Does intermittent fasting increase or decrease our risk of cancer?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Research over the years has suggested intermittent fasting has the potential to improve our health and reduce the likelihood of developing cancer.
So what should we make of a new study in mice suggesting fasting increases the risk of cancer?

What is intermittent fasting?
Intermittent fasting means switching between times of eating and not eating. Unlike traditional diets that focus on what to eat, this approach focuses on when to eat.
There are lots of commonly used intermittent fasting schedules. The 16/8 plan means you only eat within an eight-hour window, then fast for the remaining 16 hours. Another popular option is the 5:2 diet, where you eat normally for five days then restrict calories for two days.
In Australia, poor diet contributes to 7% of all cases of disease, including coronary heart disease, stroke, type 2 diabetes, and cancers of the bowel and lung. Globally, poor diet is linked to 22% of deaths in adults over the age of 25.
Intermittent fasting has gained a lot of attention in recent years for its potential health benefits. Fasting influences metabolism, which is how your body processes food and energy. It can affect how the body absorbs nutrients from food and burns energy from sugar and fat.
What did the new study find?
The new study, published in Nature, found when mice ate again after fasting, their gut stem cells, which help repair the intestine, became more active. The stem cells were better at regenerating compared with those of mice who were either totally fasting or eating normally.
This suggests the body might be better at healing itself when eating after fasting.
However, this could also have a downside. If there are genetic mutations present, the burst of stem cell-driven regeneration after eating again might make it easier for cancer to develop.
Polyamines – small molecules important for cell growth – drive this regeneration after refeeding. These polyamines can be produced by the body, influenced by diet, or come from gut bacteria.
The findings suggest that while fasting and refeeding can improve stem cell function and regeneration, there might be a tradeoff with an increased risk of cancer, especially if fasting and refeeding cycles are repeated over time.
While this has been shown in mice, the link between intermittent fasting and cancer risk in humans is more complicated and not yet fully understood.
What has other research found?
Studies in animals have found intermittent fasting can help with weight loss, improve blood pressure and blood sugar levels, and subsequently reduce the risks of diabetes and heart disease.
Research in humans suggests intermittent fasting can reduce body weight, improve metabolic health, reduce inflammation, and enhance cellular repair processes, which remove damaged cells that could potentially turn cancerous.
However, other studies warn that the benefits of intermittent fasting are the same as what can be achieved through calorie restriction, and that there isn’t enough evidence to confirm it reduces cancer risk in humans.
What about in people with cancer?
In studies of people who have cancer, fasting has been reported to protect against the side effects of chemotherapy and improve the effectiveness of cancer treatments, while decreasing damage to healthy cells.
Prolonged fasting in some patients who have cancer has been shown to be safe and may potentially be able to decrease tumour growth.
On the other hand, some experts advise caution. Studies in mice show intermittent fasting could weaken the immune system and make the body less able to fight infection, potentially leading to worse health outcomes in people who are unwell. However, there is currently no evidence that fasting increases the risk of bacterial infections in humans.
So is it OK to try intermittent fasting?
The current view on intermittent fasting is that it can be beneficial, but experts agree more research is needed. Short-term benefits such as weight loss and better overall health are well supported. But we don’t fully understand the long-term effects, especially when it comes to cancer risk and other immune-related issues.
Since there are many different methods of intermittent fasting and people react to them differently, it’s hard to give advice that works for everyone. And because most people who participated in the studies were overweight, or had diabetes or other health problems, we don’t know how the results apply to the broader population.
For healthy people, intermittent fasting is generally considered safe. But it’s not suitable for everyone, particularly those with certain medical conditions, pregnant or breastfeeding women, and people with a history of eating disorders. So consult your health-care provider before starting any fasting program.
Amali Cooray, PhD Candidate in Genetic Engineering and Cancer, WEHI (Walter and Eliza Hall Institute of Medical Research)
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Best Salt for Neti Pots?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
❓ Q&A With 10almonds Subscribers!
Q: What kind of salt is best for neti pots?
A: Non-iodised salt is usually recommended, but really, any human-safe salt is fine. By this we mean for example:
- Sodium chloride (like most kitchen salts),
- Potassium chloride (as found in “reduced sodium” kitchen salts), or
- Magnesium sulfate (also known as epsom salts).
Share This Post
-
How Are You, Really?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Are You, Really? The Free NHS Health Test
We took this surprisingly incisive 10-minute test from the UK’s famous National Health Service—the test is part of the “Better Health” programme, a free-to-all (yes, even those from/in other countries) initiative aimed at keeping people healthy enough to have less need of medical attention.
As one person who took the test wrote:
❝I didn’t expect that a government initiative would have me talking about how I need to keep myself going to be there for the people I love, let alone that a rapid-pace multiple-choice test would elicit these responses and give personalized replies in turn, but here we are❞
It goes beyond covering the usual bases, in that it also looks at what’s most important to you, and why, and what might keep you from doing the things you want/need to do for your health, AND how those obstacles can be overcome.
Pretty impressive for a 10-minute test!
Is Your Health Above Average Already? Take the Free 10-minute NHS test now!
How old are you, in your heart?
Poetic answers notwithstanding (this writer sometimes feels so old, and yet also much younger than she is), there’s a biological answer here, too.
Again free for the use of all*, here’s a heart age calculator.
*It is suitable for you if you are aged 30–95, and do not have a known complicating cardiovascular disease.
It will ask you your (UK) postcode; just leave that field blank if you’re not in the UK; it’ll be fine.
How Old Are You, In Your Heart? Take the Free 10-minute NHS test now!
(Neither test requires logging into anything, and they do not ask for your email address. The tests are right there on the page, and they give the answers right there on the page, immediately)
Share This Post
-
What is a virtual emergency department? And when should you ‘visit’ one?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For many Australians the emergency department (ED) is the physical and emblematic front door to accessing urgent health-care services.
But health-care services are evolving rapidly to meet the population’s changing needs. In recent years, we’ve seen growing use of telephone, video, and online health services, including the national healthdirect helpline, 13YARN (a crisis support service for First Nations people), state-funded lines like 13 HEALTH, and bulk-billed telehealth services, which have helped millions of Australians to access health care on demand and from home.
The ED is similarly expanding into new telehealth models to improve access to emergency medical care. Virtual EDs allow people to access the expertise of a hospital ED through their phone, computer or tablet.
All Australian states and the Northern Territory have some form of virtual ED at least in development, although not all of these services are available to the general public at this stage.
So what is a virtual ED, and when is it appropriate to consider using one?
Shutterstock/Nils Versemann How does a virtual ED work?
A virtual ED is set up to mirror the way you would enter the physical ED front door. First you provide some basic information to administration staff, then you are triaged by a nurse (this means they categorise the level of urgency of your case), then you see the ED doctor. Generally, this all takes place in a single video call.
In some instances, virtual ED clinicians may consult with other specialists such as neurologists, cardiologists or trauma experts to make clinical decisions.
A virtual ED is not suitable for managing medical emergencies which would require immediate resuscitation, or potentially serious chest pains, difficulty breathing or severe injuries.
A virtual ED is best suited to conditions that require immediate attention but are not life-threatening. These could include wounds, sprains, respiratory illnesses, allergic reactions, rashes, bites, pain, infections, minor burns, children with fevers, gastroenteritis, vertigo, high blood pressure, and many more.
People with these sorts of conditions and concerns may not be able to get in to see a GP straight away and may feel they need emergency advice, care or treatment.
When attending the ED, they can be subject to long wait times and delayed specialist attention because more serious cases are naturally prioritised. Attending a virtual ED may mean they’re seen by a doctor more quickly, and can begin any relevant treatment sooner.
From the perspective of the health-care system, virtual EDs are about redirecting unnecessary presentations away from physical EDs, helping them be ready to respond to emergencies. The virtual ED will not hesitate in directing callers to come into the physical ED if staff believe it is an emergency.
The doctor in the virtual ED may also direct the patient to a GP or other health professional, for example if their condition can’t be assessed visually, or if they need physical treatment.
The results so far
Virtual EDs have developed significantly over the past three years, predominantly driven by the COVID pandemic. We are now starting to slowly see assessments of these services.
A recent evaluation my colleagues and I did of Queensland’s Metro North Virtual ED found roughly 30% of calls were directed to the physical ED. This suggests 70% of the time, cases could be managed effectively by the virtual ED.
Preliminary data from a Victorian virtual ED indicates it curbed a similar rate of avoidable ED presentations – 72% of patients were successfully managed by the virtual ED alone. A study on the cost-effectiveness of another Victorian virtual ED suggested it has the potential to generate savings in health-care costs if it prevents physical ED visits.
Only 1.2% of people assessed in Queensland’s Metro North Virtual ED required unexpected hospital admission within 48 hours of being “discharged” from the virtual ED. None of these cases were life-threatening. This indicates the virtual ED is very safe.
The service experienced an average growth rate of 65% each month over a two-year evaluation period, highlighting increasing demand and confidence in the service. Surveys suggested clinicians also view the virtual ED positively.
The right advice could tell you whether you need to visit hospital in person or not. 1st footage/Shutterstock What now?
We need further research into patient outcomes and satisfaction, as well as the demographics of those using virtual EDs, and how these measures compare to the physical ED across different triage categories.
There are also challenges associated with virtual EDs, including around technology (connection and skills among patients and health professionals), training (for health professionals) and the importance of maintaining security and privacy.
Nonetheless, these services have the potential to reduce congestion in physical EDs, and offer greater convenience for patients.
Eligibility differs between different programs, so if you want to use a virtual ED, you may need to check you are eligible in your jurisdiction. Most virtual EDs can be accessed online, and some have direct phone numbers.
Jaimon Kelly, Senior Research Fellow in Telehealth delivered health services, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
What Flexible Dieting Really Means
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Flexibility Is The Dish Of The Day
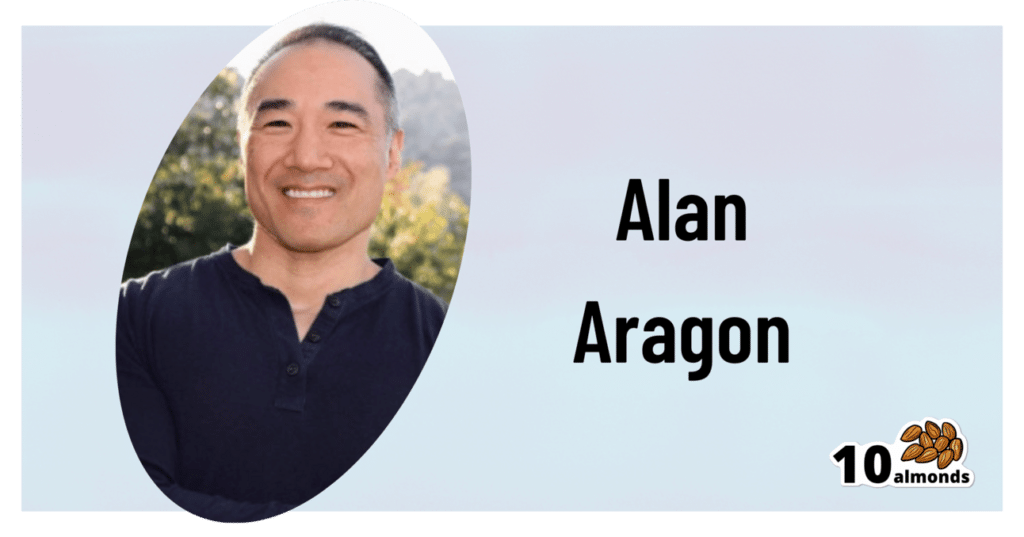
This is Alan Aragon. Notwithstanding not being a “Dr. Alan Aragon”, he’s a research scientist with dozens of peer-reviewed nutrition science papers to his name, as well as being a personal trainer and fitness educator. Most importantly, he’s an ardent champion of making people’s pursuit of health and fitness more evidence-based.
We’ll be sharing some insights from a book of his that we haven’t reviewed yet, but we will link it at the bottom of today’s article in any case.
What does he want us to know?
First, get out of the 80s and into the 90s
In the world of popular dieting, the 80s were all about calorie-counting and low-fat diets. They did not particularly help.
In the 90s, it was discovered that not only was low-fat not the way to go, but also, regardless of the diet in question, rigid dieting leads to “disinhibition”, that is to say, there comes a point (usually not far into a diet) whereby one breaks the diet, at which point, the floodgates open and the dieter binges unhealthily.
Aragon would like to bring our attention to a number of studies that found this in various ways over the course of the 90s measuring various different metrics including rigid vs flexible dieting’s impacts on BMI, weight gain, weight loss, lean muscle mass changes, binge-eating, anxiety, depression, and so forth), but we only have so much room here, so here’s a 1999 study that’s pretty much the culmination of those:
Flexible vs. Rigid Dieting Strategies: Relationship with Adverse Behavioral Outcomes
So in short: trying to be very puritan about any aspect of dieting will not only not work, it will backfire.
Next, get out of the 90s into the 00s
…which is not only fun if you read “00s” out loud as “naughties”, but also actually appropriate in this case, because it is indeed important to be comfortable being a little bit naughty:
In 2000, Dr. Marika Tiggemann found that dichotomous perceptions of food (e.g. good/bad, clean/dirty, etc) were implicated as a dysfunctional cognitive style, and predicted not only eating disorders and mood disorders, but also adverse physical health outcomes:
Dieting and Cognitive Style: The Role of Current and Past Dieting Behaviour and Cognitions
This was rendered clearer, in terms of physical health outcomes, by Dr. Susan Byrne & Dr. Emma Dove, in 2009:
❝Weight loss was negatively associated with pre-treatment depression and frequency of treatment attendance, but not with dichotomous thinking. Females who regard their weight as unacceptably high and who think dichotomously may experience high levels of depression irrespective of their actual weight, while depression may be proportionate to the degree of obesity among those who do not think dichotomously❞
Aragon’s advice based on all this: while yes, some foods are better than others, it’s more useful to see foods as being part of a spectrum, rather than being absolutist or “black and white” about it.
Next: hit those perfect 10s… Imperfectly
The next decade expanded on this research, as science is wont to do, and for this one, Aragon shines a spotlight on Dr. Alice Berg’s 2018 study with obese women averaging 69 years of age, in which…
In other words (and in fact, to borrow Dr. Berg’s words from that paper),
❝encouraging a flexible approach to eating behavior and discouraging rigid adherence to a diet may lead to better intentional weight loss for overweight and obese older women❞
You may be wondering: what did this add to the studies from the 90s?
And the key here is: rather than being observational, this was interventional. In other words, rather than simply observing what happened to people who thought one way or another, this study took people who had a rigid, dichotomous approach to food, and gave them a 6-month behavioral intervention (in other words, support encouraging them to be more flexible and open in their approach to food), and found that this indeed improved matters for them.
Which means, it’s not a matter of fate or predisposition, as it could have been back in the 90s, per “some people are just like that; who’s to say which factor causes which”. Instead, now we know that this is an approach that can be adopted, and it can be expected to work.
Beyond weight loss
Now, so far we’ve talked mostly about weight loss, and only touched on other health outcomes. This is because:
- weight loss a very common goal for many
- it’s easy to measure so there’s a lot of science for it
Incidentally, if it’s a goal of yours, here’s what 10almonds had to say about that, along with two follow-up articles for other related goals:
Spoiler: we agree with Aragon, and recommend a relaxed and flexible approach to all three of these things
Aragon’s evidence-based approach to nutrition has found that this holds true for other aspects of healthy eating, too. For example…
To count or not to count?
It’s hard to do evidence-based anything without counting, and so Aragon talks a lot about this. Indeed, he does a lot of counting in scientific papers of his own, such as:
and
The effect of protein timing on muscle strength and hypertrophy: a meta-analysis
…as well as non-protein-related but diet-related topics such as:
But! For the at-home health enthusiast, Aragon recommends that the answer to the question “to count or not to count?” is “both”:
- Start off by indeed counting and tracking everything that is important to you (per whatever your current personal health intervention is, so it might be about calories, or grams of protein, or grams of carbs, or a certain fat balance, or something else entirely)
- Switch to a more relaxed counting approach once you get used to the above. By now you probably know the macros for a lot of your common meals, snacks, etc, and can tally them in your head without worrying about weighing portions and knowing the exact figures.
- Alternatively, count moderately standardized portions of relevant foods, such as “three servings of beans or legumes per day” or “no more than one portion of refined carbohydrates per day”
- Eventually, let habit take the wheel. Assuming you have established good dietary habits, this will now do you just fine.
This latter is the point whereby the advice (that Aragon also champions) of “allow yourself an unhealthy indulgence of 10–20% of your daily food”, as a budget of “discretionary calories”, eventually becomes redundant—because chances are, you’re no longer craving that donut, and at a certain point, eating foods far outside the range of healthiness you usually eat is not even something that you would feel inclined to do if offered.
But until that kicks in, allow yourself that budget of whatever unhealthy thing you enjoy, and (this next part is important…) do enjoy it.
Because it is no good whatsoever eating that cream-filled chocolate croissant and then feeling guilty about it; that’s the dichotomous thinking we had back in the 80s. Decide in advance you’re going to eat and enjoy it, then eat and enjoy it, then look back on it with a sense of “that was enjoyable” and move on.
The flipside of this is that the importance of allowing oneself a “little treat” is that doing so actively helps ensure that the “little treat” remains “little”. Without giving oneself permission, then suddenly, “well, since I broke my diet, I might as well throw the whole thing out the window and try again on Monday”.
On enjoying food fully, by the way:
Mindful Eating: How To Get More Nutrition Out Of The Same Food
Want to know more from Alan Aragon?
Today we’ve been working heavily from this book of his; we haven’t reviewed it yet, but we do recommend checking it out:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Childhood Vaccination Rates, a Rare Health Bright Spot in Struggling States, Are Slipping
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Jen Fisher can do only so much to keep her son safe from the types of infections that children can encounter at school. The rest, she said, is up to other students and parents in their hometown of Franklin, Tennessee.
Fisher’s son Raleigh, 12, lives with a congenital heart condition, which has left him with a weakened immune system. For his protection, Raleigh has received all the recommended vaccines for a child his age. But even with his vaccinations, a virus that might only sideline another child could sicken him and land him in the emergency room, Fisher said.
“We want everyone to be vaccinated so that illnesses like measles and things that have basically been eradicated don’t come back,” Fisher said. “Those can certainly have a very adverse effect on Raleigh.”
For much of Raleigh’s life, Fisher could take comfort in the high childhood vaccination rate in Tennessee — a public health bright spot in a conservative state with poor health outcomes and one of the shortest life expectancies in the nation.
Mississippi and West Virginia, two similarly conservative states with poor health outcomes and short life expectancies, also have some of the highest vaccination rates for kindergartners in the nation — a seeming contradiction that stems from the fact that childhood vaccination requirements don’t always align with states’ other characteristics, said James Colgrove, a Columbia University professor who studies factors that influence public health.
“The kinds of policies that states have don’t map neatly on to ‘red’ versus ‘blue’ or one region or another,” Colgrove said.
Advocates, doctors, public health officials, and researchers worry such public health bright spots in some states are fading: Many states have recently reported an increase in people opting out of vaccines for their kids as Americans’ views shift.
During the 2023-24 school year, the percentage of kindergartners exempted from one or more vaccinations rose to 3.3%, the highest ever reported, with increases in 40 states and Washington, D.C., according to Centers for Disease Control and Prevention data. Tennessee and Mississippi were among those with increases. Nearly all exemptions nationally were for nonmedical reasons.
Vaccine proponents worry anti-vaccine messaging could accelerate a growing “health freedom” movement that has been pushed by leaders in states such as Florida. Momentum against vaccines is likely to continue to grow with the election of Donald Trump as president and his proposed nomination of anti-vaccine activist Robert F. Kennedy Jr. as secretary of the Department of Health and Human Services.
Pediatricians in states with high exemption rates, such as Florida and Georgia, say they’re concerned by what they see — declining immunization levels for kindergartners, which could lead to a resurgence in vaccine-preventable diseases such as measles. The Florida Department of Health reported nonmedical exemption rates as high as 50% for children in some areas.
“The religious exemption is huge,” said Brandon Chatani, a pediatric infectious disease doctor in Orlando. “That has allowed for an easy way for these kids to enter schools without vaccines.”
In many states, it’s easier to get a religious exemption than a medical one, which often requires signoff from a doctor.
Over the past decade, California, Connecticut, Maine, and New York have removed religious and philosophical exemptions from school vaccination requirements. West Virginia has not had them.
Idaho, Alaska, and Utah had the highest exemption rates for the 2023-24 school year, according to the CDC. Those states allow parents or legal guardians to exempt their children for religious reasons by submitting a notarized form or a signed statement.
Florida and Georgia, with some of the lowest reported minimum vaccination rates for kindergartners, allow parents to exempt their children by submitting a form with the child’s school or day care.
Both states have reported declines in uptake of the measles, mumps, and rubella vaccine, which is one of the most common childhood shots. In Georgia, MMR coverage for kindergartners dropped to 88.4% in the 2023-24 school year from 93.1% in 2019-20, according to the CDC. Florida dropped to 88.1% from 93.5% during the same period.
Andi Shane, a pediatric infectious disease specialist in Atlanta, traces Georgia’s declining rates to families who lack access to a pediatrician. State policies on exemptions are also key, she said.
“There’s lots of data to support the fact that when personal belief exemptions are not permitted, that vaccination rates are higher,” she said.
In December, Georgia public health officials put out an advisory saying the state had recorded significantly more whooping cough cases than in the prior year. According to CDC data, Georgia reported 280 cases in 2024 compared with 96 the year before.
Until 2023, Mississippi was one of the few states that allowed parents to opt out of vaccinating their kids only for medical reasons — and only with the approval of a doctor. That gave it among the highest vaccination rates in the nation as of the 2023-24 school year.
“It’s one of the few things Mississippi has done well,” said Anita Henderson, a pediatrician who has practiced in the southern part of the state for nearly 30 years. In terms of health, she said, childhood vaccination rates were the state’s one “shining star.”
But that changed in April 2023 when a federal judge ordered state officials to start allowing religious exemptions. The ruling has emboldened many families, Henderson said.
“We are seeing more and more skepticism, more and more vaccine hesitancy, and a lack of confidence because of this ruling,” she said.
State officials have granted more than 5,000 religious exemptions since the court order allowing them, according to the state health department. Daniel Edney, the state health officer, said most of the requests have come from “more affluent” residents in “pockets” of the state.
“Most people listen to the expert opinions of their pediatricians and family medicine doctors to stay on the vaccine schedule, because it’s what is best to protect their children,” he said.
West Virginia’s vaccine law — which hasn’t allowed nonmedical exemptions — also could soon change, Matthew Christiansen said in December before he resigned as the state’s health officer.
A bill that would have broadened exemptions made it through the legislature last year but was vetoed by outgoing Republican Gov. Jim Justice. The new governor, Republican Pat Morrisey, has been a vocal critic of vaccine mandates. And just a day after being inaugurated, he issued an executive order to propose provisions by Feb. 1 that could allow religious and conscientious exemptions.
“I want to send a message that if you have a religious belief, then we’re going to have an exception,” he said at a Jan. 14 press conference. “We’re not going to be the outlier.”
People asserting their personal freedoms to decline vaccines for their kids can ultimately curtail the ability of others to live full lives, Christiansen said. “Kids getting measles and mumps and polio and being paralyzed for their whole life is an impediment on personal freedom and autonomy for those kids,” he said.
Since the covid pandemic, anti-vaccine sentiment has been growing in Tennessee. One organization, Stand for Health Freedom, drafted a letter for constituents to send to their state lawmakers calling for the resignation of the medical director of Tennessee’s Vaccine-Preventable Diseases and Immunization Program. The group said she demonstrated a “lack of respect for the informed consent rights” of the people.
“They feel emboldened by the idea that this presidential administration seems to feel very strongly that a lot of these issues should be taken back to the states,” said Emily Delikat, director of Tennessee Families for Vaccines, a pro-vaccine group.
Ultimately, like many effective public health interventions, vaccines are a victim of their own success, said Henderson, the Mississippi pediatrician. Most people haven’t seen outbreaks of measles or polio, so they forget how dangerous the diseases are, she said.
“It may unfortunately take a resurgence of those diseases to raise awareness to the fact that these are dangerous, these are deadly, these are preventable,” she said. “I hope it doesn’t come to that.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Move – by Caroline Williams
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
- Get 150 minutes of moderate exercise per week, says the American Heart Association
- There are over 10,000 minutes per week, says the pocket calculator
Is 150/10,000 really the goal here? Really?
For Caroline Williams, the answer is no.
In this book that’s practically a manifesto, she outlines the case that:
- Humans evolved to move
- Industrialization and capitalism scuppered that
- We now spend far too long each day without movement
Furthermore, for Williams this isn’t just an anthropological observation, it’s a problem to be solved, because:
- Our lack of movement is crippling us—literally
- Our stagnation affects not just our bodies, but also our minds
- (again literally—there’s a direct correlation with mental health)
- We urgently need to fix this
So, what now, do we need to move in to the gym and become full-time athletes to clock up enough hours of movement? No.
Williams convincingly argues the case (using data from supercentenarian “blue zones” around the world) that even non-exertive movement is sufficient. In other words, you don’t have to be running; walking is great. You don’t have to be lifting weights; doing the housework or gardening will suffice.
From that foundational axiom, she calls on us to find ways to build our life around movement… rather than production-efficiency and/or convenience. She gives plenty of tips for such too!
Bottom line: some books are “I couldn’t put it down!” books. This one’s more of a “I got the urge to get up and get moving!” book.
Get your get-up-and-go up and going with “Move”—order yours from Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: