Evidence doesn’t support spinal cord stimulators for chronic back pain – and they could cause harm
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In an episode of ABC’s Four Corners this week, the use of spinal cord stimulators for chronic back pain was brought into question.
Spinal cord stimulators are devices implanted surgically which deliver electric impulses directly to the spinal cord. They’ve been used to treat people with chronic pain since the 1960s.
Their design has changed significantly over time. Early models required an external generator and invasive surgery to implant them. Current devices are fully implantable, rechargeable and can deliver a variety of electrical signals.
However, despite their long history, rigorous experimental research to test the effectiveness of spinal cord stimulators has only been conducted this century. The findings don’t support their use for treating chronic pain. In fact, data points to a significant risk of harm.
What does the evidence say?
One of the first studies used to support the effectiveness of spinal cord stimulators was published in 2005. This study looked at patients who didn’t get relief from initial spinal surgery and compared implantation of a spinal cord stimulator to a repeat of the spinal surgery.
Although it found spinal cord stimulation was the more effective intervention for chronic back pain, the fact this study compared the device to something that had already failed once is an obvious limitation.
Later studies provided more useful evidence. They compared spinal cord stimulation to non-surgical treatments or placebo devices (for example, deactivated spinal cord stimulators).
A 2023 Cochrane review of the published comparative studies found nearly all studies were restricted to short-term outcomes (weeks). And while some studies appeared to show better pain relief with active spinal cord stimulation, the benefits were small, and the evidence was uncertain.
Only one high-quality study compared spinal cord stimulation to placebo up to six months, and it showed no benefit. The review concluded the data doesn’t support the use of spinal cord stimulation for people with back pain.
What about the harms?
The experimental studies often had small numbers of participants, making any estimate of the harms of spinal cord stimulation difficult. So we need to look to other sources.
A review of adverse events reported to Australia’s Therapeutic Goods Administration found the harms can be serious. Of the 520 events reported between 2012 and 2019, 79% were considered “severe” and 13% were “life threatening”.
We don’t know exactly how many spinal cord stimulators were implanted during this period, however this surgery is done reasonably widely in Australia, particularly in the private and workers compensation sectors. In 2023, health insurance data showed more than 1,300 spinal cord stimulator procedures were carried out around the country.
In the review, around half the reported harms were due to a malfunction of the device itself (for example, fracture of the electrical lead, or the lead moved to the wrong spot in the body). The other half involved declines in people’s health such as unexplained increased pain, infection, and tears in the lining around the spinal cord.
More than 80% of the harms required at least one surgery to correct the problem. The same study reported four out of every ten spinal cord stimulators implanted were being removed.

High costs
The cost here is considerable, with the devices alone costing tens of thousands of dollars. Adding associated hospital and medical costs, the total cost for a single procedure averages more than $A50,000. With many patients undergoing multiple repeat procedures, it’s not unusual for costs to be measured in hundreds of thousands of dollars.
Rebates from Medicare, private health funds and other insurance schemes may go towards this total, along with out-of-pocket contributions.
Insurers are uncertain of the effectiveness of spinal cord stimulators, but because their implantation is listed on the Medicare Benefits Schedule and the devices are approved for reimbursement by the government, insurers are forced to fund their use.
Industry influence
If the evidence suggests no sustained benefit over placebo, the harms are significant and the cost is high, why are spinal cord stimulators being used so commonly in Australia? In New Zealand, for example, the devices are rarely used.
Doctors who implant spinal cord stimulators in Australia are well remunerated and funding arrangements are different in New Zealand. But the main reason behind the lack of use in New Zealand is because pain specialists there are not convinced of their effectiveness.
In Australia and elsewhere, the use of spinal cord stimulators is heavily promoted by the pain specialists who implant them, and the device manufacturers, often in unison. The tactics used by the spinal cord stimulator device industry to protect profits have been compared to tactics used by the tobacco industry.
A 2023 paper describes these tactics which include flooding the scientific literature with industry-funded research, undermining unfavourable independent research, and attacking the credibility of those who raise concerns about the devices.
It’s not all bad news
Many who suffer from chronic pain may feel disillusioned after watching the Four Corners report. But it’s not all bad news. Australia happens to be home to some of the world’s top back pain researchers who are working on safe, effective therapies.
New approaches such as sensorimotor retraining, which includes reassurance and encouragement to increase patients’ activity levels, cognitive functional therapy, which targets unhelpful pain-related thinking and behaviour, and old approaches such as exercise, have recently shown benefits in robust clinical research.
If we were to remove funding for expensive, harmful and ineffective treatments, more funding could be directed towards effective ones.
Ian Harris, Professor of Orthopaedic Surgery, UNSW Sydney; Adrian C Traeger, Research Fellow, Institute for Musculoskeletal Health, University of Sydney, and Caitlin Jones, Postdoctoral Research Associate in Musculoskeletal Health, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
First things first… How much fiber should we be eating?
- The World Health Organization recommends we each get at least 25g of fiber per day:
- A more recent meta-review of studies, involving thousands of people and decades of time, suggests 25–29g is ideal:
- The British Nutritional Foundation gives 30g as the figure:
- The US National Academy of Sciences’ Institute of Medicine recommends 21g–38g per day, depending on age and sex:
- A large study last year gave 30–40g as the figure:
*This one is also a great read to understand more about the “why” of fiber
Meanwhile, the average American gets 16g of fiber per day.
So, how to get more fiber, without piling on too many carbs?
Foods that contain fiber generally contain carbs (there’s a limit to how much celery most people want to eat), so there are two key ideas here:
- Getting a good carb:fiber ratio
- Making substitutions that boost fiber without overdoing (or in some case, even changing) carbs
Meat → Lentils
Well-seasoned lentils can be used to replaced ground beef or similar. A cup of boiled lentils contains 18g of fiber, so you’re already outdoing the average American’s daily total.
Meat → Beans
Black beans are a top-tier option here (15g per cup, cooked weight), but many kinds of beans are great.
Chicken/Fish → Chickpeas
Yes, chicken/fish is already meat, but we’re making a case for chickpeas here. Cooked and seasoned appropriately, they do the job, and pack in 12g of fiber per cup. Also… Hummus!
Bonus: Hummus, eaten with celery sticks.
White pasta/bread → Wholewheat pasta/bread
This is one where “moderation is key”, but if you’re going to eat pasta/bread, then wholewheat is the way to go. Fiber amounts vary, so read labels, but it will always have far more than white.
Processed salty snacks → Almonds and other nuts
Nuts in general are great, but almonds are top-tier for fiber, amongst other things. A 40g handful of almonds contains about 10g of fiber.
Starchy vegetables → Non-starchy vegetables
Potatoes, parsnips, and their friends have their place. But they cannot compete with broccoli, peas, cabbage, and other non-starchy vegetables for fiber content.
Bonus: if you’re going to have starchy vegetables though, leave the skins on!
Fruit juice → Fruit
Fruit juice has had most, if not all, of its fiber removed. Eat an actual juicy fruit, instead. Apples and bananas are great options; berries such as blackberries and raspberries are even better (at around 8g per cup, compared to the 5g or so depending on the size of an apple/banana)
Processed cereals → Oats
5g fiber per cup. Enough said.
Summary
Far from being a Herculean task, getting >30g of fiber per day can be easily accomplished by a lentil ragù with wholewheat pasta.
If your breakfast is overnight oats with fruit and some chopped almonds, you can make it to >20g already by the time you’ve finished your first meal of the day.
Enjoy!
Share This Post
-
9 Reasons To Avoid Mobility Training
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Why might someone not want to do mobility training? Here are some important reasons:
Make an informed choice
Here’s Liv’s hit-list of reasons to skip mobility training:
- Poor Circulation: Avoid mobility training if you don’t want to improve or maintain good blood circulation, which aids muscle recovery and reduces soreness.
- Low Energy Levels: Mobility training increases oxygen flow to the brain and muscles, boosting energy. Skip it if you prefer feeling sluggish!
- Digestive Health: Stretches that rotate the torso aid digestion and relieve bloating. Definitely best to avoid it if you’re uninterested in improving digestive health.
- Joint Health: Mobility work stimulates synovial fluid production, reducing joint friction and promoting longevity. You can skip it if you don’t care about comfortable movement.
- Sleep Quality: Gentle stretching triggers relaxation, aiding restful sleep. Avoid it if you enjoy restless nights!
- Pain Tolerance: Stretching trains the nervous system to handle discomfort better. Skip it if you prefer suffering 🙂
- Headache Reduction: Mobility work relieves tension in the neck and shoulders, reducing the occurrence and severity of headaches. No need to do it if you’re fine with frequent headaches.
- Immune System Support: Mobility training boosts lymphatic circulation, aiding the immune system. Avoid it if you prefer your immune system to get exciting in a bad way.
- Stress Reduction: Mobility exercises release endorphins and lower cortisol levels, reducing stress. So, it is certainly best to skip it if you prefer feeling stressed and enjoy the many harmful symptoms of high cortisol levels!
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Mobility As Though A Sporting Pursuit: Train For The Event Of Your Life!
Take care!
Share This Post
-
Unlimited Memory – by Kevin Horsley
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Premise: there are easily learnable techniques to rapidly (and greatly) improve one’s memory. We’ve touched on some of these methods before at 10almonds, but being a newsletter rather than a book, we’ve not been able to go as deeply into it as Horsley!
Your memory is far, far, far more powerful than you might realize, and this book will help unlock that. To illustrate…
Some of the book is given over to what are for most purposes “party tricks”, such as remembering pi to 10,000 places. Those things are fun, even if not as practical in today’s world of rarely needing to even know the actual digits of a phone number. However, they do also serve as a good example of just how much of “super memory” isn’t a matter of hard work, so much as being better organized about it.
Most of the book is focused on practical methods to improve the useful aspects of memory—including common mistakes!
If the book has any flaw it’s that the first chapter or so is spent persuading the reader of things we presumably already believe, given that we bought the book. For example, that remembering things is a learnable skill and that memory is functionally limitless. However, we still advise to not skip those chapters as they do contain some useful reframes as well.
Bottom line: if you read this book you will be astonished by how much you just learned—because you’ll be able to recall whole sections in detail! And then you can go apply that whatever areas of your life you wanted to when you bought the book.
Share This Post
Related Posts
-
Should We Skip Shampoo?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝What’s the science on “no poo”? Is it really better for hair? There are so many mixed reports out there.❞
First, for any unfamiliar: this is not about constipation; rather, it is about skipping shampoo, and either:
- Using an alternative cleaning agent, such as vinegar and/or sodium bicarbonate
- Using nothing at all, just conditioner when wet and brushing when dry
Let’s examine why the trend became a thing: the thinking went “shampoo does not exist in nature, and most of our body is more or less self-cleaning; shampoos remove oils from hair, and the body has to produce more sebum to compensate, resulting in a rapid cycle of dry and greasy hair”.
Now let’s fact-check each of those:
- shampoo does not exist in nature: true (except in the sense that everything that exists can be argued to exist in nature, since nature encompasses everything—but the point is that shampoo is a purely artificial human invention)
- most of our body is more or less self-cleaning: true, but our hair is not, for the same reason our nails are not: they’re not really a living part of the overall organism that is our body, so much as a keratinous protrusion of neatly stacked and hardened dead cells from our body. Dead things are not self-cleaning.
- shampoos remove oils from hair: true; that is what they were invented for and they do it well
- the body has to produce more sebum to compensate, resulting in a rapid cycle of dry and greasy hair: false; or at least, there is no evidence for this.
Our hair’s natural oils are great at protecting it, and also great at getting dirt stuck in it. For the former reason we want the oil there; for the latter reason, we don’t.
So the trick becomes: how to remove the oil (and thus the dirt stuck in it) and then put clean oil back (but not too much, because we don’t want it greasy, just, shiny and not dry)?
The popular answer is: shampoo to clean the hair, conditioner to put an appropriate amount of oil* back.
*these days, mostly not actually oil, but rather silicon-based substitutes, that do the same job of protecting hair and keeping it shiny and not brittle, without attracting so much dirt. Remember also that silicon is inert and very body safe; its molecules are simply too large to be absorbed, which is why it gets used in hair products, some skin products, and lube.
See also: Water-based Lubricant vs Silicon-based Lubricant – Which is Healthier?
If you go “no poo”, then what will happen is either you dry your hair out much worse by using vinegar or (even worse) bicarbonate of soda, or you just have oil (and any dirt stuck in it) in your hair for the life of the hair. As in, each individual strand of hair has a lifespan, and when it falls out, the dirt will go with it. But until that day, it’s staying with you, oil and dirt and all.
If you use a conditioner after using those “more natural” harsh cleaners* that aren’t shampoo, then you’ll undo a lot of the damage done, and you’ll probably be fine.
*in fact, if you’re going to skip shampoo, then instead of vinegar or bicarbonate of soda, dish soap from your kitchen may actually do less damage, because at least it’s pH-balanced. However, please don’t use that either.
If you’re going to err one way or the other with regard to pH though, erring on the side of slightly acidic is much better than slightly alkaline.
More on pH: Journal of Trichology | The Shampoo pH can Affect the Hair: Myth or Reality?
If you use nothing, then brushing a lot will mitigate some of the accumulation of dirt, but honestly, it’s never going to be clean until you clean it.
Our recommendation
When your hair seems dirty, and not before, wash it with a simple shampoo (most have far too many unnecessary ingredients; it just needs a simple detergent, and the rest is basically for marketing; to make it foam completely unnecessarily but people like foam, to make it thicker so it feels more substantial, to make it smell nice, to make it a color that gives us confidence it has ingredients in it, etc).
Then, after rinsing, enjoy a nice conditioner. Again there are usually a lot of unnecessary ingredients, but an argument can be made this time for some being more relevant as unlike with the shampoo, many ingredients are going to remain on your hair after rinsing.
Between washes, if you have long hair, consider putting some hair-friendly oil (such as argan oil or coconut oil) on the tips daily, to avoid split ends.
And if you have tight curly hair, then this advice goes double for you, because it takes a lot longer for natural oils to get from your scalp to the ends of your hair. For those of us with straight hair, it pretty much zips straight on down there within a day or two; not so if you have beautiful 4C curls to take care of!
For more on taking care of hair gently, check out:
Gentler Hair Care Options, According To Science
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
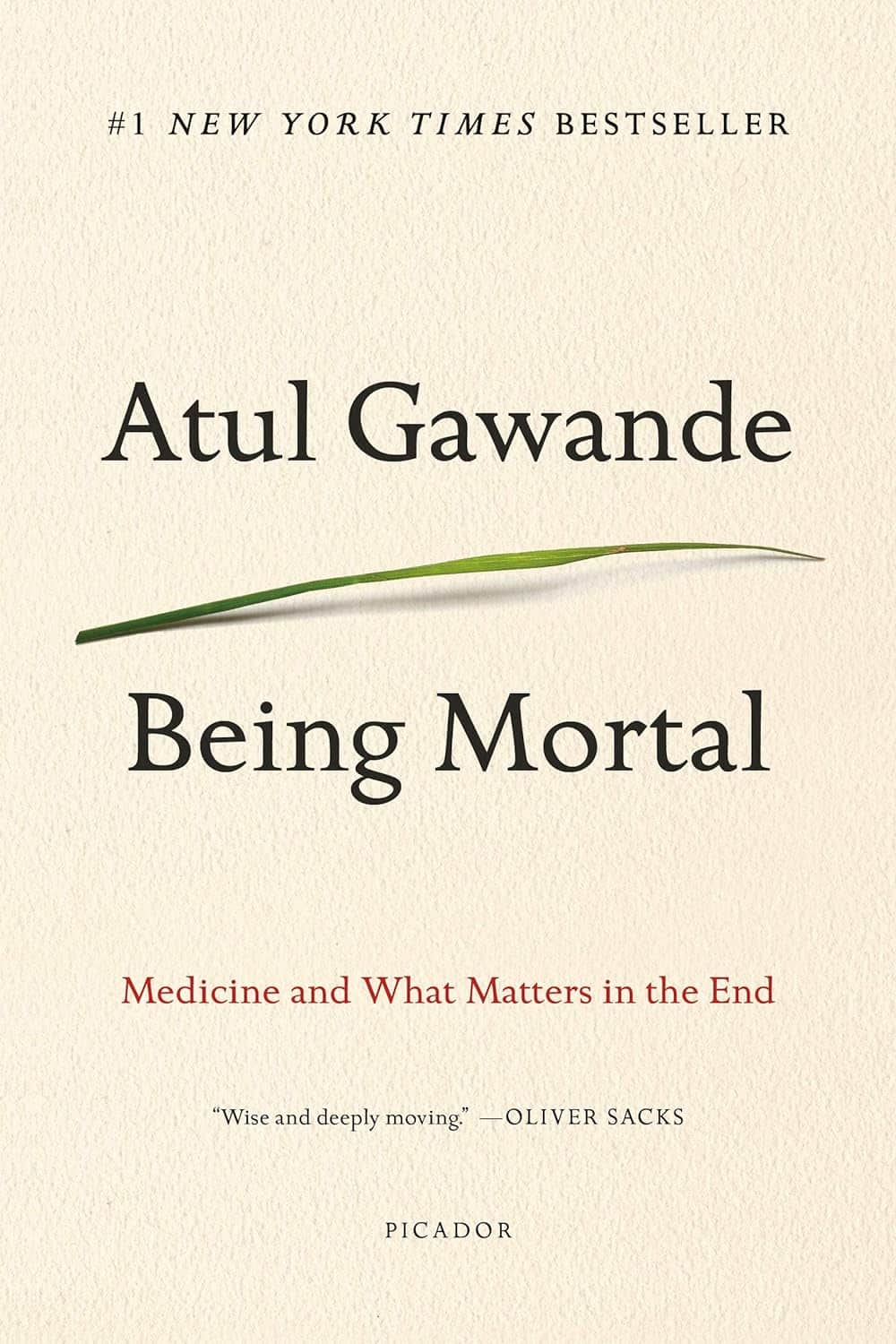
Being Mortal – by Dr. Atul Gawande
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Maybe you want to “live forever or die trying”, and that’s an understandable goal… But are you prepared for “or die trying” being the outcome?
This is not a cheerful book, if you’re anything like this reviewer, you will need a little towel or something to mop up the tears while you read. But it’s worth it.
Dying is one thing; fighting for life is even generally considered a noble endeavor. Suffering alone isn’t fun, losing independence can feel humiliating, and seeing someone who was always a tower of strength, now a frail shadow of their former self, reduced to begging for something that they’re “not allowed”, can be worse.
Do we want that for ourselves? For our loved ones? Can there be a happy medium between that, and the alternative to indeed “go gentle into that good night”?
Dr. Gawande, a surgeon well-acquainted with death and dying, thinks so. But it involves work on our part, and being prepared for hard decisions.
- What is most important to us, and what tradeoffs are we willing to make for it?
- What, even, is actually an option to us with the resources available?
- Can we make peace with a potentially bad lot? And… Should we?
- When is fighting important, and when is it self-destructive?
These (and others) are all difficult questions posed by Dr. Gawande, but critical ones.
We don’t usually quote other people’s reviews when reviewing books here, but let’s consider the following words from the end of a long review on Amazon:
❝If “dying as we lived” is some kind of standard for how we should go, then maybe alone and medicalized makes some sense right now after all.❞
Bottom line: we all deserve better than that. And if we don’t take the time to think about what’s most important, then time will take it from us. This very insightful book may not have all the answers, but it has the questions, and it can help a lot in exploring them and deciding what matters most to us in the end, really.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Latest Alzheimer’s Prevention Research Updates
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Questions and Answers at 10almonds
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
I am now in the “aging” population. A great concern for me is Alzheimers. My father had it and I am so worried. What is the latest research on prevention?
One good thing to note is that while Alzheimer’s has a genetic component, it doesn’t appear to be hereditary per se. Still, good to be on top of these things, and it’s never too early to start with preventive measures!
You might like a main feature we did on this recently:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: