early clinical trials have shown promising results.
Meanwhile, StroVac, which is already approved in Germany, contains inactivated strains of bacteria such as E. coli and provides protection for up to 12 months, requiring a booster dose after that. This injection works by stimulating the immune system in the bladder, offering temporary protection against recurrent infections.
These vaccines show promise, but challenges like achieving long-term immunity remain. Research is ongoing to improve these options.
No magic bullet, but there’s reason for optimism
While vaccines such as Uromune may not be an accessible or perfect solution for everyone, they offer real hope for people tired of recurring UTIs and endless rounds of antibiotics.
Although the road to long-term relief might still be a bit bumpy, it’s exciting to see innovative treatments like these giving people more options to take control of their health.
Iris Lim, Assistant Professor in Biomedical Science, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: