Eat to Live – by Dr. Joel Fuhrman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It sure would be great if we could eat all that we wanted, and remain healthy without putting on weight.
That’s the main intent of Dr. Joel Fuhrman’s book, with some caveats:
- His diet plan gives unlimited amounts of some foods, while restricting others
- With a focus on nutrient density, he puts beans and legumes into the “eat as much as you want” category, and grains (including whole grains) into the “restrict” category
This latter is understandable for a weight-loss diet (as the book’s subtitle promises). The question then is: will it be sustainable?
Current scientific consensus holds for “whole grains are good and an important part of diet”. It does seem fair that beans and legumes should be able to replace grains, for grains’ carbohydrates and fiber.
However, now comes the double-edged aspect: beans and legumes contain more protein than grains. So, we’ll feel fuller sooner, and stay fuller for longer. This means we’ll probably lose weight, and keep losing weight. Or at least: losing fat. Muscle mass will stay or go depending on what you’re doing with your muscles.
If you want to keep your body fat percentage at a certain level and not go below it, you may well need to reintroduce grains to your diet, which isn’t something that Dr. Fuhrman covers in this book.
Bottom line: this is a good, science-based approach for healthily losing weight (specifically, fat) and keeping it off. It might be a little too good at this for some people though.
Click here to check out Eat To Live and decide what point you want to stop losing weight at!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dr. Kim Foster’s Method For Balancing Hormones Naturally
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not just sex hormones, but also hormones like cortisol (the stress hormone), and thyroid hormones (for metabolism regulation) too! The body is most of the time self-regulating when it comes to hormones, but there are things that we can do to help our body look after us correctly.
In short, if we give our body what it needs, it will (usually, barring serious illness!) give us what we need.
Dr. Foster recommends…
Foods:
- Healthy fats (especially avocados and nuts)
- Lean proteins (especially poultry, fish, and legumes)
- Fruits & vegetables (especially colorful ones)
- Probiotics (especially fermented foods like sauerkraut, kimchi, etc)
- Magnesium-rich foods (especially dark leafy greens, nuts, and yes, dark chocolate)
Teas:
- Camomile tea (especially beneficial against cortisol overproduction)
- Nettle tea (especially beneficial for estrogen production)
- Peppermint tea (especially beneficial for gut health, thus indirect hormone benefits)
Stress reduction:
- Breathing exercises (especially mindfulness exercises)
- Yoga (especially combining exercise with stretches)
- Spending time in nature (especially green spaces)
Dr. Foster explains more about all of these things, along with more illustrative examples, so if you can, do enjoy her video:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to read more about this topic?
You might like our main feature: What Does “Balance Your Hormones” Even Mean?
Enjoy!
Share This Post
-
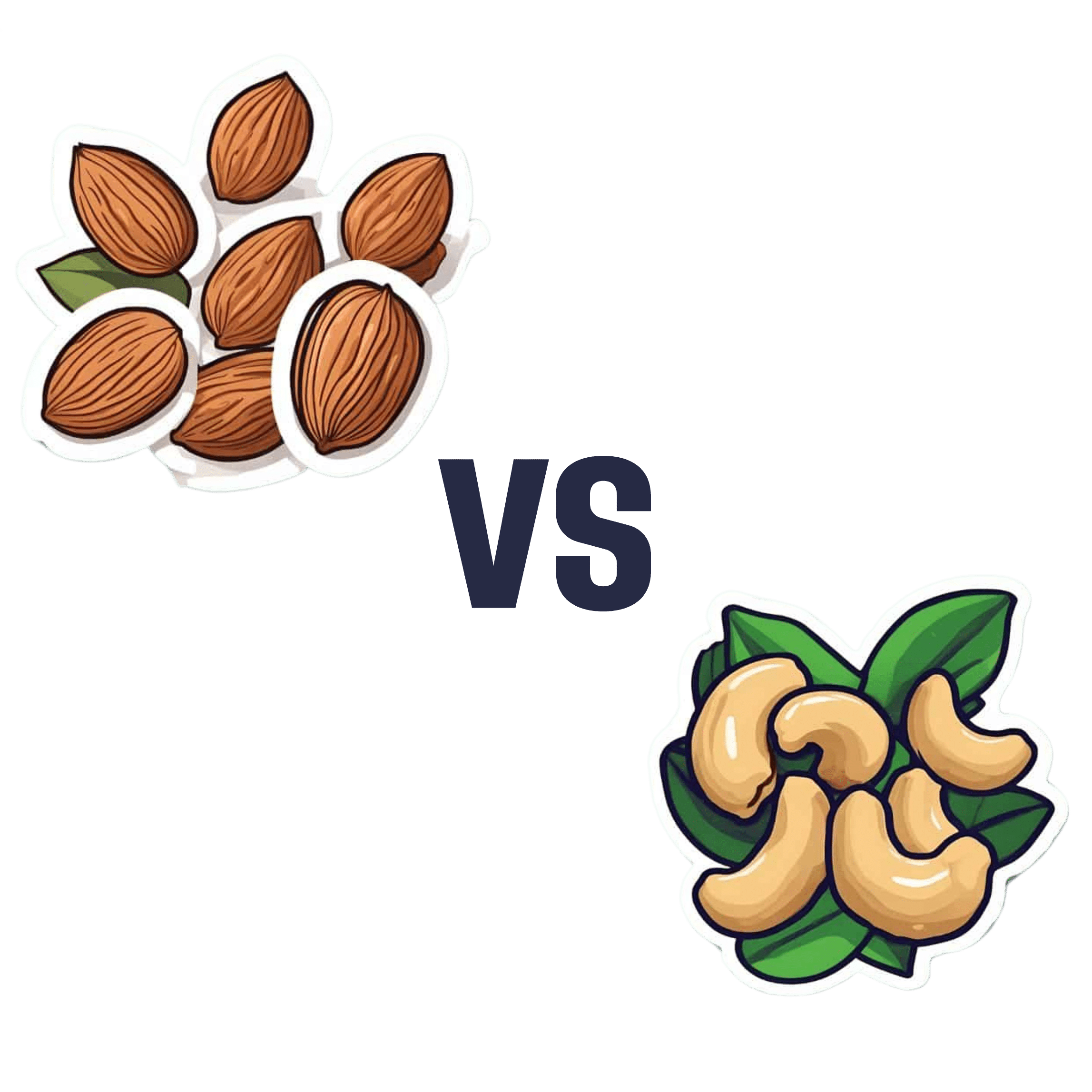
Almonds vs Cashews – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing almonds to cashews, we picked the almonds.
Why?
Both are great! But here’s why we picked the almonds:
In terms of macros, almonds have a little more protein and more than 4x the fiber. Given how critical fiber is to good health, and how most people in industrialized countries in general (and N. America in particular) aren’t getting enough, we consider this a major win for almonds.
Things are closer to even for vitamins, but almonds have a slight edge. Almonds are higher in vitamins A, B2, B3, B9, and especially 27x higher in vitamin E, while cashews are higher in vitamins B1, B5, B6, C & K. So, a moderate win for almonds.
In the category of minerals, cashews do a bit better on average. Cashews have moderately more copper, iron, phosphorus, selenium, and zinc, while almonds boast 6x more calcium, and slightly more manganese and potassium. We say this one’s a slight win for cashews.
Adding the categories up, however, makes it clear that almonds win the day.
However, of course, enjoy both! Diversity is healthy. Just, if you’re going to choose between them, we recommend almonds.
Want to learn more?
You might like to read:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Almonds vs Walnuts – Which is Healthier?
- Pistachios vs Cashews – Which is Healthier?
- Why You Should Diversify Your Nuts!
- What Matters Most For Your Heart?
Take care!
Share This Post
-
Elon Musk says ‘disc replacement’ worked for him. But evidence this surgery helps chronic pain is lacking
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Last week in a post on X, owner of the platform Elon Musk recommended people look into disc replacement if they’re experiencing severe neck or back pain.
According to a biography of the billionaire, he’s had chronic back and neck pain since he tried to “judo throw” a 350-pound sumo wrestler in 2013 at a Japanese-themed party for his 42nd birthday, and blew out a disc at the base of his neck.
In comments following the post, Musk said the surgery was a “gamechanger” and reduced his pain significantly.
Musk’s original post has so far had more than 50 million views and generated controversy. So what is disc replacement surgery and what does the evidence tells us about its benefits and harms?
What’s involved in a disc replacement?
Disc replacement is a type of surgery in which one or more spinal discs (a cushion between the spine bones, also known as vertebrae) are removed and replaced with an artificial disc to retain movement between the vertebrae. Artificial discs are made of metal or a combination of metal and plastic.
Disc replacement may be performed for a number of reasons, including slipped discs in the neck, as appears to be the case for Musk.
Disc replacement is major surgery. It requires general anaesthesia and the operation usually takes 2–4 hours. Most people stay in hospital for 2–7 days. After surgery patients can walk but need to avoid things like strenuous exercise and driving for 3–6 weeks. People may be required to wear a neck collar (following neck surgery) or a back brace (following back surgery) for about 6 weeks.
Costs vary depending on whether you have surgery in the public or private health system, if you have private health insurance, and your level of coverage if you do. In Australia, even if you have health insurance, a disc replacement surgery may leave you more than A$12,000 out of pocket.
Disc replacement surgery is not performed as much as other spinal surgeries (for example, spinal fusion) but its use is increasing.
In New South Wales for example, rates of privately-funded disc replacement increased six-fold from 6.2 per million people in 2010–11 to 38.4 per million in 2019–20.
What are the benefits and harms?
People considering surgery will typically weigh that option against not having surgery. But there has been very little research comparing disc replacement surgery with non-surgical treatments.
Clinical trials are the best way to determine if a treatment is effective. You first want to show that a new treatment is better than doing nothing before you start comparisons with other treatments. For surgical procedures, the next step might be to compare the procedure to non-surgical alternatives.
Unfortunately, these crucial first research steps have largely been skipped for disc replacement surgery for both neck and back pain. As a result, there’s a great deal of uncertainty about the treatment.
There are no clinical trials we know of investigating whether disc replacement is effective for neck pain compared to nothing or compared to non-surgical treatments.
For low back pain, the only clinical trial that has been conducted to our knowledge comparing disc replacement to a non-surgical alternative found disc replacement surgery was slightly more effective than an intensive rehabilitation program after two years and eight years.
Many people experience chronic pain. Yan Krukau/Pexels Complications are not uncommon, and can include disclocation of the artificial disc, fracture (break) of the artificial disc, and infection.
In the clinical trial mentioned above, 26 of the 77 surgical patients had a complication within two years of follow up, including one person who underwent revision surgery that damaged an artery leading to a leg needing to be amputated. Revision surgery means a re-do to the primary surgery if something needs fixing.
Are there effective alternatives?
The first thing to consider is whether you need surgery. Seeking a second opinion may help you feel more informed about your options.
Many surgeons see disc replacement as an alternative to spinal fusion, and this choice is often presented to patients. Indeed, the research evidence used to support disc replacement mainly comes from studies that compare disc replacement to spinal fusion. These studies show people with neck pain may recover and return to work faster after disc replacement compared to spinal fusion and that people with back pain may get slightly better pain relief with disc replacement than with spinal fusion.
However, spinal fusion is similarly not well supported by evidence comparing it to non-surgical alternatives and, like disc replacement, it’s also expensive and associated with considerable risks of harm.
Fortunately for patients, there are new, non-surgical treatments for neck and back pain that evidence is showing are effective – and are far cheaper than surgery. These include treatments that address both physical and psychological factors that contribute to a person’s pain, such as cognitive functional therapy.
While Musk reported a good immediate outcome with disc replacement surgery, given the evidence – or lack thereof – we advise caution when considering this surgery. And if you’re presented with the choice between disc replacement and spinal fusion, you might want to consider a third alternative: not having surgery at all.
Giovanni E Ferreira, NHMRC Emerging Leader Research Fellow, Institute of Musculoskeletal Health, University of Sydney; Christine Lin, Professor, Institute for Musculoskeletal Health, University of Sydney; Christopher Maher, Professor, Sydney School of Public Health, University of Sydney; Ian Harris, Professor of Orthopaedic Surgery, UNSW Sydney, and Joshua Zadro, NHMRC Emerging Leader Research Fellow, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Older, Faster, Stronger – by Margaret Webb
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, now in her 60s, made it her mission in her 50s to become the best runner she could. Before that, she’d been a keen runner previously, but let things slip rather in her 40s. But the book’s not about her 40s, it’s about her 50s and onwards, and other female runners in their 50s, 60s, 70s, 80s, and even 90s.
There’s a lot of this book that’s about people’s individual stories, and those should certainly be enough to prompt almost any reader that “if they can do it, I can”.
A lot, meanwhile, is about health and exercise science, training methods, and what has worked for various later-life athletes, including the author. So, it’s also partway instruction manual, with plenty of reference to science and medical considerations too.
Bottom line: sometimes, life throws us challenges. Sometimes, the best response is “Yeah? Bet” and surprise everyone.
Click here to check out Older, Faster, Stronger, and become all those cool things!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Should We Skip Shampoo?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝What’s the science on “no poo”? Is it really better for hair? There are so many mixed reports out there.❞
First, for any unfamiliar: this is not about constipation; rather, it is about skipping shampoo, and either:
- Using an alternative cleaning agent, such as vinegar and/or sodium bicarbonate
- Using nothing at all, just conditioner when wet and brushing when dry
Let’s examine why the trend became a thing: the thinking went “shampoo does not exist in nature, and most of our body is more or less self-cleaning; shampoos remove oils from hair, and the body has to produce more sebum to compensate, resulting in a rapid cycle of dry and greasy hair”.
Now let’s fact-check each of those:
- shampoo does not exist in nature: true (except in the sense that everything that exists can be argued to exist in nature, since nature encompasses everything—but the point is that shampoo is a purely artificial human invention)
- most of our body is more or less self-cleaning: true, but our hair is not, for the same reason our nails are not: they’re not really a living part of the overall organism that is our body, so much as a keratinous protrusion of neatly stacked and hardened dead cells from our body. Dead things are not self-cleaning.
- shampoos remove oils from hair: true; that is what they were invented for and they do it well
- the body has to produce more sebum to compensate, resulting in a rapid cycle of dry and greasy hair: false; or at least, there is no evidence for this.
Our hair’s natural oils are great at protecting it, and also great at getting dirt stuck in it. For the former reason we want the oil there; for the latter reason, we don’t.
So the trick becomes: how to remove the oil (and thus the dirt stuck in it) and then put clean oil back (but not too much, because we don’t want it greasy, just, shiny and not dry)?
The popular answer is: shampoo to clean the hair, conditioner to put an appropriate amount of oil* back.
*these days, mostly not actually oil, but rather silicon-based substitutes, that do the same job of protecting hair and keeping it shiny and not brittle, without attracting so much dirt. Remember also that silicon is inert and very body safe; its molecules are simply too large to be absorbed, which is why it gets used in hair products, some skin products, and lube.
See also: Water-based Lubricant vs Silicon-based Lubricant – Which is Healthier?
If you go “no poo”, then what will happen is either you dry your hair out much worse by using vinegar or (even worse) bicarbonate of soda, or you just have oil (and any dirt stuck in it) in your hair for the life of the hair. As in, each individual strand of hair has a lifespan, and when it falls out, the dirt will go with it. But until that day, it’s staying with you, oil and dirt and all.
If you use a conditioner after using those “more natural” harsh cleaners* that aren’t shampoo, then you’ll undo a lot of the damage done, and you’ll probably be fine.
*in fact, if you’re going to skip shampoo, then instead of vinegar or bicarbonate of soda, dish soap from your kitchen may actually do less damage, because at least it’s pH-balanced. However, please don’t use that either.
If you’re going to err one way or the other with regard to pH though, erring on the side of slightly acidic is much better than slightly alkaline.
More on pH: Journal of Trichology | The Shampoo pH can Affect the Hair: Myth or Reality?
If you use nothing, then brushing a lot will mitigate some of the accumulation of dirt, but honestly, it’s never going to be clean until you clean it.
Our recommendation
When your hair seems dirty, and not before, wash it with a simple shampoo (most have far too many unnecessary ingredients; it just needs a simple detergent, and the rest is basically for marketing; to make it foam completely unnecessarily but people like foam, to make it thicker so it feels more substantial, to make it smell nice, to make it a color that gives us confidence it has ingredients in it, etc).
Then, after rinsing, enjoy a nice conditioner. Again there are usually a lot of unnecessary ingredients, but an argument can be made this time for some being more relevant as unlike with the shampoo, many ingredients are going to remain on your hair after rinsing.
Between washes, if you have long hair, consider putting some hair-friendly oil (such as argan oil or coconut oil) on the tips daily, to avoid split ends.
And if you have tight curly hair, then this advice goes double for you, because it takes a lot longer for natural oils to get from your scalp to the ends of your hair. For those of us with straight hair, it pretty much zips straight on down there within a day or two; not so if you have beautiful 4C curls to take care of!
For more on taking care of hair gently, check out:
Gentler Hair Care Options, According To Science
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
South Indian-Style Chickpea & Mango Salad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We have a double-dose of chickpeas today, but with all the other ingredients, this dish is anything but boring. Fun fact about chickpeas though: they’re rich in sitosterol, a plant sterol that, true to its name, sits on cholesterol absorption sites, reducing the amount of dietary cholesterol absorbed. If you are vegan, this will make no difference to you because your diet does not contain cholesterol, but for everyone else, this is a nice extra bonus!
You will need
- 1 can white chickpeas, drained and rinsed
- 1 can black chickpeas (kala chana), drained and rinsed
- 9 oz fresh mango, diced (or canned is fine if that’s what’s available)
- 1½ oz ginger, peeled and grated
- 2 green chilis, finely chopped (adjust per heat preferences)
- 2 tbsp desiccated coconut (or 3 oz grated coconut, if you have it fresh)
- 8 curry leaves (dried is fine if that’s what’s available)
- 1 tsp mustard seeds
- 1 tsp cumin seeds
- 1 tsp black pepper, coarse ground
- ½ tsp MSG or 1 tsp low-sodium salt
- Juice of 1 lime
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a skillet over a medium heat. When it’s hot but not smoking, add the ginger, chilis, curry leaves, mustard seeds, and cumin seeds, stirring well to combine, keep going until the mustard seeds start popping.
2) Add the chickpeas (both kinds), as well as the black pepper and the MSG/salt. Once they’re warm through, take it off the heat.
3) Add the mango, coconut, and lime juice, mixing thoroughly.
4) Serve warm, at room temperature, or cold:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- What Matters Most For Your Heart?
- Can Saturated Fats Be Healthy?
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: