Do you have knee pain from osteoarthritis? You might not need surgery. Here’s what to try instead
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most people with knee osteoarthritis can control their pain and improve their mobility without surgery, according to updated treatment guidelines from the Australian Commission on Safety and Quality in Health Care.
So what is knee osteoarthritis and what are the best ways to manage it?

More than 2 million Australians have osteoarthritis
Osteoarthritis is the most common joint disease, affecting 2.1 million Australians. It costs the economy A$4.3 billion each year.
Osteoarthritis commonly affects the knees, but can also affect the hips, spine, hands and feet. It impacts the whole joint including bone, cartilage, ligaments and muscles.
Most people with osteoarthritis have persistent pain and find it difficult to perform simple daily tasks, such as walking and climbing stairs.
Is it caused by ‘wear and tear’?
Knee osteoarthritis is most likely to affect older people, those who are overweight or obese, and those with previous knee injuries. But contrary to popular belief, knee osteoarthritis is not caused by “wear and tear”.
Research shows the degree of structural wear and tear visible in the knee joint on an X-ray does not correlate with the level of pain or disability a person experiences. Some people have a low degree of structural wear and tear and very bad symptoms, while others have a high degree of structural wear and tear and minimal symptoms. So X-rays are not required to diagnose knee osteoarthritis or guide treatment decisions.
Telling people they have wear and tear can make them worried about their condition and afraid of damaging their joint. It can also encourage them to try invasive and potentially unnecessary treatments such as surgery. We have shown this in people with osteoarthritis, and other common pain conditions such as back and shoulder pain.
This has led to a global call for a change in the way we think and communicate about osteoarthritis.
What’s the best way to manage osteoarthritis?
Non-surgical treatments work well for most people with osteoarthritis, regardless of their age or the severity of their symptoms. These include education and self-management, exercise and physical activity, weight management and nutrition, and certain pain medicines.
Education is important to dispel misconceptions about knee osteoarthritis. This includes information about what osteoarthritis is, how it is diagnosed, its prognosis, and the most effective ways to self-manage symptoms.
Health professionals who use positive and reassuring language can improve people’s knowledge and beliefs about osteoarthritis and its management.
Many people believe that exercise and physical activity will cause further damage to their joint. But it’s safe and can reduce pain and disability. Exercise has fewer side effects than commonly used pain medicines such as paracetamol and anti-inflammatories and can prevent or delay the need for joint replacement surgery in the future.
Many types of exercise are effective for knee osteoarthritis, such as strength training, aerobic exercises like walking or cycling, Yoga and Tai chi. So you can do whatever type of exercise best suits you.
Increasing general physical activity is also important, such as taking more steps throughout the day and reducing sedentary time.
Weight management is important for those who are overweight or obese. Weight loss can reduce knee pain and disability, particularly when combined with exercise. Losing as little as 5–10% of your body weight can be beneficial.
Pain medicines should not replace treatments such as exercise and weight management but can be used alongside these treatments to help manage pain. Recommended medicines include paracetamol and non-steroidal anti-inflammatory drugs.
Opioids are not recommended. The risk of harm outweighs any potential benefits.
What about surgery?
People with knee osteoarthritis commonly undergo two types of surgery: knee arthroscopy and knee replacement.
Knee arthroscopy is a type of keyhole surgery used to remove or repair damaged pieces of bone or cartilage that are thought to cause pain.
However, high-quality research has shown arthroscopy is not effective. Arthroscopy should therefore not be used in the management of knee osteoarthritis.
Joint replacement involves replacing the joint surfaces with artificial parts. In 2021–22, 53,500 Australians had a knee replacement for their osteoarthritis.
Joint replacement is often seen as being inevitable and “necessary”. But most people can effectively manage their symptoms through exercise, physical activity and weight management.
The new guidelines (known as “care standard”) recommend joint replacement surgery only be considered for those with severe symptoms who have already tried non-surgical treatments.
I have knee osteoarthritis. What should I do?
The care standard links to free evidence-based resources to support people with osteoarthritis. These include:
- education, such as a decision aid and four-week online course
- self-directed online exercise and yoga programs
- weight management support
- pain management strategies, such as MyJointPain and painTRAINER.
If you have osteoarthritis, you can use the care standard to inform discussions with your health-care provider, and to make informed decisions about your care.
Belinda Lawford, Postdoctoral research fellow in physiotherapy, The University of Melbourne; Giovanni E. Ferreira, NHMRC Emerging Leader Research Fellow, Institute of Musculoskeletal Health, University of Sydney; Joshua Zadro, NHMRC Emerging Leader Research Fellow, Sydney Musculoskeletal Health, University of Sydney, and Rana Hinman, Professor in Physiotherapy, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eye Exercises That Measurably Improve Your Vision
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our eyesight, like most of the rest of our body’s functions, will decline if not adequately maintained. Modern lifestyles see most of us indoors for most of the day (which means a reduced maximum focal length) and often looking at screens (even further reduced focal length), which means that part of our eyes responsible for focus will tend to atrophy and wither. And if we want to see something better, we adjust the settings instead of adjusting our eyes. However, it is perfectly possible to recover our clear youthful vision:
See the results for yourself (and see them clearly!)
The exercises that gave him the results he showed between the two tests, are:
- Blink for 30 seconds
- Focus on something in front and (keeping your focus on that stationary point) move your head left & right, upwards & downwards, and diagonally
- Take a break and blink for 30 seconds
- Keep your head still while you move your eyes left & right, upwards & downwards, and diagonally
- Focus on something in front while you move move your head left & right, upwards & downwards, and diagonally
This should temporarily improve your vision immediately, because of what has been going on in the capillaries in and around your eyes, but sustained results require sustained (i.e. daily) practice. This is because the vasculature is only part of the mechanism; it’s also a matter of improving the muscles responsible for focusing the eyes—and like any muscles, it’s not a case of “do it once and enjoy the results forever”. So, even just 2–3 minutes each day is recommended.
For more on all of this plus a visual demonstration, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Are Your Glasses Making Your Eyesight Worse?
or, if you are very serious about having excellent vision for life:
Vision for Life, Revised Edition – by Dr. Meir Schneider ← this one’s a book, and a very good one at that
Take care!
Share This Post
-
Mango vs Papaya – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mango to papaya, we picked the mango.
Why?
Both are great! But there are some things to set them apart:
In terms of macros, this one’s not so big of a difference. They are equal in fiber, while mango has more protein and slightly more carbs. They are both low glycemic index, so we’ll call this one a tie, or the slenderest nominal win for papaya.
When it comes to vitamins, mango has more of vitamins A, B1, B3, B5, B7, B9, E, K, and choline, while papaya has more vitamin C. However, a cup of mango already gives the RDA of vitamin C, so at this point, it’s not even really much of a bonus that papaya has more. In any case, a clear and overwhelming win in the vitamins category for mango.
As for minerals, this one’s closer; mango has more copper, manganese, phosphorus, and zinc, while papaya has more calcium, iron, and magnesium. Still, a 4:3 win for mango.
Adding these up makes for a clear win for mango. However, one extra thing to bear in mind about both:
Both of these fruits interact with warfarin and many other anticoagulants. So if you’re taking those, you might want to skip these, or at least consult with your doctor/pharmacist for input on your personal situation.
Aside from that; enjoy both; diversity is good! But mango is the more nutritionally dense, and thus the winner here.
Want to learn more?
You might like to read:
5 Ways To Make Your Smoothie Blood Sugar Friendly (Avoid the Spike!)
Take care!
Share This Post
-
Sesame Oil vs Almond Oil – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sesame oil to almond oil, we picked the almond.
Why?
We were curious about this one! Were you, or were you confident? You see, almonds tend to blow away all the other nuts with their nutritional density, but they’re far from the oiliest of nuts, and their greatest strengths include their big dose of protein and fiber (which don’t make it into the oil), vitamins (most of which don’t make it into the oil) and minerals (which don’t make it into the oil). So, a lot will come down to the fat profile!
On which note, looking at the macros first, it’s 100% fat in both cases, but sesame oil has more saturated fat and polyunsaturated fat, while almond oil has more monounsaturated fat. Since the mono- and poly-unsaturated fats are both healthy and each oil has more of one or the other, the deciding factor here is which has the least saturated fat—and that’s the almond oil, which has close to half the saturated fat of sesame oil. As an aside, neither of them are a source of omega-3 fatty acids.
In terms of vitamins, there’s not a lot to say here, but “not a lot” is not nothing: sesame oil has nearly 2x the vitamin K, while almond oil has 28x the vitamin E*, and 2x the choline. So, another win for almond oil.
*which is worth noting, not least of all because seeds are more widely associated with vitamin E in popular culture, but it’s the almond oil that provide much more here. Not to get too distracted into looking at the values of the actual seeds and nuts, almonds themselves do have over 102x the vitamin E compared to sesame seeds.
Now, back to the oils:
In the category of minerals, there actually is nothing to say here, except you can’t get more than the barest trace of any mineral from either of these two oils. So it’s a tie on this one.
Adding up the categories makes for a clear win for almond oil!
Want to learn more?
You might like to read:
Avocado Oil vs Olive Oil – Which is Healthier?
Take care!
Share This Post
Related Posts
-
How To Keep Your Mind From Wandering
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whether your mind keeps wandering more as you get older, or you’re a young student whose super-active brain is more suited to TikTok than your assigned reading, sustained singular focus can be a challenge for everyone—and yet (alas!) it remains a required skill for so much in life.
Today’s edition of 10Almonds presents a nifty trick to get yourself through those tasks! We’ll also be taking some time to reply to your questions and comments, in our weekly interactive Q&A.
First of all though, we’ve a promise to make good on, so…
How To Stay On The Ball (Or The Tomato?) The Easy Way
For most of us, we face three main problems when it comes to tackling our to-dos:
- Where to start?
- The task seems intimidating in its size
- We get distracted and/or run out of energy
If you’re really not sure where to start, we recommended a powerful tool in last Friday’s newsletter!
For the rest, we love the Pomodoro Technique:
- Set a timer for 25 minutes, and begin your task.
- Keep going until the timer is done! No other tasks, just focus.
- Take a 5-minute break.
- Repeat
This approach has three clear benefits:
- No matter the size of the task, you are only committing to 25 minutes—everything is much less overwhelming when there’s an end in sight!
- Being only 25 minutes means we are much more likely to stay on track; it’s easier to defer other activities if we know that there will be a 5-minute break for that soon.
- Even without other tasks to distract us, it can be difficult to sustain attention for long periods; making it only 25 minutes at a time allows us to approach it with a (relatively!) fresh mind.
Have you heard that a human brain can sustain attention for only about 40 minutes before focus starts to decline rapidly?
While that’s been a popular rationale for school classroom lesson durations (and perhaps coincidentally ties in with Zoom’s 40-minute limit for free meetings), the truth is that focus starts dropping immediately, to the point that one-minute attention tests are considered sufficient to measure the ability to focus.
So a 25-minute Pomodoro is a more than fair compromise!
Why’s it called the “Pomodoro” technique?
And why is the 25-minute timed work period called a Pomodoro?
It’s because back in the 80s, university student Francesco Cirillo was struggling to focus and made a deal with himself to focus just for a short burst at a time—and he used a (now “retro” style) kitchen timer in the shape of a tomato, or “pomodoro”, in Italian.
If you don’t have a penchant for kitsch kitchenware, you can use this free, simple Online Pomodoro Timer!
(no registration/login/download necessary; it’s all right there on the web page)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Wrong Arm Position = Wrong Measurement Of Blood Pressure
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is especially important to know if you measure your own blood pressure at home.
Even if you don’t, it’s still good to know this as healthcare providers also can (and often will) do it wrong, especially if they are under time pressure (e.g. they need to get you out of their office and the next person in):
From the heart
Many things can change our blood pressure, and even gravity changes (considerably!) our blood pressure locally.
For example, even with good circulation, so long as we are in the Earth’s gravity under normal conditions (e.g. not skydiving, not riding a rollercoaster, etc), our blood pressure will always be higher below our heart, and lower above it, because gravity is pulling our blood downwards; this is also why if your circulation is not good, you may feel light-headed upon sitting up or standing up, as the bloodstream takes a moment to win a battle against gravity. This is also why blood rushes to your head if you are hanging upside down—increasing the local blood pressure in your head, which unlike your feet, isn’t used to it, so you feel it, and the effect may be visible from the outside, too.
When it comes to having your arm above or below your heart, the difference is less pronounced as it’s only a small change, but that small change can make a big difference:
- If the cuff is above heart level → Lower blood pressure reading.
- If the cuff is below heart level → Higher blood pressure reading.
- Every 1-inch difference causes a 2 mmHg change in readings.
For the reading to be accurate, the blood pressure cuff therefore needs to be at the same height as your heart.
You may be thinking: “my heart is bigger than an inch; do I aim for the middle?”
And the answer is: ideally the cuff should be at the same height as the right atrium of the heart, which is under the midpoint of the sternum.
However, your arm needs to be supported at that height, because if you have to keep it there using your own power, that will mean a tensing of your muscles, and increase in both heart rate and blood pressure. In fact, studies cited in the video found:
- Unsupported arm, in healthy patients → Systolic +8 mmHg, Diastolic +7 mmHg.
- Unsupported arm, in high blood pressure patients → Systolic +23 mmHg, Diastolic +10 mmHg.
Some other considerations; firstly, correct sitting posture:
- Sit upright with back support
- Feet flat on the floor, legs uncrossed
- Arm should be outward from the body and, as per the above explanation, supported (armrest, table, etc.)
And finally, you should be relaxed and at rest.
For example, your writer here is due for a regular checkup in a couple of weeks, and usually when I go there, I will have walked a couple of miles to get there, then bounced cheerfully up 6 flights of stairs. However, for this appointment, I will need to make sure to arrive early, so that I have time for my (so far as I know, happy and healthy) heart to return to its resting pulse and blood pressure.
Also, if you are anything like this writer, the blood pressure cuff activating is not a relaxing experience (and so invites a higher pulse and blood pressure), so it’s better to take three readings and then discard the first one, and record the average of the second two (I do it this way at home).
Similarly, if a medical environment in general is stressful for you, then taking two minutes to do a little mindfulness meditation, or even just breathing exercises, can be good.
For more on all of these, plus also comments on issues such as correct cuff size and tightness, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Common Hospital Blood Pressure Mistake (Don’t Let This Happen To You Or A Loved One)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is Cutting Calories The Key To Healthy Long Life?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Caloric Restriction with Optimal Nutrition
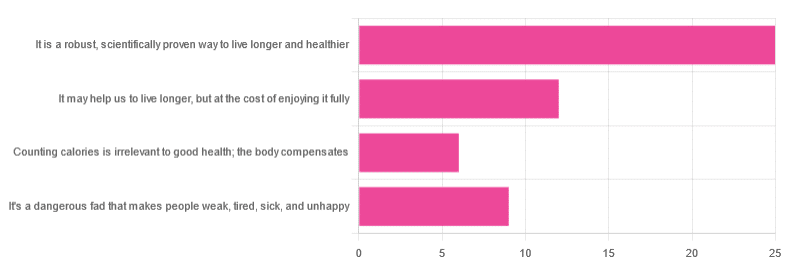
Yesterday, we asked you “What is your opinion of caloric restriction as a health practice?” and got the above-depicted, below-described spread of responses:
- 48% said “It is a robust, scientifically proven way to live longer and healthier”
- 23% said “It may help us to live longer, but at the cost of enjoying it fully”
- 17% said “It’s a dangerous fad that makes people weak, tired, sick, and unhealthy”
- 12% said “Counting calories is irrelevant to good health; the body compensates”
So… What does the science say?
A note on terms, first
“Caloric restriction” (henceforth: CR), as a term, sees scientific use to mean anything from a 25% reduction to a 50% reduction, compared to metabolic base rate.
This can also be expressed the other way around, “dropping to 60% of the metabolic base rate” (i.e., a 40% reduction).
Here we don’t have the space to go into much depth, so our policy will be: if research papers consider it CR, then so will we.
A quick spoiler, first
The above statements about CR are all to at least some degree True in one way or another.
However, there are very important distinctions, so let’s press on…
CR is a robust, scientifically proven way to live longer and healthier: True or False?
True! This has been well-studied and well-documented. There’s more science for this than we could possibly list here, but here’s a good starting point:
❝Calorie restriction (CR), a nutritional intervention of reduced energy intake but with adequate nutrition, has been shown to extend healthspan and lifespan in rodent and primate models.
Accumulating data from observational and randomized clinical trials indicate that CR in humans results in some of the same metabolic and molecular adaptations that have been shown to improve health and retard the accumulation of molecular damage in animal models of longevity.
In particular, moderate CR in humans ameliorates multiple metabolic and hormonal factors that are implicated in the pathogenesis of type 2 diabetes, cardiovascular diseases, and cancer, the leading causes of morbidity, disability and mortality❞
Source: Ageing Research Reviews | Calorie restriction in humans: an update
See also: Caloric restriction in humans reveals immunometabolic regulators of health span
We could devote a whole article (or a whole book, really) to this, but the super-short version is that it lowers the metabolic “tax” on the body and allows the body to function better for longer.
CR may help us to live longer, but at the cost of enjoying it fully: True or False?
True or False, contingently, depending on what’s important to you. And that depends on psychology as much as physiology, but it’s worth noting that there is often a selection bias in the research papers; people ill-suited to CR drop out of the studies and are not counted in the final data.
Also, relevant for a lot of our readers, most (human-based) studies recruit people over 18 and under 60. So while it is reasonable to assume the same benefits will be carried over that age, there is not nearly as much data for it.
Studies into CR and Health-Related Quality of Life (HRQoL) have been promising, and/but have caveats:
❝In non-obese adults, CR had some positive effects and no negative effects on HRQoL.❞
❝We do not know what degree of CR is needed to achieve improvements in HRQoL, but we do know it requires an extraordinary amount of support.
Therefore, the incentive to offer this intervention to a low-risk, normal or overweight individual is lacking and likely not sustainable in practice.❞
CR a dangerous fad that makes people weak, tired, sick, and unhealthy: True or False?
True if it is undertaken improperly, and/or without sufficient support. Many people will try CR and forget that the idea is to reduce metabolic load while still getting good nutrition, and focus solely on the calorie-counting.
So for example, if a person “saves” their calories for the day to have a night out in a bar where they drink their calories as alcohol, then this is going to be abysmal for their health.
That’s an extreme example, but lesser versions are seen a lot. If you save your calories for a pizza instead of a night of alcoholic drinks, then it’s not quite so woeful, but for example the nutrition-to-calorie ratio of pizza is typically not great. Multiply that by doing it as often as not, and yes, someone’s health is going to be in ruins quite soon.
Counting calories is irrelevant to good health; the body compensates: True or False?
True if by “good health” you mean weight loss—which is rarely, if ever, what we mean by “good health” here at 10almonds (unless we clarify such), but it’s a very common association and indeed, for some people it’s a health goal. You cannot sustainably and healthily lose weight by CR alone, especially if you’re not getting optimal nutrition.
Your body will notice that you are starving, and try to save you by storing as much fat as it can, amongst other measures that will similarly backfire (cortisol running high, energy running low, etc).
For short term weight loss though, yes, it’ll work. At a cost. That we don’t recommend.
❝By itself, decreasing calorie intake will have a limited short-term influence.❞
Source: Reducing Calorie Intake May Not Help You Lose Body Weight
See also…
❝Caloric restriction is a commonly recommended weight-loss method, yet it may result in short-term weight loss and subsequent weight regain, known as “weight cycling”, which has recently been shown to be associated with both poor sleep and worse cardiovascular health❞
Source: Dieting Behavior Characterized by Caloric Restriction
In summary…
Caloric restriction is a well-studied area of health science. We know:
- Practised well, it can extend not only lifespan, but also healthspan
- Practised well, it can improve mood, energy, sexual function, and the other things people fear losing
- Practised badly, it can be ruinous to the health—it is critical to practise caloric restriction with optimal nutrition.
- Practised badly, it can lead to unhealthy weight loss and weight regain
One final note…
If you’ve tried CR and hated it, and you practised it well (e.g., with optimal nutrition), then we recommend just not doing it.
You could also try intermittent fasting instead, for similar potential benefits. If that doesn’t work out either, then don’t do that either!
Sometimes, we’re just weird. It can often be because of a genetic or epigenetic quirk. There are usually workarounds, and/but not everything that’s right for most people will be right for all of us.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: