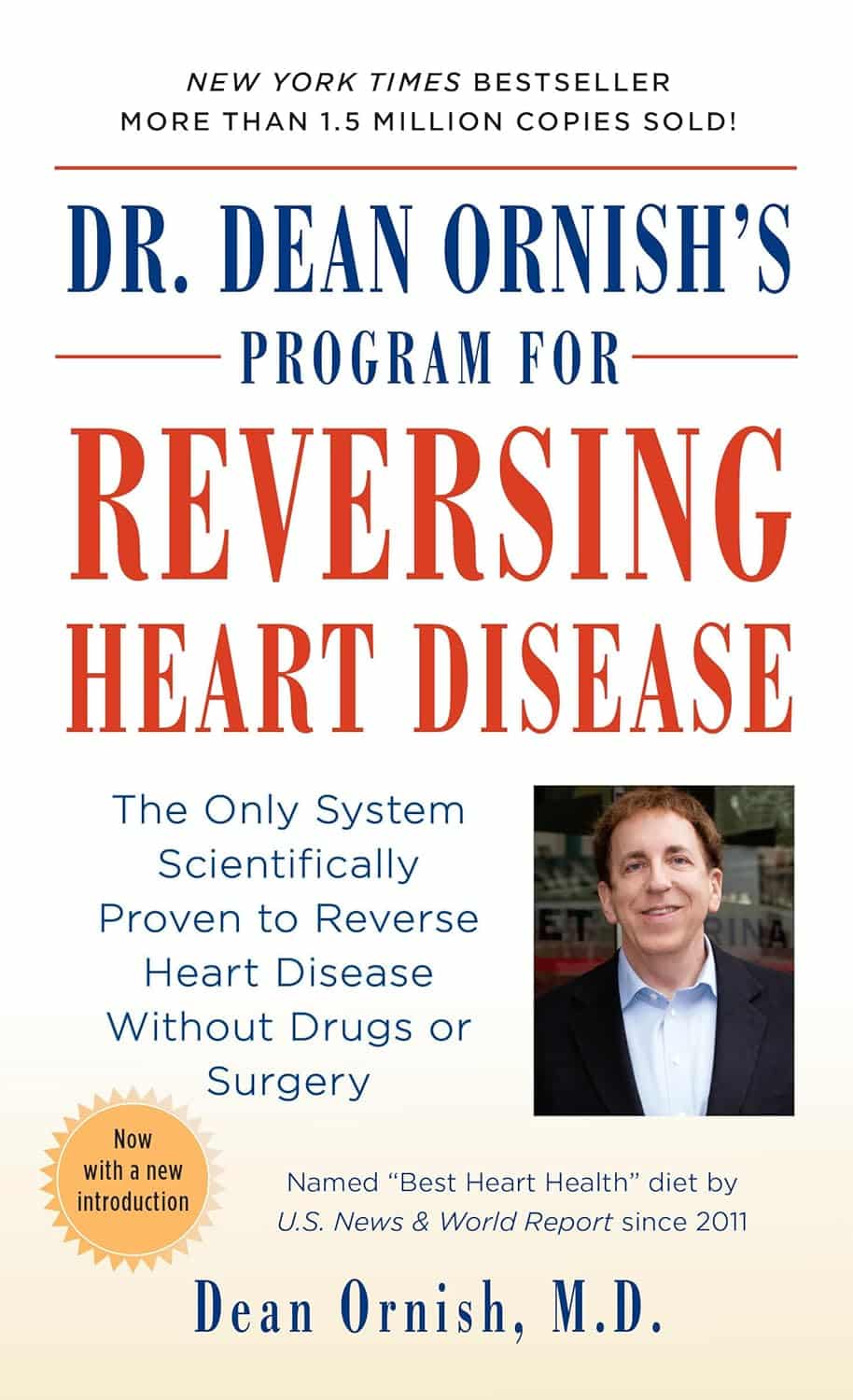
Dr. Dean Ornish’s Program For Reversing Heart Disease – by Dr. Dean Ornish
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Dr. Ornish’s “Undo It!” which is about reversing many kinds of chronic diseases (not all, alas, but quite a few) by undercutting their common etiologies, such as inflammation, insulin resistance, and so forth.
This book is entirely consistent with that one, but the focus here is (as the title says) specifically on reversing heart disease.
Of course, it does not require you to already have heart disease—if you do, well, getting onto this is better sooner than later. If you don’t, and are “merely” in a risk zone, or even just want to be proactive about your heart health, then this book will stand you in good stead.
The book covers all the lifestyle things you’d expect it to (especially diet, but also exercise, and not just “quit smoking” but also how, things like that), and possibly some things you might not expect (chapters on more psychological factors that have a big impact on heart health).
There are recipes (157 pages of them; they are plant-based and good) and there is a 21-day meal plan to get you going.
The style is a little dated (written in the 90s), but the content doesn’t suffer for it, having been updated over the years in any case.
Bottom line: if you want a holistic approach to taking care of your heart that’s not extreme and/but is very effective, then well, you’ve found it.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
High-Protein Plant-Based Diet for Beginners – by Maya Howard with Ariel Warren
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Seasoned vegans (well-seasoned vegans?) will know that getting enough protein from a plant-based diet is really not the challenge that many think it is, but for those just embarking on cutting out the meat, it’s not useful to say “it’s easy!”; it’s useful to show how.
That’s what this book does. And not just by saying “these foods” and leaving people to wonder if they need to eat a pound of tofu each day to get their protein in. Instead, recipes. Enough for a 4-week meal plan, and the idea is that after a month of eating that way, it won’t be nearly so mysterious.
The recipes are very easy to execute, while still having plenty of flavor (which is what happens when one uses a lot of flavorsome main ingredients and then seasons them well too). The ingredients are not obscure, and you should be able to find everything easily in any medium-sized supermarket.
As for the well-roundedness of the diet, we’ll mention that the “with Ariel Warren” in the by-line means that while the book was principally authored by Maya Howard (who is, at time of writing, a nutritionist-in-training), she had input throughout from Ariel Warren (a Registered Dietician Nutritionist) to ensure she didn’t go off-piste anyway and it gets the professional stamp of approval.
Bottom line: if you’d like to cook plant based while still prioritizing protein and you’re not sure how to make that exciting and fun instead of a chore, then this book will show you how to please your taste buds and improve your body composition at the same time.
Click here to check out High-Protein Plant-Based Diet for Beginners, and dig in!
Share This Post
-
Reading At Night: Good Or Bad For Sleep? And Other Questions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Would be interested in your views about “reading yourself to sleep”. I find that current affairs magazines and even modern novels do exactly the opposite. But Dickens – ones like David Copperfield and Great Expectations – I find wonderfully effective. It’s like entering a parallel universe where none of your own concerns matter. Any thoughts on the science that may explain this?!❞
Anecdotally: this writer is (like most writers) a prolific reader, and finds reading some fiction last thing at night is a good way to create a buffer between the affairs of the day and the dreams of night—but I could never fall asleep that way, unless I were truly sleep-deprived. The only danger is if I “one more chapter” my way deep into the night! For what it’s worth, bedtime reading for me means a Kindle self-backlit with low, soft lighting.
Scientifically: this hasn’t been a hugely researched area, but there are studies to work from. But there are two questions at hand (at least) here:
- one is about reading, and
- the other is about reading from electronic devices with or without blue light filters.
Here’s a study that didn’t ask the medium of the book, and concluded that reading a book in bed before going to sleep improved sleep quality, compared to not reading a book in bed:
Here’s a study that concluded that reading on an iPad (with no blue light filter) that found no difference in any metrics except EEG (so, there was no difference on time spent in different sleep states or sleep onset latency), but advised against it anyway because of the EEG readings (which showed slow wave activity being delayed by approximately 30 minutes, which is consistent with melatonin production mechanics):
Here’s another study that didn’t take EEG readings, and/but otherwise confirmed no differences being found:
We’re aware this goes against general “sleep hygiene” advice in two different ways:
- General advice is to avoid electronic devices before bedtime
- General advice is to not do activities besides sleep (and sex) in bed
…but, we’re committed to reporting the science as we find it!
Enjoy!
Share This Post
-
Stop Sabotaging Your Gut
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
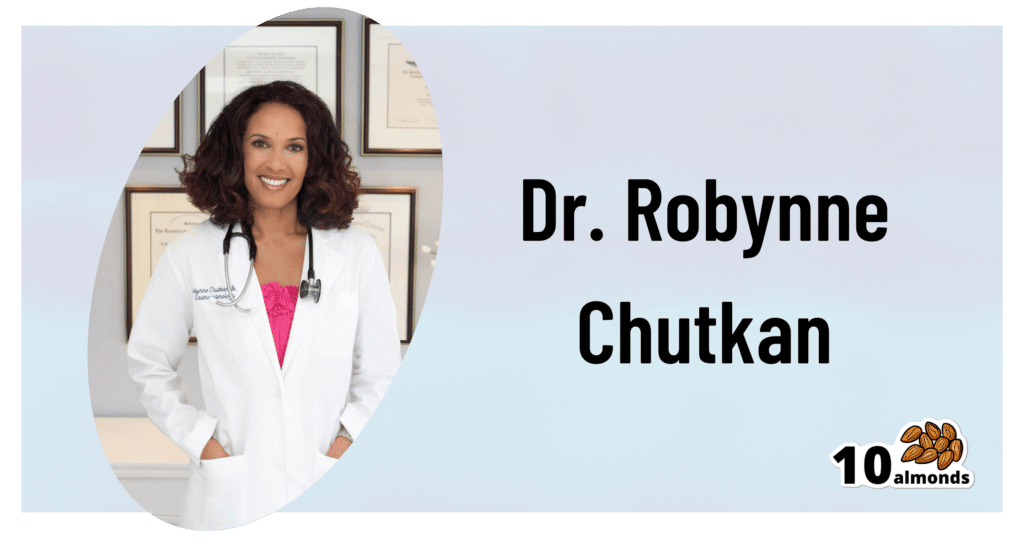
This is Dr. Robynne Chutkan. She’s an integrative gastroenterologist, and founder of the Digestive Center for Wellness, in Washington DC, which for the past 20 years has been dedicated to uncovering the root causes of gastrointestinal disorders, while the therapeutic side of things has been focused on microbial optimization, nutritional therapy, mind-body techniques, and lifestyle changes.
In other words, maximal health for minimal medicalization.
So… What does she want us to know?
Live dirty
While attentive handwashing is important to avoid the spread of communicable diseases*, excessive cleanliness in general can result in an immune system that has no idea how to deal with pathogens when exposure does finally occur.
*See also: The Truth About Handwashing
This goes doubly for babies: especially those who were born by c-section and thus missed out on getting colonized by vaginal bacteria, and especially those who are not breast-fed, and thus miss out on nutrients given in breast milk that are made solely for the benefit of certain symbiotic bacteria (humans can’t even digest those particular nutrients, we literally evolved to produce some nutrients solely for the bacteria).
See also: Breast Milk’s Benefits That Are (So Far) Not Replicable
However, it still goes for the rest of us who are not babies, too. We could, Dr. Chutkan tells us, stand to wash less in general, and definitely ease up on antibacterial soaps and so forth.
See also: Should You Shower Daily?
Take antibiotics only if absolutely necessary (and avoid taking them by proxy)
Dr. Chutkan describes antibiotics as the single biggest threat to our microbiome, not just because of overprescription, but also the antibiotics that are used in animal agriculture and thus enter the food chain (and thus, enter us, if we eat animal products).
Still, while the antibiotics meat/dairy-enjoyers will get from food are better avoided, antibiotics actually taken directly are even worse, and are absolutely a “scorched earth” tactic against whatever they’re being prescribed for.
See also: Antibiotics? Think Thrice ← which also brings up “Four Ways Antibiotics Can Kill You”; seriously, the risks of antibiotics are not to be underestimated, including the risks associated only with them working exactly as intended—let alone if something goes wrong.
Probiotics won’t save you
While like any gastroenterologist (or really, almost any person in general), she notes that probiotics can give a boost to health. However, she wants us to know about two shortcomings that are little-discussed:
1) Your body has a collection of microbiomes each with their own needs, and while it is possible to take “generally good” bacteria in probiotics and assume they’ll do good, taking Lactobacillus sp. will do nothing for a shortage of Bifidobacteria sp, and even taking the correct genus can have similar shortcomings if a different species of that genus is needed, e.g. taking L. acidophilus will do nothing for a shortage of L. reuteri.
It’d be like a person with a vitamin D deficiency taking vitamin B12 supplements and wondering why they’re not getting better.
2) Probiotics are often wasted if not taken mindfully of their recipient environment. For example, most gut bacteria only live for about 20 minutes in the gut. They’re usually inactive in the supplement form, they’re activated in the presence of heat and moisture and appropriate pH etc, and then the clock is ticking for them to thrive or die.
This means that if you take a supplement offering two billion strains of good gut bacteria, and you take it on an empty stomach, then congratulations, 20 minutes later, they’re mostly dead, because they had nothing to eat. Or if you take it after drinking a soda, congratulations, they’re mostly dead because not only were they starved, but also their competing “bad” microbes weren’t starved and changed the environment to make it worse for the “good” ones.
For this reason, taking probiotics with (or immediately after) plenty of fiber is best.
This is all accentuated if you’re recovering from using antibiotics, by the way.
Imagine: a nuclear war devastates the population of the Earth. Some astronauts manage to safely return, finding a mostly-dead world covered in nuclear winter. Is the addition of a few astronauts going to quickly repopulate the world? No, of course not. They are few, the death toll is many, and the environment is very hostile to life. A hundred years later, the population will be pretty much the same—a few straggling survivors.
It’s the same after taking antibiotics, just, generations pass in minutes instead of decades. You can’t wipe out almost everything beneficial in the gut, create a hostile environment there, throw in a couple of probiotic gummies, and expect the population to bounce back.
That said, although “probiotics will not save you”, they can help provided you give them a nice soft bed of fiber to land on, some is better than none, and guessing at what strains are needed is better than giving nothing.
See also: How Much Difference Do Probiotic Supplements Make, Really?
What she recommends
So to recap, we’ve had:
- Wash less, and/or with less harsh chemicals
- Avoid antibiotics like the plague, unless you literally have The Plague, for which the treatment is indeed antibiotics
- Avoid antibiotic-contaminated foods, which in the US is pretty much all animal products unless it’s, for example, your own back-yard hens whom you did not give antibiotics. Do not fall for greenwashing aesthetics in the packaging of “happy cows” and their beef, milk, etc, “happy hens” and their meat, eggs, etc… If it doesn’t explicitly claim to be free from the use of antibiotics, then antibiotics were almost certainly used.
- Dr. Chutkan herself is not even vegan, by the way, but very much wants us to be able to make informed choices about this, and does recommend at least a “plants-forward” diet, for the avoiding-antibiotics reason and for the plenty-of-fiber reason, amongst others.
- Consider probiotics, but don’t expect them to work miracles by themselves; you’ve got to help them to help you.
- Dr. Chutkan also recommends getting microbiome tests done if you think something might be amiss, and then you can supplement with probiotics in a more targetted fashion instead of guessing at what species is needed where.
She also recommends, of course, a good gut-healthy diet in general, especially “leafy green things that were recently alive; not powders”, beans, and nuts, while avoiding gut-unhealthy things such as sugars-without-fiber, alcohol, or some gut-harmful additives (such as most artificial sweeteners, although stevia is a gut-healthy exception, and sucralose is ok in moderation).
For more on gut-healthy eating, check out:
Make Friends With Your Gut (You Can Thank Us Later)
Want to know more from Dr. Chutkan?
We recently reviewed an excellent book of hers:
The Anti-Viral Gut: Tackling Pathogens From The Inside Out – by Dr. Robynne Chutkan
Enjoy!
Share This Post
Related Posts
-
10 Ways To Balance Blood Sugars
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Let Them Eat Cake”, She Said…
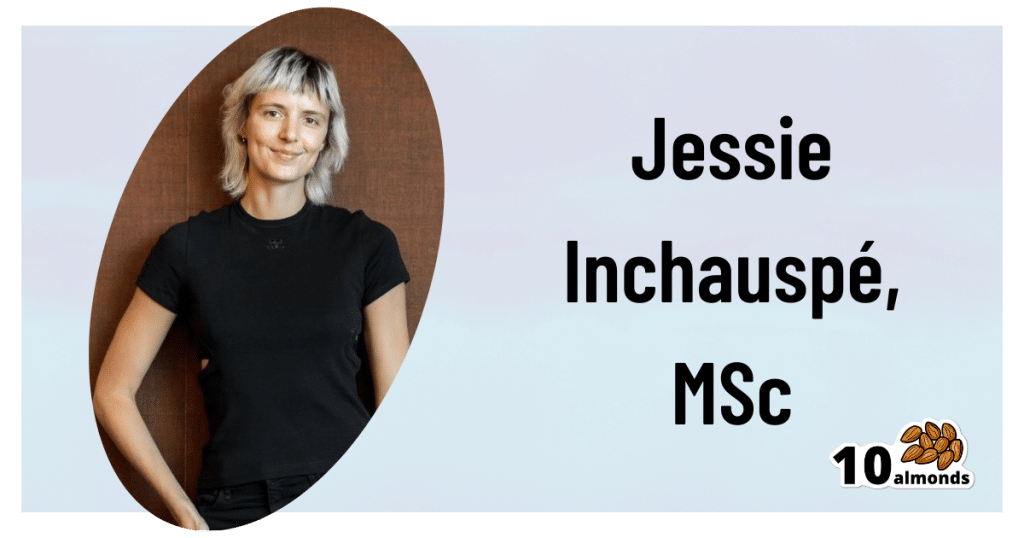
This is Jessie Inchauspé, a French biochemist and author. She’s most known for her best-selling “Glucose Revolution: The Life-Changing Power Of Balancing Your Blood Sugar”.
It’s a great book (which we reviewed recently) and you absolutely should read it, but meanwhile, we’re going to distill at least the most critical core ideas, 10almonds style. In this case, her “ten hacks”:
Eat foods in the right order
The order is:
- Fiber first
- Protein and fat second
- Starches and sugars last
What happens here is… the fiber perks up the gut bacteria, the protein and fat will then be better-digested next, and the starches and sugars will try to jump the line, but they can’t because the fiber is a physical speedbump and the proteins and fats are taking the prime place for being digested. So instead, the starches and sugars—usually responsible for blood sugar spikes—get processed much more gradually, resulting in a nice even curve.
Add a green starter to all your meals
We know what you’re thinking: “that’s just the first one again”, but no. This is an extra starter, before you get to that. If you’re the cook of the household, this can absolutely simply mean snacking on green ingredients while cooking.
Stop counting calories
Especially, she advises: stop worrying about extra calories from fats, such as if doing an oil-and-vinegar dressing for salad—which she also recommends, because all three components (the oil, the vinegar, and the salad) help even out blood sugar levels.
Flatten your breakfast curve
For many, breakfast is the starchiest meal of the day, if not the sugariest. Inchauspé recommends flipping this (ideally) or softening it (if you really must have a carb-based breakfast):
- Top choices include: a warm vegetable salad, fish, or eggs (or tofu if you don’t do animal products).
- Next-best include: if you must have toast, make sure to have butter (and/or the aforementioned egg/tofu, for example) to give your digestion an extra thing to do.
- Also: she recommends skipping the juice in favour of home-made breakfast smoothies. That way, instead of basically just sugar with some vitamins, you’re getting a range of nutrients that, if you stack it right, can constitute a balanced meal itself, with fiber + protein + fat + carbs.
Have any type of sugar—they’re all the same
They’re technically not, but the point is that your body will immediately take them apart and then they will be just the same. Whether it’s the cheapest white sugar or the most expensive organic lovingly hand-reared free-range agave nectar, your body is going to immediately give it the chop-shop treatment (a process so quick as to be practically instantaneous) and say “this is now glucose”.
Pick a dessert over a sweet snack
Remember that about the right order for foods? A dessert, when your body is already digesting dinner, is going to make much less of a glucose spike than, say, a blueberry muffin when all you’ve had this morning is coffee and juice.
Reach for the vinegar before you eat
We recently did a whole main feature about this, so we’ll not double up today!
After you eat, move
The glucose you eat will be used to replace lost muscle glycogen, before any left over is stored as fat… and, while it’s waiting to be stored as fat, just sitting in your bloodstream being high blood sugars. So, this whole thing will go a lot better if you are actively using muscle glycogen (by moving your body).
Inchauspé gives a metaphor: imagine a steam train worker, shoveling coal into the furnace. Meanwhile, other workers are bringing more coal. If the train is moving quickly, the coal can be shoveled into the furnace and burned and won’t build up so quickly. But if the train is moving slowly or not at all, that coal is just going to build up and build up, until the worker can shovel no more because of being neck-deep in coal.
Same with your blood sugars!
If you want to snack, go low-sugar
In the category of advice that will shock nobody: sugary snacks aren’t good for avoiding blood sugar spikes! This one probably didn’t need a chapter devoted to it, but anyway: low sugar is indeed the way to go for snacks.
Put some clothes on your carbs
This is about olive oil on pasta, butter on potatoes, and so forth. Basically, anything starchy is going to be broken down quickly to sugar and sent straight into the bloodstream, if there’s nothing to slow it down. If you’re wondering what to do with rice: adding a tablespoon of chia seeds to the rice while cooking (so they’re cooked together) will add very healthy fats to your rice, and (because they’ve been cooked) will not seem like eating seeds, by the way. In terms of texture and appearance, it’ll be as though you threw some black pepper in*
*which you should also do for many reasons, but that’s beyond the scope of this “about blood sugars” feature!
Wanting to know more about the science of this?
We’ve done all we have room for here today, but Inchauspé is, as ever, happy to explain it herself:
Prefer text? Check out:
The Science Behind Glucose GoddessDon’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Antidepressants: Personalization Is Key!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Antidepressants: Personalization Is Key!
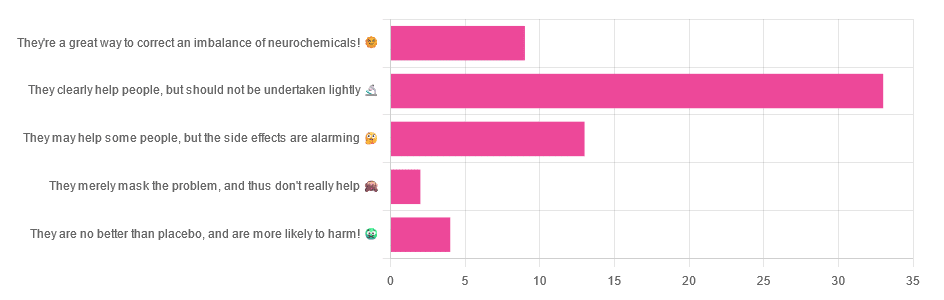
Yesterday, we asked you for your opinions on antidepressants, and got the above-depicted, below-described, set of responses:
- Just over half of respondents said “They clearly help people, but should not be undertaken lightly”
- Just over a fifth of respondents said “They may help some people, but the side effects are alarming”
- Just under a sixth of respondents said “They’re a great way to correct an imbalance of neurochemicals”
- Four respondents said “They are no better than placebo, and are more likely to harm”
- Two respondents said “They merely mask the problem, and thus don’t really help”
So what does the science say?
❝They are no better than placebo, and are more likely to harm? True or False?❞
True or False depending on who you are and what you’re taking. Different antidepressants can work on many different systems with different mechanisms of action. This means if and only if you’re not taking the “right” antidepressant for you, then yes, you will get only placebo benefits:
- Placebo Effect in the Treatment of Depression and Anxiety ← randomly assigned antidepressants are, shockingly, luck of the draw in usefulness
- Antidepressants versus placebo in major depression: an overview ← “wow this science is messy”
- Comparative efficacy and acceptability of 21 antidepressant drugs: a systematic review and network meta-analysis ← “oh look, it makes a difference which antidepressant we give to people”
Rather than dismissing antidepressants as worthless, therefore, it is a good idea to find out (by examination or trial and error) what kind of antidepressant you need, if you indeed do need such.
Otherwise it is like getting a flu shot and being surprised when you still catch a cold!
❝They merely mask the problem, and thus don’t really help: True or False?❞
False, categorically.
The problem in depressed people is the depressed mood. This may be influenced by other factors, and antidepressants indeed won’t help directly with those, but they can enable the person to better tackle them (more on this later).
❝They may help some people, but the side-effects are alarming: True or False?❞
True or False depending on more factors than we can cover here.
Side-effects vary from drug to drug and person to person, of course. As does tolerability and acceptability, since to some extent these things are subjective.
One person’s dealbreaker may be another person’s shrugworthy minor inconvenience at most.
❝They’re a great way to correct an imbalance of neurochemicals: True or False?❞
True! Contingently.
That is to say: they’re a great way to correct an imbalance of neurochemicals if and only if your problem is (at least partly) an imbalance of neurochemicals. If it’s not, then your brain can have all the neurotransmitters it needs, and you will still be depressed, because (for example) the other factors* influencing your depression have not changed.
*common examples include low self-esteem, poor physical health, socioeconomic adversity, and ostensibly bleak prospects for the future.
For those for whom the problem is/was partly a neurochemical imbalance and partly other factors, the greatest help the antidepressants give is getting the brain into sufficient working order to be able to tackle those other factors.
Want to know more about the different kinds?
Here’s a helpful side-by-side comparison of common antidepressants, what type they are, and other considerations:
Mind | Comparing Antidepressants
Want a drug-free approach?
You might like our previous main feature:
The Mental Health First-Aid That You’ll Hopefully Never Need
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Stickers and wristbands aren’t a reliable way to prevent mosquito bites. Here’s why
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Protecting yourself and family from mosquito bites can be challenging, especially in this hot and humid weather. Protests from young children and fears about topical insect repellents drive some to try alternatives such as wristbands, patches and stickers.
These products are sold online as well as in supermarkets, pharmacies and camping stores. They’re often marketed as providing “natural” protection from mosquitoes.
But unfortunately, they aren’t a reliable way to prevent mosquito bites. Here’s why – and what you can try instead.
Why is preventing mosquito bites important?
Mosquitoes can spread pathogens that make us sick. Japanese encephalitis and Murray Valley encephalitis viruses can have potentially fatal outcomes. While Ross River virus won’t kill you, it can cause potentially debilitating illnesses.
Health authorities recommend preventing mosquito bites by: avoiding areas and times of the day when mosquitoes are most active; covering up with long sleeved shirts, long pants, and covered shoes; and applying a topical insect repellent (a cream, lotion, or spray).
I don’t want to put sticky and smelly repellents on my skin!
While for many people, the “sting” of a biting mosquitoes is enough to prompt a dose of repellent, others are reluctant. Some are deterred by the unpleasant feel or smell of insect repellents. Others believe topical repellents contain chemicals that are dangerous to our health.
However, many studies have shown that, when used as recommended, these products are safe to use. All products marketed as mosquito repellents in Australia must be registered by the Australian Pesticides and Veterinary Medicines Authority; a process that provides recommendations for safe use.
How do topical repellents work?
While there remains some uncertainty about how the chemicals in topical insect repellents actually work, they appear to either block the sensory organs of mosquitoes that drive them to bite, or overpower the smells of our skin that helps mosquitoes find us.
Diethytolumide (DEET) is a widely recommended ingredient in topical repellents. Picaridin and oil of lemon eucalyptus are also used and have been shown to be effective and safe.
How do other products work?
“Physical” insect-repelling products, such as wristbands, coils and candles, often contain a botanically derived chemical and are often marketed as being an alternative to DEET.
However, studies have shown that devices such as candles containing citronella oil provide lower mosquito-bite prevention than topical repellents.
A laboratory study in 2011 found wristbands infused with peppermint oil failed to provide full protection from mosquito bites.
Even as topical repellent formulations applied to the skin, these botanically derived products have lower mosquito bite protection than recommended products such as those containing DEET, picaridin and oil of lemon eucalyptus.
Wristbands infused with DEET have shown mixed results but may provide some bite protection or bite reduction. DEET-based wristbands or patches are not currently available in Australia.
There is also a range of mosquito repellent coils, sticks, and other devices that release insecticides (for example, pyrethroids). These chemicals are primarily designed to kill or “knock down” mosquitoes rather than to simply keep them from biting us.
What about stickers and patches?
Although insect repellent patches and stickers have been available for many years, there has been a sudden surge in their marketing through social media. But there are very few scientific studies testing their efficacy.
Our current understanding of the way insect repellents work would suggest these small stickers and patches offer little protection from mosquito bites.
At best, they may reduce some bites in the way mosquito coils containing botanical products work. However, the passive release of chemicals from the patches and stickers is likely to be substantially lower than those from mosquito coils and other devices actively releasing chemicals.
One study in 2013 found a sticker infused with oil of lemon eucalyptus “did not provide significant protection to volunteers”.
Clothing impregnated with insecticides, such as permethrin, will assist in reducing mosquito bites but topical insect repellents are still recommended for exposed areas of skin.
Take care when using these products
The idea you can apply a sticker or patch to your clothing to protect you from mosquito bites may sound appealing, but these devices provide a false sense of security. There is no evidence they are an equally effective alternative to the topical repellents recommended by health authorities around the world. It only takes one bite from a mosquito to transmit the pathogens that result in serious disease.
It is also worth noting that there are some health warnings and recommendations for their use required by Australian Pesticides and Veterinary Medicines Authority. Some of these products warn against application to the skin (recommending application to clothing only) and to keep products “out of reach of children”. This is a challenge if attached to young children’s clothing.
Similar warnings are associated with most other topical and non-topical mosquito repellents. Always check the labels of these products for safe use recommendations.
Are there any other practical alternatives?
Topical insect repellents are safe and effective. Most can be used on children from 12 months of age and pose no health risks. Make sure you apply the repellent as a thin even coat on all exposed areas of skin.
But you don’t need “tropical strength” repellents for short periods of time outdoors; a range of formulations with lower concentrations of repellent will work well for shorter trips outdoors. There are some repellents that don’t smell as strong (for example, children’s formulations, odourless formulations) or formulations that may be more pleasant to use (for example, pump pack sprays).
Finally, you can always cover up. Loose-fitting long-sleeved shirts, long pants, and covered shoes will provide a physical barrier between you and mosquitoes on the hunt for your or your family’s blood this summer.
Cameron Webb, Clinical Associate Professor and Principal Hospital Scientist, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: